Spotlight
A selection of stories from across the Federation

France, Germany, Poland, United Kingdom, United States, Colombia, India, Tunisia
Abortion Rights: Latest Decisions and Developments around the World
The global landscape of abortion rights continues to evolve in 2024, with new legislation and feminist movements fighting for better access. Let's take a trip around the world to see the latest developments.
Most Popular This Week
France, Germany, Poland, United Kingdom, United States, Colombia, India, Tunisia

Abortion Rights: Latest Decisions and Developments around the World
Over the past 30 years, more than

Palestine

In their own words: The people providing sexual and reproductive health care under bombardment in Gaza
Week after week, heavy Israeli bombardment from air, land, and sea, has continued across most of the Gaza Strip.
Vanuatu

When getting to the hospital is difficult, Vanuatu mobile outreach can save lives
In the mountains of Kumera on Tanna Island, Vanuatu, the village women of Kamahaul normally spend over 10,000 Vatu ($83 USD) to travel to the nearest hospital.
Vanuatu

Sex: changing minds and winning hearts in Tanna, Vanuatu
“Very traditional.” These two words are often used to describe the people of Tanna in Vanuatu, one of the most populated islands in the small country in the Pacific.
Vanuatu

Vanuatu cyclone response: The mental health toll on humanitarian providers
Girls and women from nearby villages flock to mobile health clinics set up by the Vanuatu Family Health Association (VFHA).
Cook Islