Spotlight
A selection of stories from across the Federation

France, Germany, Poland, United Kingdom, United States, Colombia, India, Tunisia
Abortion Rights: Latest Decisions and Developments around the World
The global landscape of abortion rights continues to evolve in 2024, with new legislation and feminist movements fighting for better access. Let's take a trip around the world to see the latest developments.
Most Popular This Week
France, Germany, Poland, United Kingdom, United States, Colombia, India, Tunisia

Abortion Rights: Latest Decisions and Developments around the World
Over the past 30 years, more than

Palestine

In their own words: The people providing sexual and reproductive health care under bombardment in Gaza
Week after week, heavy Israeli bombardment from air, land, and sea, has continued across most of the Gaza Strip.
Vanuatu

When getting to the hospital is difficult, Vanuatu mobile outreach can save lives
In the mountains of Kumera on Tanna Island, Vanuatu, the village women of Kamahaul normally spend over 10,000 Vatu ($83 USD) to travel to the nearest hospital.
Vanuatu

Sex: changing minds and winning hearts in Tanna, Vanuatu
“Very traditional.” These two words are often used to describe the people of Tanna in Vanuatu, one of the most populated islands in the small country in the Pacific.
Vanuatu

Vanuatu cyclone response: The mental health toll on humanitarian providers
Girls and women from nearby villages flock to mobile health clinics set up by the Vanuatu Family Health Association (VFHA).
Cook Islands

Trans & Proud: Being Transgender in the Cook Islands
It’s a scene like many others around the world: a loving family pour over childhood photos, giggling and reminiscing about the memories.
Cook Islands

In Pictures: The activists who helped win LGBTI+ rights in the Cook Islands
The Cook Islands has removed a law that criminalizes homosexuality, in a huge victory for the local LGBTI+ community.
Filter our stories by:
- Afghanistan
- Albania
- Aruba
- Bangladesh
- Benin
- Botswana
- Burundi
- Cambodia
- (-) Cameroon
- Colombia
- Congo, Dem. Rep.
- Cook Islands
- El Salvador
- Ethiopia
- Fiji
- France
- Germany
- Ghana
- Guinea-Conakry
- India
- Ireland
- Jamaica
- Kenya
- Kiribati
- Lesotho
- Malawi
- Mali
- Mozambique
- Nepal
- Nigeria
- Pakistan
- Palestine
- Poland
- Senegal
- Somaliland
- Sri Lanka
- Sudan
- Thailand
- Togo
- Tonga
- Trinidad and Tobago
- Tunisia
- (-) Uganda
- United Kingdom
- United States
- Vanuatu
- Zambia


| 05 January 2022
In pictures: The changemaker keeping her community healthy and happy
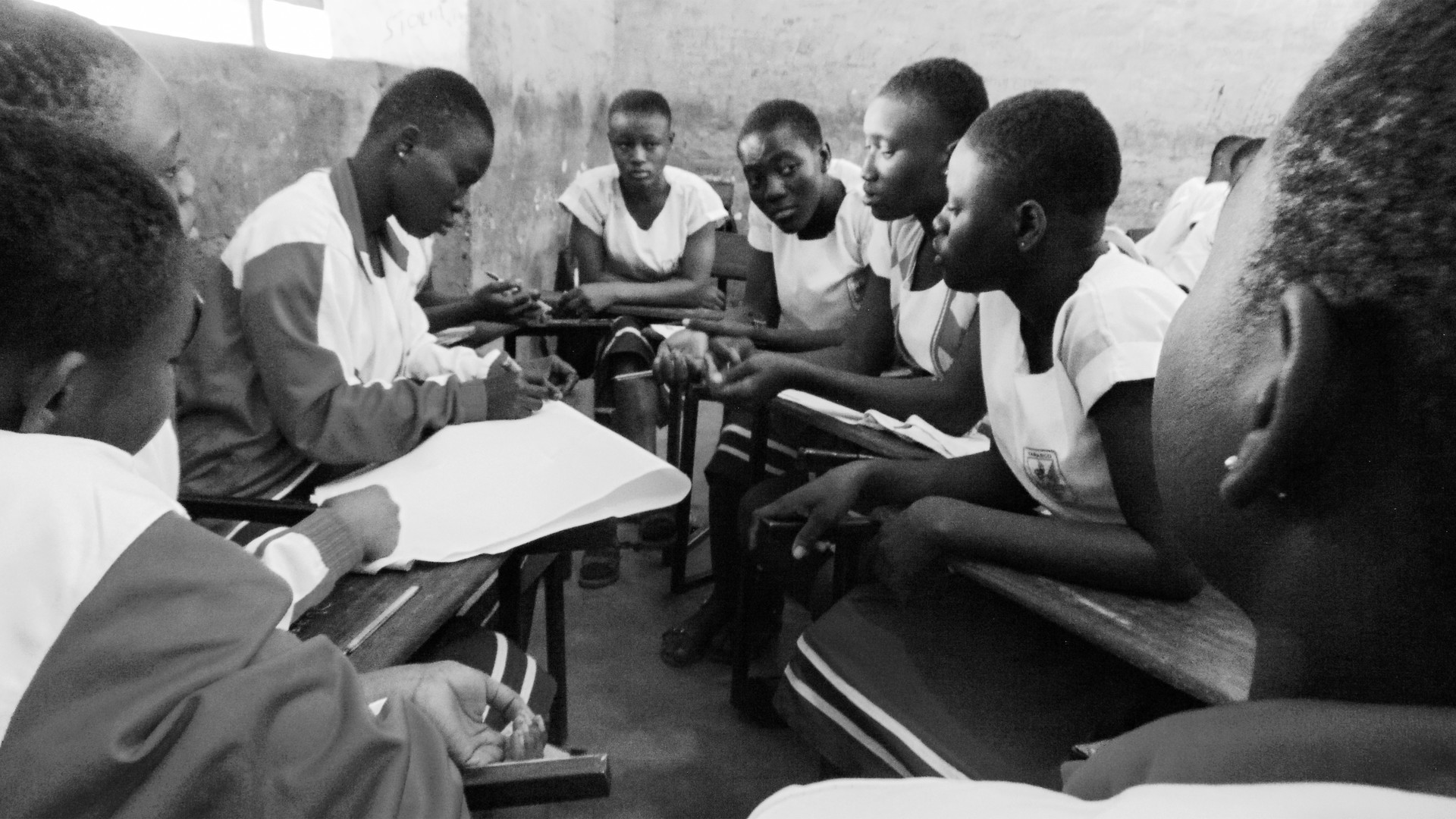
The Get Up, Speak Out! initiative works with and for young people to overcome barriers such as unequal gender norms, negative attitudes towards sexuality, taboos about sex, menstruation, and abortion. Empowering youth communities - especially girls and young women - with information and knowledge about sexual and reproductive health, and the provision of access to health and contraceptive care, is at the heart of the initiative. Get Up, Speak Out! is an international initiative developed by a consortium of partners including IPPF, Rutgers, CHOICE for Youth & Sexuality, Dance4Life, Simavi, and Aidsfonds, with support from the Dutch Ministry of Foreign Affairs.

| 24 April 2024
In pictures: The changemaker keeping her community healthy and happy
The Get Up, Speak Out! initiative works with and for young people to overcome barriers such as unequal gender norms, negative attitudes towards sexuality, taboos about sex, menstruation, and abortion. Empowering youth communities - especially girls and young women - with information and knowledge about sexual and reproductive health, and the provision of access to health and contraceptive care, is at the heart of the initiative. Get Up, Speak Out! is an international initiative developed by a consortium of partners including IPPF, Rutgers, CHOICE for Youth & Sexuality, Dance4Life, Simavi, and Aidsfonds, with support from the Dutch Ministry of Foreign Affairs.

| 23 September 2020
In pictures: Innovating during COVID-19
Women around the world have faced multiple barriers to accessing safe abortion care during the COVID-19 pandemic including the de-prioritization of sexual and reproductive healthcare, overwhelmed health systems and restrictions on movement. The COVID-19 crisis has sparked innovation among IPPF Member Associations who responded swiftly by developing new approaches to reach women with safe abortion care including telemedicine and home-based provision of medical abortion. Strong evidence generated from this work supports the continuation and strengthening of these approaches beyond the end of the pandemic. Cameroon Cameroon National Planning Association for Family Welfare (CAMNAFAW) To ensure that quality abortion care can be provided to women during travel restrictions, CAMNAFAW’s service providers travel to partner clinics in underserved areas and to clients’ homes to provide medical and surgical abortion care. This model of taking safe abortion care closer to women will continue even with easing of travel restrictions, as this has been found to be an effective and acceptable approach to increasing access.Photo: IPPF/Xaume Olleros/Cameroon Share on Twitter Share on Facebook Share via WhatsApp Share via Email Guinea Association Guinéenne pour le Bien-Etre Familial (AGBEF) Building on lessons learned during the Ebola crisis in Guinea, AGBEF quickly took measures to prevent infection in its clinics to continue providing sexual and reproductive healthcare, including surgical and medical abortion, in a safe environment. AGBEF donated protective materials to communities, including hand-washing stations, face masks and antibacterial gel, alongside messaging on infection prevention. This community visibility reassures clients they can safely attend AGBEF clinics for abortion and contraceptive care.Photo: AGBEF/Guinea Share on Twitter Share on Facebook Share via WhatsApp Share via Email India Family Planning Association of India (FPA India) FPA India and partners advocated to have sexual and reproductive healthcare, including abortion, recognized as essential by the government, which meant FPA India could continue healthcare delivery during the national lockdown. To reduce in-person clinic visits, FPA India established teleconsultation and counselling for abortion care, and is continuing to provide in-clinic care for both medical and surgical abortion. Photo: IPPF/Alison Joyce/India Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nepal Family Planning Association of Nepal (FPAN) FPAN and partners advocated for interim approval of home provision of medical abortion and telemedicine for abortion counselling during COVID-19. FPAN is now implementing these approaches, ensuring continued access to abortion care in Nepal, where many people live in remote locations with limited mobility, which has been further restricted by COVID-19 lockdowns. Photo: FPAN/Nepal Share on Twitter Share on Facebook Share via WhatsApp Share via Email Pakistan Rahnuma – Family Planning Association of Pakistan (Rahnuma-FPAP) Rahnuma-FPAP and partners successfully advocated for the government to class sexual and reproductive healthcare as ‘essential’, which enabled the team to continue providing post-abortion care during the pandemic. Rahnuma-FPAP expanded its telemedicine and home-based provision for menstrual regulation counselling and post-abortion care. These new approaches have ensured continued access to services for clients unable to reach clinics.Photo: Rahnuma-FPAP/Pakistan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Palestine Palestinian Family Planning and Protection Association (PFPPA) In response to the government-mandated closure of its clinics, PFPPA quickly established a toll-free call centre which provides consultations, counselling, referrals and follow-up, including consultation for abortion care through a harm reduction approach, ensuring that women are provided with accurate information. Due to its success, PFPPA is exploring options for continuing this healthcare delivery model beyond the pandemic, with the aim of keeping it free of charge for users.Photo: SAAF/Samar Hazboun/Palestine Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sudan Sudan Family Planning Association (SFPA) Following a nation-wide shutdown in April, SFPA established a call centre to increase access to healthcare, including abortion and contraceptive counselling and referrals. An unexpected outcome of the new call centre is that it has reached an increased number of young women who regularly call to discuss their reproductive health and rights. SFPA is working towards institutionalizing this model for continuation beyond the pandemic.Photo: SFPA/Sudan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Togo Association Togolaise pour le Bien-Etre Familial (ATBEF) ATBEF adapted its mobile application ‘Infos Ado Jeunes’, adding a toll-free teleconsultation service for young clients to use to access abortion consultations and pre- and post-abortion counselling. This app has given young clients ongoing access to care when they face challenges travelling to clinics. It has also eased overall client flow in clinics at a time when social distancing is being implemented.Photo: ATBEF/Togo Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 24 April 2024
In pictures: Innovating during COVID-19
Women around the world have faced multiple barriers to accessing safe abortion care during the COVID-19 pandemic including the de-prioritization of sexual and reproductive healthcare, overwhelmed health systems and restrictions on movement. The COVID-19 crisis has sparked innovation among IPPF Member Associations who responded swiftly by developing new approaches to reach women with safe abortion care including telemedicine and home-based provision of medical abortion. Strong evidence generated from this work supports the continuation and strengthening of these approaches beyond the end of the pandemic. Cameroon Cameroon National Planning Association for Family Welfare (CAMNAFAW) To ensure that quality abortion care can be provided to women during travel restrictions, CAMNAFAW’s service providers travel to partner clinics in underserved areas and to clients’ homes to provide medical and surgical abortion care. This model of taking safe abortion care closer to women will continue even with easing of travel restrictions, as this has been found to be an effective and acceptable approach to increasing access.Photo: IPPF/Xaume Olleros/Cameroon Share on Twitter Share on Facebook Share via WhatsApp Share via Email Guinea Association Guinéenne pour le Bien-Etre Familial (AGBEF) Building on lessons learned during the Ebola crisis in Guinea, AGBEF quickly took measures to prevent infection in its clinics to continue providing sexual and reproductive healthcare, including surgical and medical abortion, in a safe environment. AGBEF donated protective materials to communities, including hand-washing stations, face masks and antibacterial gel, alongside messaging on infection prevention. This community visibility reassures clients they can safely attend AGBEF clinics for abortion and contraceptive care.Photo: AGBEF/Guinea Share on Twitter Share on Facebook Share via WhatsApp Share via Email India Family Planning Association of India (FPA India) FPA India and partners advocated to have sexual and reproductive healthcare, including abortion, recognized as essential by the government, which meant FPA India could continue healthcare delivery during the national lockdown. To reduce in-person clinic visits, FPA India established teleconsultation and counselling for abortion care, and is continuing to provide in-clinic care for both medical and surgical abortion. Photo: IPPF/Alison Joyce/India Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nepal Family Planning Association of Nepal (FPAN) FPAN and partners advocated for interim approval of home provision of medical abortion and telemedicine for abortion counselling during COVID-19. FPAN is now implementing these approaches, ensuring continued access to abortion care in Nepal, where many people live in remote locations with limited mobility, which has been further restricted by COVID-19 lockdowns. Photo: FPAN/Nepal Share on Twitter Share on Facebook Share via WhatsApp Share via Email Pakistan Rahnuma – Family Planning Association of Pakistan (Rahnuma-FPAP) Rahnuma-FPAP and partners successfully advocated for the government to class sexual and reproductive healthcare as ‘essential’, which enabled the team to continue providing post-abortion care during the pandemic. Rahnuma-FPAP expanded its telemedicine and home-based provision for menstrual regulation counselling and post-abortion care. These new approaches have ensured continued access to services for clients unable to reach clinics.Photo: Rahnuma-FPAP/Pakistan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Palestine Palestinian Family Planning and Protection Association (PFPPA) In response to the government-mandated closure of its clinics, PFPPA quickly established a toll-free call centre which provides consultations, counselling, referrals and follow-up, including consultation for abortion care through a harm reduction approach, ensuring that women are provided with accurate information. Due to its success, PFPPA is exploring options for continuing this healthcare delivery model beyond the pandemic, with the aim of keeping it free of charge for users.Photo: SAAF/Samar Hazboun/Palestine Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sudan Sudan Family Planning Association (SFPA) Following a nation-wide shutdown in April, SFPA established a call centre to increase access to healthcare, including abortion and contraceptive counselling and referrals. An unexpected outcome of the new call centre is that it has reached an increased number of young women who regularly call to discuss their reproductive health and rights. SFPA is working towards institutionalizing this model for continuation beyond the pandemic.Photo: SFPA/Sudan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Togo Association Togolaise pour le Bien-Etre Familial (ATBEF) ATBEF adapted its mobile application ‘Infos Ado Jeunes’, adding a toll-free teleconsultation service for young clients to use to access abortion consultations and pre- and post-abortion counselling. This app has given young clients ongoing access to care when they face challenges travelling to clinics. It has also eased overall client flow in clinics at a time when social distancing is being implemented.Photo: ATBEF/Togo Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 08 July 2019
"I help to raise awareness of why we have to protect ourselves"
“The first time I met Chariette [a peer educator for the Cameroon National Planning Association for Family Welfare] was at Sunday football, around four years ago. She was invited by the organizer to come and talk to us when the match was over. We were all men but she wasn’t intimidated and she handled the stupid jokes well. We stayed in touch and then one day I realized I had an STI. It’s a little taboo and I didn’t want to talk about it. I bought some drugs at the local market but they didn’t have any effect. I called Chariette and we discussed what had happened. She told me to come to the CAMNAFAW clinic and I did, where I spoke about my problem and they gave me proper drugs to get rid of it. That day, I decided to become a peer educator myself. There are a lot of guys who are suffering but too scared to speak out. Above all, men are scared of talking about STIs. I now work in schools and youth groups, especially sports teams. They will insist they don’t have anything wrong but every Sunday since then I have gone round the teams and chatted with them. I speak about pregnancy as well. It’s the guys who push women to have sex without a condom and also to have an abortion afterwards. I help to raise awareness of why we have to protect ourselves. It’s hard to recruit people to become peer educators because we are volunteers. It’s not easy to persuade people to change their ways. The view from a lot of churches is very strict and centers on abstinence. The young men want to be macho.” Hervé Tchuigwa Djiya is a peer educator for the Cameroon National Planning Association for Family Welfare (CAMNAFAW)

| 24 April 2024
"I help to raise awareness of why we have to protect ourselves"
“The first time I met Chariette [a peer educator for the Cameroon National Planning Association for Family Welfare] was at Sunday football, around four years ago. She was invited by the organizer to come and talk to us when the match was over. We were all men but she wasn’t intimidated and she handled the stupid jokes well. We stayed in touch and then one day I realized I had an STI. It’s a little taboo and I didn’t want to talk about it. I bought some drugs at the local market but they didn’t have any effect. I called Chariette and we discussed what had happened. She told me to come to the CAMNAFAW clinic and I did, where I spoke about my problem and they gave me proper drugs to get rid of it. That day, I decided to become a peer educator myself. There are a lot of guys who are suffering but too scared to speak out. Above all, men are scared of talking about STIs. I now work in schools and youth groups, especially sports teams. They will insist they don’t have anything wrong but every Sunday since then I have gone round the teams and chatted with them. I speak about pregnancy as well. It’s the guys who push women to have sex without a condom and also to have an abortion afterwards. I help to raise awareness of why we have to protect ourselves. It’s hard to recruit people to become peer educators because we are volunteers. It’s not easy to persuade people to change their ways. The view from a lot of churches is very strict and centers on abstinence. The young men want to be macho.” Hervé Tchuigwa Djiya is a peer educator for the Cameroon National Planning Association for Family Welfare (CAMNAFAW)

| 08 July 2019
"I have brothers and I have helped them to change too. I’ve helped them to adopt a healthier sex life"
“Chariette was my neighbor. We lived next door to each other. She often organized group information sessions in the neighbourhood to talk about sexually transmitted infections (STIs) and early pregnancy, and unintended pregnancies as well. When I started attending her sessions I was in a bit of unstable relationship. My life was chaotic. My boyfriend didn’t like using protection and we told each other that as we loved each other we weren’t taking any risks. Once I caught something and I was itching a lot. My boyfriend told me that I must have caught it in a public toilet. I trusted him and I didn’t realize I could catch something. When I started listening to Chariette it opened my eyes and I realized I was running big risks. As we aren’t married and we are still studying, we shouldn’t have an unintended pregnancy. What would we do? She told me about sexually transmitted infections as well. I tried to talk to my boyfriend about it but he didn’t want to hear about it, especially about using condoms. I asked for a private session with Chariette for him, and she spoke to us both and he finally understood. Today we have a much more stable sex life and we aren’t running those risks anymore. He learned how to use a condom. After attending her sessions, I was able to save a friend with Chariette’s help. This friend tried to perform an abortion herself and she was bleeding everywhere. I remembered that Chariette told me about the Cameroon National Planning Association for Family Welfare clinic, so I called her and asked how she could be admitted. She was able to receive post-abortion care but if I hadn’t known Chariette I don’t know what would have happened. I have brothers and I have helped them to change too. I’ve helped them to adopt a healthier sex life. There is HIV around and it’s scary.” Gertrude Zouakeu Noutcha, 29, is a student and peer educator for the Cameroon National Planning Association for Family Welfare (CAMNAFAW)

| 24 April 2024
"I have brothers and I have helped them to change too. I’ve helped them to adopt a healthier sex life"
“Chariette was my neighbor. We lived next door to each other. She often organized group information sessions in the neighbourhood to talk about sexually transmitted infections (STIs) and early pregnancy, and unintended pregnancies as well. When I started attending her sessions I was in a bit of unstable relationship. My life was chaotic. My boyfriend didn’t like using protection and we told each other that as we loved each other we weren’t taking any risks. Once I caught something and I was itching a lot. My boyfriend told me that I must have caught it in a public toilet. I trusted him and I didn’t realize I could catch something. When I started listening to Chariette it opened my eyes and I realized I was running big risks. As we aren’t married and we are still studying, we shouldn’t have an unintended pregnancy. What would we do? She told me about sexually transmitted infections as well. I tried to talk to my boyfriend about it but he didn’t want to hear about it, especially about using condoms. I asked for a private session with Chariette for him, and she spoke to us both and he finally understood. Today we have a much more stable sex life and we aren’t running those risks anymore. He learned how to use a condom. After attending her sessions, I was able to save a friend with Chariette’s help. This friend tried to perform an abortion herself and she was bleeding everywhere. I remembered that Chariette told me about the Cameroon National Planning Association for Family Welfare clinic, so I called her and asked how she could be admitted. She was able to receive post-abortion care but if I hadn’t known Chariette I don’t know what would have happened. I have brothers and I have helped them to change too. I’ve helped them to adopt a healthier sex life. There is HIV around and it’s scary.” Gertrude Zouakeu Noutcha, 29, is a student and peer educator for the Cameroon National Planning Association for Family Welfare (CAMNAFAW)
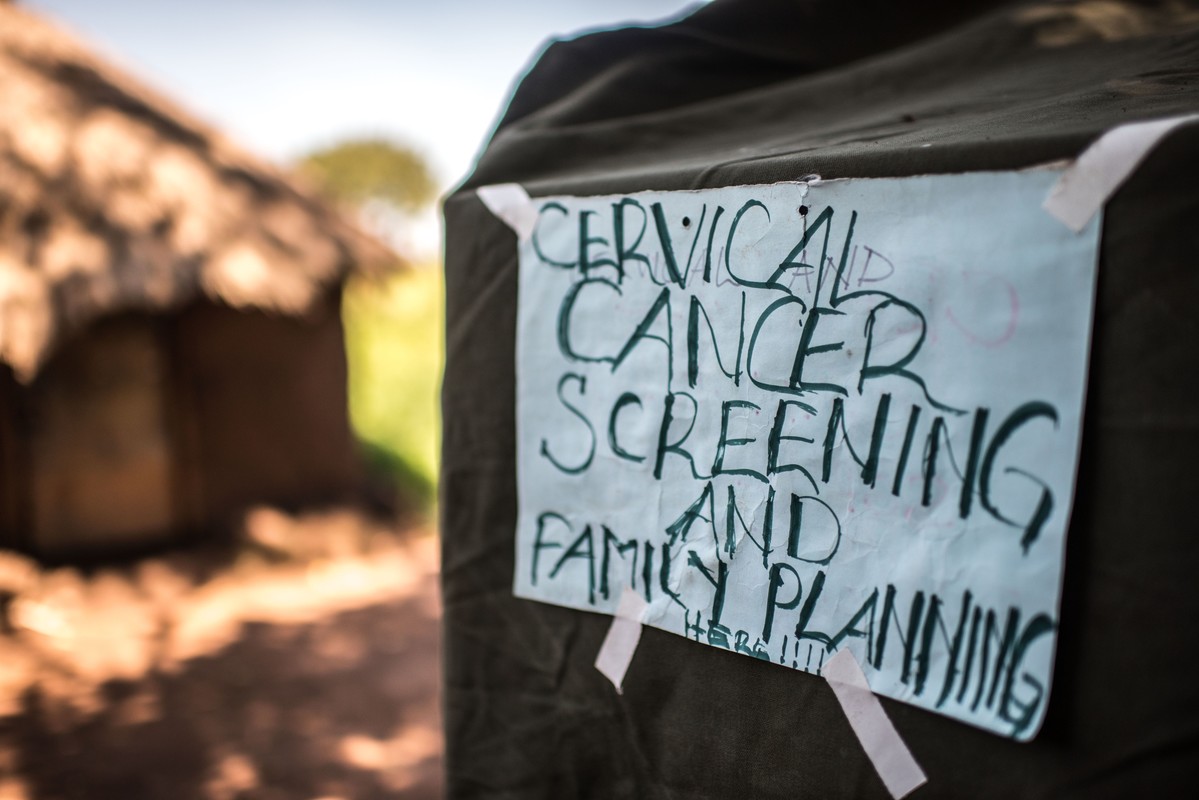
| 22 August 2018
“A radio announcement saved my life” – Gertrude’s story
Gertrude Mugala is a teacher in Fort Portal, a town in Western Uganda. While Gertrude considered herself fairly knowledgeable about cancer, she had never considered taking a screening test or imagined herself ever having the disease. Then one day, she heard an announcement on the radio urging women to go for cervical cancer screenings at a Reproductive Health Uganda (RHU) clinic. “The radio presenter was talking about cervical cancer, and in her message she encouraged all women to get screened. I decided to go and try it out,” she said. Gertrude made her way to RHU's Fort Portal Branch clinic for the free cervical cancer screening. There, she met Ms. Irene Kugonza, an RHU service provider. Ms. Kugonza educated Gertrude and a group of other women about cervical cancer and the importance of routine screening. Gertrude received a type of cervical cancer screening called VIA (visual inspection with acetic acid). "I did not know what was happening" But Gertrude's results were not what she expected; she received a positive result. The good news, however, is that precancerous lesions can be treated if detected early. “I was so shaken when I was told I had pre-cancerous lesions. I did not know what was happening and I didn't believe what I was hearing. I had no idea of my health status. I thought I was healthy, but I was actually harbouring a potential killer disease in me. What would have happened if I didn't go for the screening? If I hadn't heard the radio announcement?” Gertrude was then referred for cryotherapy. “Following cryotherapy, I am now in the process of healing, and I am supposed to go back for review after three months,” said Gertrude. Community screenings Today, Gertrude advocates for cervical cancer screening in her community. She talks to women about cancer, especially cervical cancer, at her workplace, at the market, in meetings, and any other opportunity she gets. “I decided to let women know that cervical cancer is real and it is here with us, and that it kills. At the moment, those are the platforms I have, and I will continue educating women about cancer and encourage them to go for routine testing. I am also happy that I was near my radio that day, where I heard that announcement encouraging all women to get tested for cervical cancer. It might be because of that radio announcement that I am here today,” she said.
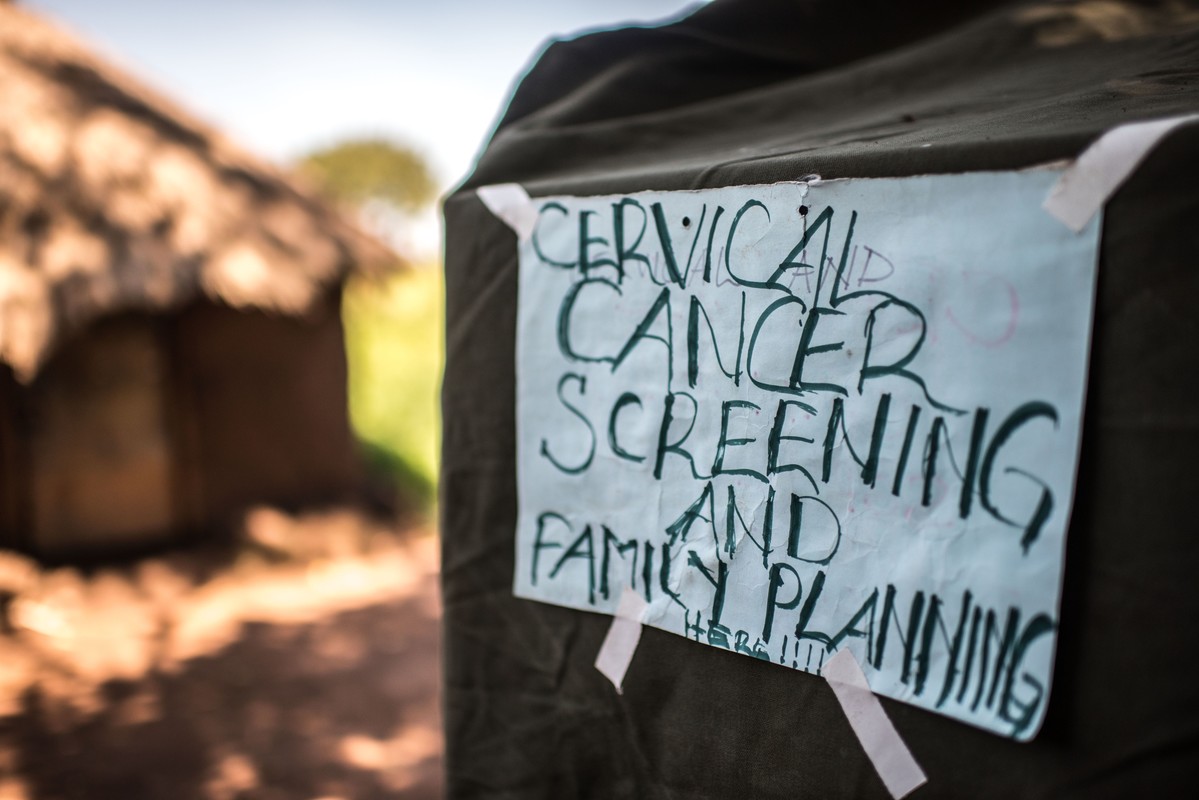
| 24 April 2024
“A radio announcement saved my life” – Gertrude’s story
Gertrude Mugala is a teacher in Fort Portal, a town in Western Uganda. While Gertrude considered herself fairly knowledgeable about cancer, she had never considered taking a screening test or imagined herself ever having the disease. Then one day, she heard an announcement on the radio urging women to go for cervical cancer screenings at a Reproductive Health Uganda (RHU) clinic. “The radio presenter was talking about cervical cancer, and in her message she encouraged all women to get screened. I decided to go and try it out,” she said. Gertrude made her way to RHU's Fort Portal Branch clinic for the free cervical cancer screening. There, she met Ms. Irene Kugonza, an RHU service provider. Ms. Kugonza educated Gertrude and a group of other women about cervical cancer and the importance of routine screening. Gertrude received a type of cervical cancer screening called VIA (visual inspection with acetic acid). "I did not know what was happening" But Gertrude's results were not what she expected; she received a positive result. The good news, however, is that precancerous lesions can be treated if detected early. “I was so shaken when I was told I had pre-cancerous lesions. I did not know what was happening and I didn't believe what I was hearing. I had no idea of my health status. I thought I was healthy, but I was actually harbouring a potential killer disease in me. What would have happened if I didn't go for the screening? If I hadn't heard the radio announcement?” Gertrude was then referred for cryotherapy. “Following cryotherapy, I am now in the process of healing, and I am supposed to go back for review after three months,” said Gertrude. Community screenings Today, Gertrude advocates for cervical cancer screening in her community. She talks to women about cancer, especially cervical cancer, at her workplace, at the market, in meetings, and any other opportunity she gets. “I decided to let women know that cervical cancer is real and it is here with us, and that it kills. At the moment, those are the platforms I have, and I will continue educating women about cancer and encourage them to go for routine testing. I am also happy that I was near my radio that day, where I heard that announcement encouraging all women to get tested for cervical cancer. It might be because of that radio announcement that I am here today,” she said.

| 21 May 2017
A graduate in need turns to sex work
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Lady Mermaid's Bureau. I am Pretty Lynn, aged 25. I am a sex worker but I went to university. I graduated with a Bachelor's Degree in Tourism in 2013. But now, during the day I’m sleeping and during the night I’m working. That is how my day goes every day. I got into sex work through friends. Okay it is not good but I am earning. I tried to get a job when I graduated. I have been applying since I graduated in 2013. I’m still applying but I’m not getting anywhere. You know to get jobs in Uganda; you have to know someone there and no one knows me there. To be a sex worker is like a curse. People look at you like, I don’t know, as someone that has no use in society. People look at you in a bad way. They even don’t consider why you are selling. They just see you as the worst thing that can happen in the society. So it is not comfortable, it is really hard but we try and survive. The fact sex working is illegal means you have to hide yourself when you are selling so that police cannot take you. And then you get diseases, men don’t want to pay. When the police come and take us, sometimes they even use us and don’t pay. So it is really hard. They want a free service. Like if they come and take you and pay that would be fair. But they say it is illegal to sell yourself. But they still use you yet they are saying it is illegal. You can’t report the police because there is no evidence. Abortion and unwanted pregnancies are really common because men don’t want to use condoms and female condoms are really rare and they are expensive. Though at times we get female condoms from Lady Marmaid’s Bureau (LMB) because there are so many of us they can’t keep on giving you them all the time. At times when we get pregnant we use local methods. You can go and use local herbs but it is not safe. One time I used local herbs and I was successful. Then the other time I used Omo washing powder and tea leaves but it was really hard for me. I almost died. I had a friend who died last year from this. But the good thing is that LMB taught us about safe abortion. I have had a safe abortion too. There are some tabs they are called Miso (misoprostol). It costs about fifty thousand shillings (£10 pounds or $20.) It is a lot of money. But if I’m working and I know I’m pregnant, I can say, "this week I’m working for my safe abortion". So if I’m working for twenty thousand, by the end of the week I will have the money. It is expensive compared to Omo at five hundred shillings but that is risky. So if I say I will work this whole week for Miso (misoprostol) it is better. But I'm working and I'm not eating. A project like this one from Lady Mermaid's can help young girls and women. But to take us from sex work, it would really be hard. They would not have enough money to cater for all of us. So what they have to do is to teach us how to protect ourselves, how to defend ourselves. Safe abortion yes. They will just have to sensitise us more about our lives, protection, female condoms and all that. I don't have a boyfriend but maybe when I get money and leave this job I will. But for now, no man would like a woman who sells. No man will bear the wife selling herself. And that will happen only if I get funds, settle somewhere else and become responsible woman. I don’t want this job. I don’t want to be in this business of sex work all the time. I want be married, with my children happily, not selling myself. Stories Read more stories about the amazing success of SAAF in Uganda

| 24 April 2024
A graduate in need turns to sex work
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Lady Mermaid's Bureau. I am Pretty Lynn, aged 25. I am a sex worker but I went to university. I graduated with a Bachelor's Degree in Tourism in 2013. But now, during the day I’m sleeping and during the night I’m working. That is how my day goes every day. I got into sex work through friends. Okay it is not good but I am earning. I tried to get a job when I graduated. I have been applying since I graduated in 2013. I’m still applying but I’m not getting anywhere. You know to get jobs in Uganda; you have to know someone there and no one knows me there. To be a sex worker is like a curse. People look at you like, I don’t know, as someone that has no use in society. People look at you in a bad way. They even don’t consider why you are selling. They just see you as the worst thing that can happen in the society. So it is not comfortable, it is really hard but we try and survive. The fact sex working is illegal means you have to hide yourself when you are selling so that police cannot take you. And then you get diseases, men don’t want to pay. When the police come and take us, sometimes they even use us and don’t pay. So it is really hard. They want a free service. Like if they come and take you and pay that would be fair. But they say it is illegal to sell yourself. But they still use you yet they are saying it is illegal. You can’t report the police because there is no evidence. Abortion and unwanted pregnancies are really common because men don’t want to use condoms and female condoms are really rare and they are expensive. Though at times we get female condoms from Lady Marmaid’s Bureau (LMB) because there are so many of us they can’t keep on giving you them all the time. At times when we get pregnant we use local methods. You can go and use local herbs but it is not safe. One time I used local herbs and I was successful. Then the other time I used Omo washing powder and tea leaves but it was really hard for me. I almost died. I had a friend who died last year from this. But the good thing is that LMB taught us about safe abortion. I have had a safe abortion too. There are some tabs they are called Miso (misoprostol). It costs about fifty thousand shillings (£10 pounds or $20.) It is a lot of money. But if I’m working and I know I’m pregnant, I can say, "this week I’m working for my safe abortion". So if I’m working for twenty thousand, by the end of the week I will have the money. It is expensive compared to Omo at five hundred shillings but that is risky. So if I say I will work this whole week for Miso (misoprostol) it is better. But I'm working and I'm not eating. A project like this one from Lady Mermaid's can help young girls and women. But to take us from sex work, it would really be hard. They would not have enough money to cater for all of us. So what they have to do is to teach us how to protect ourselves, how to defend ourselves. Safe abortion yes. They will just have to sensitise us more about our lives, protection, female condoms and all that. I don't have a boyfriend but maybe when I get money and leave this job I will. But for now, no man would like a woman who sells. No man will bear the wife selling herself. And that will happen only if I get funds, settle somewhere else and become responsible woman. I don’t want this job. I don’t want to be in this business of sex work all the time. I want be married, with my children happily, not selling myself. Stories Read more stories about the amazing success of SAAF in Uganda

| 05 January 2022
In pictures: The changemaker keeping her community healthy and happy
The Get Up, Speak Out! initiative works with and for young people to overcome barriers such as unequal gender norms, negative attitudes towards sexuality, taboos about sex, menstruation, and abortion. Empowering youth communities - especially girls and young women - with information and knowledge about sexual and reproductive health, and the provision of access to health and contraceptive care, is at the heart of the initiative. Get Up, Speak Out! is an international initiative developed by a consortium of partners including IPPF, Rutgers, CHOICE for Youth & Sexuality, Dance4Life, Simavi, and Aidsfonds, with support from the Dutch Ministry of Foreign Affairs.

| 24 April 2024
In pictures: The changemaker keeping her community healthy and happy
The Get Up, Speak Out! initiative works with and for young people to overcome barriers such as unequal gender norms, negative attitudes towards sexuality, taboos about sex, menstruation, and abortion. Empowering youth communities - especially girls and young women - with information and knowledge about sexual and reproductive health, and the provision of access to health and contraceptive care, is at the heart of the initiative. Get Up, Speak Out! is an international initiative developed by a consortium of partners including IPPF, Rutgers, CHOICE for Youth & Sexuality, Dance4Life, Simavi, and Aidsfonds, with support from the Dutch Ministry of Foreign Affairs.

| 23 September 2020
In pictures: Innovating during COVID-19
Women around the world have faced multiple barriers to accessing safe abortion care during the COVID-19 pandemic including the de-prioritization of sexual and reproductive healthcare, overwhelmed health systems and restrictions on movement. The COVID-19 crisis has sparked innovation among IPPF Member Associations who responded swiftly by developing new approaches to reach women with safe abortion care including telemedicine and home-based provision of medical abortion. Strong evidence generated from this work supports the continuation and strengthening of these approaches beyond the end of the pandemic. Cameroon Cameroon National Planning Association for Family Welfare (CAMNAFAW) To ensure that quality abortion care can be provided to women during travel restrictions, CAMNAFAW’s service providers travel to partner clinics in underserved areas and to clients’ homes to provide medical and surgical abortion care. This model of taking safe abortion care closer to women will continue even with easing of travel restrictions, as this has been found to be an effective and acceptable approach to increasing access.Photo: IPPF/Xaume Olleros/Cameroon Share on Twitter Share on Facebook Share via WhatsApp Share via Email Guinea Association Guinéenne pour le Bien-Etre Familial (AGBEF) Building on lessons learned during the Ebola crisis in Guinea, AGBEF quickly took measures to prevent infection in its clinics to continue providing sexual and reproductive healthcare, including surgical and medical abortion, in a safe environment. AGBEF donated protective materials to communities, including hand-washing stations, face masks and antibacterial gel, alongside messaging on infection prevention. This community visibility reassures clients they can safely attend AGBEF clinics for abortion and contraceptive care.Photo: AGBEF/Guinea Share on Twitter Share on Facebook Share via WhatsApp Share via Email India Family Planning Association of India (FPA India) FPA India and partners advocated to have sexual and reproductive healthcare, including abortion, recognized as essential by the government, which meant FPA India could continue healthcare delivery during the national lockdown. To reduce in-person clinic visits, FPA India established teleconsultation and counselling for abortion care, and is continuing to provide in-clinic care for both medical and surgical abortion. Photo: IPPF/Alison Joyce/India Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nepal Family Planning Association of Nepal (FPAN) FPAN and partners advocated for interim approval of home provision of medical abortion and telemedicine for abortion counselling during COVID-19. FPAN is now implementing these approaches, ensuring continued access to abortion care in Nepal, where many people live in remote locations with limited mobility, which has been further restricted by COVID-19 lockdowns. Photo: FPAN/Nepal Share on Twitter Share on Facebook Share via WhatsApp Share via Email Pakistan Rahnuma – Family Planning Association of Pakistan (Rahnuma-FPAP) Rahnuma-FPAP and partners successfully advocated for the government to class sexual and reproductive healthcare as ‘essential’, which enabled the team to continue providing post-abortion care during the pandemic. Rahnuma-FPAP expanded its telemedicine and home-based provision for menstrual regulation counselling and post-abortion care. These new approaches have ensured continued access to services for clients unable to reach clinics.Photo: Rahnuma-FPAP/Pakistan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Palestine Palestinian Family Planning and Protection Association (PFPPA) In response to the government-mandated closure of its clinics, PFPPA quickly established a toll-free call centre which provides consultations, counselling, referrals and follow-up, including consultation for abortion care through a harm reduction approach, ensuring that women are provided with accurate information. Due to its success, PFPPA is exploring options for continuing this healthcare delivery model beyond the pandemic, with the aim of keeping it free of charge for users.Photo: SAAF/Samar Hazboun/Palestine Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sudan Sudan Family Planning Association (SFPA) Following a nation-wide shutdown in April, SFPA established a call centre to increase access to healthcare, including abortion and contraceptive counselling and referrals. An unexpected outcome of the new call centre is that it has reached an increased number of young women who regularly call to discuss their reproductive health and rights. SFPA is working towards institutionalizing this model for continuation beyond the pandemic.Photo: SFPA/Sudan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Togo Association Togolaise pour le Bien-Etre Familial (ATBEF) ATBEF adapted its mobile application ‘Infos Ado Jeunes’, adding a toll-free teleconsultation service for young clients to use to access abortion consultations and pre- and post-abortion counselling. This app has given young clients ongoing access to care when they face challenges travelling to clinics. It has also eased overall client flow in clinics at a time when social distancing is being implemented.Photo: ATBEF/Togo Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 24 April 2024
In pictures: Innovating during COVID-19
Women around the world have faced multiple barriers to accessing safe abortion care during the COVID-19 pandemic including the de-prioritization of sexual and reproductive healthcare, overwhelmed health systems and restrictions on movement. The COVID-19 crisis has sparked innovation among IPPF Member Associations who responded swiftly by developing new approaches to reach women with safe abortion care including telemedicine and home-based provision of medical abortion. Strong evidence generated from this work supports the continuation and strengthening of these approaches beyond the end of the pandemic. Cameroon Cameroon National Planning Association for Family Welfare (CAMNAFAW) To ensure that quality abortion care can be provided to women during travel restrictions, CAMNAFAW’s service providers travel to partner clinics in underserved areas and to clients’ homes to provide medical and surgical abortion care. This model of taking safe abortion care closer to women will continue even with easing of travel restrictions, as this has been found to be an effective and acceptable approach to increasing access.Photo: IPPF/Xaume Olleros/Cameroon Share on Twitter Share on Facebook Share via WhatsApp Share via Email Guinea Association Guinéenne pour le Bien-Etre Familial (AGBEF) Building on lessons learned during the Ebola crisis in Guinea, AGBEF quickly took measures to prevent infection in its clinics to continue providing sexual and reproductive healthcare, including surgical and medical abortion, in a safe environment. AGBEF donated protective materials to communities, including hand-washing stations, face masks and antibacterial gel, alongside messaging on infection prevention. This community visibility reassures clients they can safely attend AGBEF clinics for abortion and contraceptive care.Photo: AGBEF/Guinea Share on Twitter Share on Facebook Share via WhatsApp Share via Email India Family Planning Association of India (FPA India) FPA India and partners advocated to have sexual and reproductive healthcare, including abortion, recognized as essential by the government, which meant FPA India could continue healthcare delivery during the national lockdown. To reduce in-person clinic visits, FPA India established teleconsultation and counselling for abortion care, and is continuing to provide in-clinic care for both medical and surgical abortion. Photo: IPPF/Alison Joyce/India Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nepal Family Planning Association of Nepal (FPAN) FPAN and partners advocated for interim approval of home provision of medical abortion and telemedicine for abortion counselling during COVID-19. FPAN is now implementing these approaches, ensuring continued access to abortion care in Nepal, where many people live in remote locations with limited mobility, which has been further restricted by COVID-19 lockdowns. Photo: FPAN/Nepal Share on Twitter Share on Facebook Share via WhatsApp Share via Email Pakistan Rahnuma – Family Planning Association of Pakistan (Rahnuma-FPAP) Rahnuma-FPAP and partners successfully advocated for the government to class sexual and reproductive healthcare as ‘essential’, which enabled the team to continue providing post-abortion care during the pandemic. Rahnuma-FPAP expanded its telemedicine and home-based provision for menstrual regulation counselling and post-abortion care. These new approaches have ensured continued access to services for clients unable to reach clinics.Photo: Rahnuma-FPAP/Pakistan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Palestine Palestinian Family Planning and Protection Association (PFPPA) In response to the government-mandated closure of its clinics, PFPPA quickly established a toll-free call centre which provides consultations, counselling, referrals and follow-up, including consultation for abortion care through a harm reduction approach, ensuring that women are provided with accurate information. Due to its success, PFPPA is exploring options for continuing this healthcare delivery model beyond the pandemic, with the aim of keeping it free of charge for users.Photo: SAAF/Samar Hazboun/Palestine Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sudan Sudan Family Planning Association (SFPA) Following a nation-wide shutdown in April, SFPA established a call centre to increase access to healthcare, including abortion and contraceptive counselling and referrals. An unexpected outcome of the new call centre is that it has reached an increased number of young women who regularly call to discuss their reproductive health and rights. SFPA is working towards institutionalizing this model for continuation beyond the pandemic.Photo: SFPA/Sudan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Togo Association Togolaise pour le Bien-Etre Familial (ATBEF) ATBEF adapted its mobile application ‘Infos Ado Jeunes’, adding a toll-free teleconsultation service for young clients to use to access abortion consultations and pre- and post-abortion counselling. This app has given young clients ongoing access to care when they face challenges travelling to clinics. It has also eased overall client flow in clinics at a time when social distancing is being implemented.Photo: ATBEF/Togo Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 08 July 2019
"I help to raise awareness of why we have to protect ourselves"
“The first time I met Chariette [a peer educator for the Cameroon National Planning Association for Family Welfare] was at Sunday football, around four years ago. She was invited by the organizer to come and talk to us when the match was over. We were all men but she wasn’t intimidated and she handled the stupid jokes well. We stayed in touch and then one day I realized I had an STI. It’s a little taboo and I didn’t want to talk about it. I bought some drugs at the local market but they didn’t have any effect. I called Chariette and we discussed what had happened. She told me to come to the CAMNAFAW clinic and I did, where I spoke about my problem and they gave me proper drugs to get rid of it. That day, I decided to become a peer educator myself. There are a lot of guys who are suffering but too scared to speak out. Above all, men are scared of talking about STIs. I now work in schools and youth groups, especially sports teams. They will insist they don’t have anything wrong but every Sunday since then I have gone round the teams and chatted with them. I speak about pregnancy as well. It’s the guys who push women to have sex without a condom and also to have an abortion afterwards. I help to raise awareness of why we have to protect ourselves. It’s hard to recruit people to become peer educators because we are volunteers. It’s not easy to persuade people to change their ways. The view from a lot of churches is very strict and centers on abstinence. The young men want to be macho.” Hervé Tchuigwa Djiya is a peer educator for the Cameroon National Planning Association for Family Welfare (CAMNAFAW)

| 24 April 2024
"I help to raise awareness of why we have to protect ourselves"
“The first time I met Chariette [a peer educator for the Cameroon National Planning Association for Family Welfare] was at Sunday football, around four years ago. She was invited by the organizer to come and talk to us when the match was over. We were all men but she wasn’t intimidated and she handled the stupid jokes well. We stayed in touch and then one day I realized I had an STI. It’s a little taboo and I didn’t want to talk about it. I bought some drugs at the local market but they didn’t have any effect. I called Chariette and we discussed what had happened. She told me to come to the CAMNAFAW clinic and I did, where I spoke about my problem and they gave me proper drugs to get rid of it. That day, I decided to become a peer educator myself. There are a lot of guys who are suffering but too scared to speak out. Above all, men are scared of talking about STIs. I now work in schools and youth groups, especially sports teams. They will insist they don’t have anything wrong but every Sunday since then I have gone round the teams and chatted with them. I speak about pregnancy as well. It’s the guys who push women to have sex without a condom and also to have an abortion afterwards. I help to raise awareness of why we have to protect ourselves. It’s hard to recruit people to become peer educators because we are volunteers. It’s not easy to persuade people to change their ways. The view from a lot of churches is very strict and centers on abstinence. The young men want to be macho.” Hervé Tchuigwa Djiya is a peer educator for the Cameroon National Planning Association for Family Welfare (CAMNAFAW)

| 08 July 2019
"I have brothers and I have helped them to change too. I’ve helped them to adopt a healthier sex life"
“Chariette was my neighbor. We lived next door to each other. She often organized group information sessions in the neighbourhood to talk about sexually transmitted infections (STIs) and early pregnancy, and unintended pregnancies as well. When I started attending her sessions I was in a bit of unstable relationship. My life was chaotic. My boyfriend didn’t like using protection and we told each other that as we loved each other we weren’t taking any risks. Once I caught something and I was itching a lot. My boyfriend told me that I must have caught it in a public toilet. I trusted him and I didn’t realize I could catch something. When I started listening to Chariette it opened my eyes and I realized I was running big risks. As we aren’t married and we are still studying, we shouldn’t have an unintended pregnancy. What would we do? She told me about sexually transmitted infections as well. I tried to talk to my boyfriend about it but he didn’t want to hear about it, especially about using condoms. I asked for a private session with Chariette for him, and she spoke to us both and he finally understood. Today we have a much more stable sex life and we aren’t running those risks anymore. He learned how to use a condom. After attending her sessions, I was able to save a friend with Chariette’s help. This friend tried to perform an abortion herself and she was bleeding everywhere. I remembered that Chariette told me about the Cameroon National Planning Association for Family Welfare clinic, so I called her and asked how she could be admitted. She was able to receive post-abortion care but if I hadn’t known Chariette I don’t know what would have happened. I have brothers and I have helped them to change too. I’ve helped them to adopt a healthier sex life. There is HIV around and it’s scary.” Gertrude Zouakeu Noutcha, 29, is a student and peer educator for the Cameroon National Planning Association for Family Welfare (CAMNAFAW)

| 24 April 2024
"I have brothers and I have helped them to change too. I’ve helped them to adopt a healthier sex life"
“Chariette was my neighbor. We lived next door to each other. She often organized group information sessions in the neighbourhood to talk about sexually transmitted infections (STIs) and early pregnancy, and unintended pregnancies as well. When I started attending her sessions I was in a bit of unstable relationship. My life was chaotic. My boyfriend didn’t like using protection and we told each other that as we loved each other we weren’t taking any risks. Once I caught something and I was itching a lot. My boyfriend told me that I must have caught it in a public toilet. I trusted him and I didn’t realize I could catch something. When I started listening to Chariette it opened my eyes and I realized I was running big risks. As we aren’t married and we are still studying, we shouldn’t have an unintended pregnancy. What would we do? She told me about sexually transmitted infections as well. I tried to talk to my boyfriend about it but he didn’t want to hear about it, especially about using condoms. I asked for a private session with Chariette for him, and she spoke to us both and he finally understood. Today we have a much more stable sex life and we aren’t running those risks anymore. He learned how to use a condom. After attending her sessions, I was able to save a friend with Chariette’s help. This friend tried to perform an abortion herself and she was bleeding everywhere. I remembered that Chariette told me about the Cameroon National Planning Association for Family Welfare clinic, so I called her and asked how she could be admitted. She was able to receive post-abortion care but if I hadn’t known Chariette I don’t know what would have happened. I have brothers and I have helped them to change too. I’ve helped them to adopt a healthier sex life. There is HIV around and it’s scary.” Gertrude Zouakeu Noutcha, 29, is a student and peer educator for the Cameroon National Planning Association for Family Welfare (CAMNAFAW)
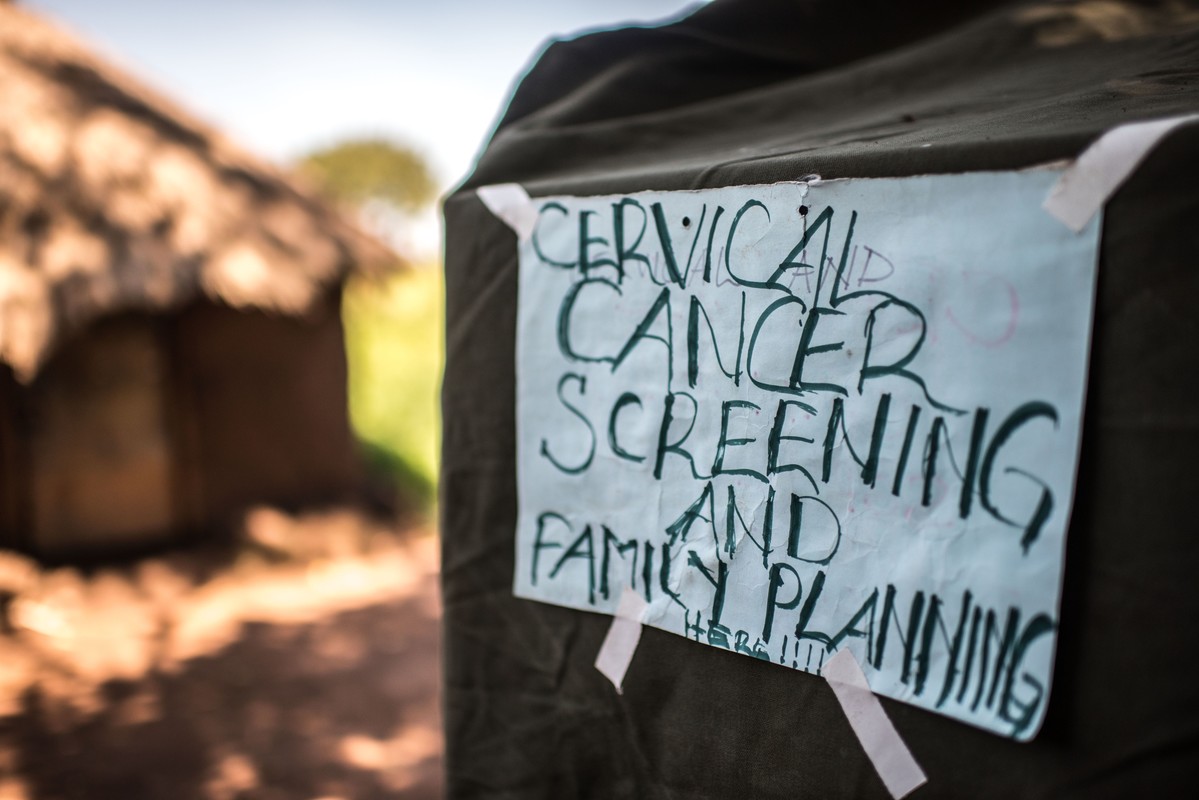
| 22 August 2018
“A radio announcement saved my life” – Gertrude’s story
Gertrude Mugala is a teacher in Fort Portal, a town in Western Uganda. While Gertrude considered herself fairly knowledgeable about cancer, she had never considered taking a screening test or imagined herself ever having the disease. Then one day, she heard an announcement on the radio urging women to go for cervical cancer screenings at a Reproductive Health Uganda (RHU) clinic. “The radio presenter was talking about cervical cancer, and in her message she encouraged all women to get screened. I decided to go and try it out,” she said. Gertrude made her way to RHU's Fort Portal Branch clinic for the free cervical cancer screening. There, she met Ms. Irene Kugonza, an RHU service provider. Ms. Kugonza educated Gertrude and a group of other women about cervical cancer and the importance of routine screening. Gertrude received a type of cervical cancer screening called VIA (visual inspection with acetic acid). "I did not know what was happening" But Gertrude's results were not what she expected; she received a positive result. The good news, however, is that precancerous lesions can be treated if detected early. “I was so shaken when I was told I had pre-cancerous lesions. I did not know what was happening and I didn't believe what I was hearing. I had no idea of my health status. I thought I was healthy, but I was actually harbouring a potential killer disease in me. What would have happened if I didn't go for the screening? If I hadn't heard the radio announcement?” Gertrude was then referred for cryotherapy. “Following cryotherapy, I am now in the process of healing, and I am supposed to go back for review after three months,” said Gertrude. Community screenings Today, Gertrude advocates for cervical cancer screening in her community. She talks to women about cancer, especially cervical cancer, at her workplace, at the market, in meetings, and any other opportunity she gets. “I decided to let women know that cervical cancer is real and it is here with us, and that it kills. At the moment, those are the platforms I have, and I will continue educating women about cancer and encourage them to go for routine testing. I am also happy that I was near my radio that day, where I heard that announcement encouraging all women to get tested for cervical cancer. It might be because of that radio announcement that I am here today,” she said.
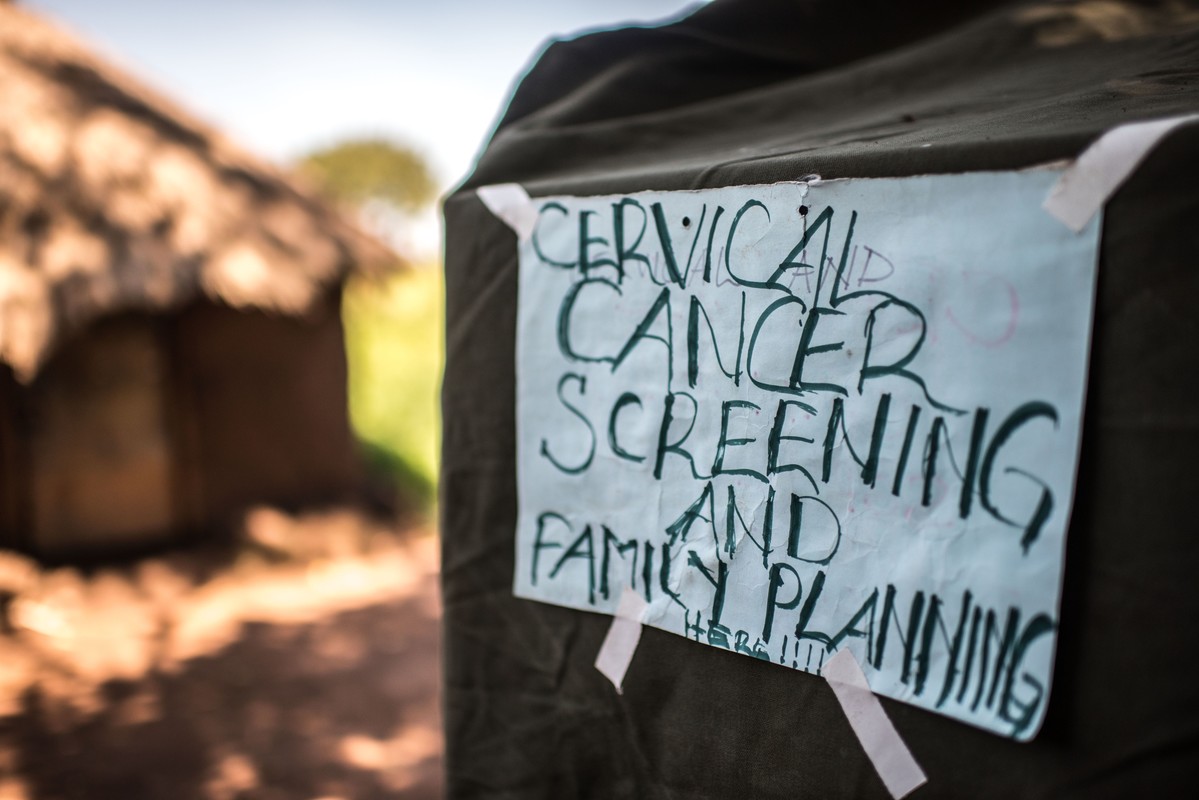
| 24 April 2024
“A radio announcement saved my life” – Gertrude’s story
Gertrude Mugala is a teacher in Fort Portal, a town in Western Uganda. While Gertrude considered herself fairly knowledgeable about cancer, she had never considered taking a screening test or imagined herself ever having the disease. Then one day, she heard an announcement on the radio urging women to go for cervical cancer screenings at a Reproductive Health Uganda (RHU) clinic. “The radio presenter was talking about cervical cancer, and in her message she encouraged all women to get screened. I decided to go and try it out,” she said. Gertrude made her way to RHU's Fort Portal Branch clinic for the free cervical cancer screening. There, she met Ms. Irene Kugonza, an RHU service provider. Ms. Kugonza educated Gertrude and a group of other women about cervical cancer and the importance of routine screening. Gertrude received a type of cervical cancer screening called VIA (visual inspection with acetic acid). "I did not know what was happening" But Gertrude's results were not what she expected; she received a positive result. The good news, however, is that precancerous lesions can be treated if detected early. “I was so shaken when I was told I had pre-cancerous lesions. I did not know what was happening and I didn't believe what I was hearing. I had no idea of my health status. I thought I was healthy, but I was actually harbouring a potential killer disease in me. What would have happened if I didn't go for the screening? If I hadn't heard the radio announcement?” Gertrude was then referred for cryotherapy. “Following cryotherapy, I am now in the process of healing, and I am supposed to go back for review after three months,” said Gertrude. Community screenings Today, Gertrude advocates for cervical cancer screening in her community. She talks to women about cancer, especially cervical cancer, at her workplace, at the market, in meetings, and any other opportunity she gets. “I decided to let women know that cervical cancer is real and it is here with us, and that it kills. At the moment, those are the platforms I have, and I will continue educating women about cancer and encourage them to go for routine testing. I am also happy that I was near my radio that day, where I heard that announcement encouraging all women to get tested for cervical cancer. It might be because of that radio announcement that I am here today,” she said.

| 21 May 2017
A graduate in need turns to sex work
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Lady Mermaid's Bureau. I am Pretty Lynn, aged 25. I am a sex worker but I went to university. I graduated with a Bachelor's Degree in Tourism in 2013. But now, during the day I’m sleeping and during the night I’m working. That is how my day goes every day. I got into sex work through friends. Okay it is not good but I am earning. I tried to get a job when I graduated. I have been applying since I graduated in 2013. I’m still applying but I’m not getting anywhere. You know to get jobs in Uganda; you have to know someone there and no one knows me there. To be a sex worker is like a curse. People look at you like, I don’t know, as someone that has no use in society. People look at you in a bad way. They even don’t consider why you are selling. They just see you as the worst thing that can happen in the society. So it is not comfortable, it is really hard but we try and survive. The fact sex working is illegal means you have to hide yourself when you are selling so that police cannot take you. And then you get diseases, men don’t want to pay. When the police come and take us, sometimes they even use us and don’t pay. So it is really hard. They want a free service. Like if they come and take you and pay that would be fair. But they say it is illegal to sell yourself. But they still use you yet they are saying it is illegal. You can’t report the police because there is no evidence. Abortion and unwanted pregnancies are really common because men don’t want to use condoms and female condoms are really rare and they are expensive. Though at times we get female condoms from Lady Marmaid’s Bureau (LMB) because there are so many of us they can’t keep on giving you them all the time. At times when we get pregnant we use local methods. You can go and use local herbs but it is not safe. One time I used local herbs and I was successful. Then the other time I used Omo washing powder and tea leaves but it was really hard for me. I almost died. I had a friend who died last year from this. But the good thing is that LMB taught us about safe abortion. I have had a safe abortion too. There are some tabs they are called Miso (misoprostol). It costs about fifty thousand shillings (£10 pounds or $20.) It is a lot of money. But if I’m working and I know I’m pregnant, I can say, "this week I’m working for my safe abortion". So if I’m working for twenty thousand, by the end of the week I will have the money. It is expensive compared to Omo at five hundred shillings but that is risky. So if I say I will work this whole week for Miso (misoprostol) it is better. But I'm working and I'm not eating. A project like this one from Lady Mermaid's can help young girls and women. But to take us from sex work, it would really be hard. They would not have enough money to cater for all of us. So what they have to do is to teach us how to protect ourselves, how to defend ourselves. Safe abortion yes. They will just have to sensitise us more about our lives, protection, female condoms and all that. I don't have a boyfriend but maybe when I get money and leave this job I will. But for now, no man would like a woman who sells. No man will bear the wife selling herself. And that will happen only if I get funds, settle somewhere else and become responsible woman. I don’t want this job. I don’t want to be in this business of sex work all the time. I want be married, with my children happily, not selling myself. Stories Read more stories about the amazing success of SAAF in Uganda

| 24 April 2024
A graduate in need turns to sex work
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Lady Mermaid's Bureau. I am Pretty Lynn, aged 25. I am a sex worker but I went to university. I graduated with a Bachelor's Degree in Tourism in 2013. But now, during the day I’m sleeping and during the night I’m working. That is how my day goes every day. I got into sex work through friends. Okay it is not good but I am earning. I tried to get a job when I graduated. I have been applying since I graduated in 2013. I’m still applying but I’m not getting anywhere. You know to get jobs in Uganda; you have to know someone there and no one knows me there. To be a sex worker is like a curse. People look at you like, I don’t know, as someone that has no use in society. People look at you in a bad way. They even don’t consider why you are selling. They just see you as the worst thing that can happen in the society. So it is not comfortable, it is really hard but we try and survive. The fact sex working is illegal means you have to hide yourself when you are selling so that police cannot take you. And then you get diseases, men don’t want to pay. When the police come and take us, sometimes they even use us and don’t pay. So it is really hard. They want a free service. Like if they come and take you and pay that would be fair. But they say it is illegal to sell yourself. But they still use you yet they are saying it is illegal. You can’t report the police because there is no evidence. Abortion and unwanted pregnancies are really common because men don’t want to use condoms and female condoms are really rare and they are expensive. Though at times we get female condoms from Lady Marmaid’s Bureau (LMB) because there are so many of us they can’t keep on giving you them all the time. At times when we get pregnant we use local methods. You can go and use local herbs but it is not safe. One time I used local herbs and I was successful. Then the other time I used Omo washing powder and tea leaves but it was really hard for me. I almost died. I had a friend who died last year from this. But the good thing is that LMB taught us about safe abortion. I have had a safe abortion too. There are some tabs they are called Miso (misoprostol). It costs about fifty thousand shillings (£10 pounds or $20.) It is a lot of money. But if I’m working and I know I’m pregnant, I can say, "this week I’m working for my safe abortion". So if I’m working for twenty thousand, by the end of the week I will have the money. It is expensive compared to Omo at five hundred shillings but that is risky. So if I say I will work this whole week for Miso (misoprostol) it is better. But I'm working and I'm not eating. A project like this one from Lady Mermaid's can help young girls and women. But to take us from sex work, it would really be hard. They would not have enough money to cater for all of us. So what they have to do is to teach us how to protect ourselves, how to defend ourselves. Safe abortion yes. They will just have to sensitise us more about our lives, protection, female condoms and all that. I don't have a boyfriend but maybe when I get money and leave this job I will. But for now, no man would like a woman who sells. No man will bear the wife selling herself. And that will happen only if I get funds, settle somewhere else and become responsible woman. I don’t want this job. I don’t want to be in this business of sex work all the time. I want be married, with my children happily, not selling myself. Stories Read more stories about the amazing success of SAAF in Uganda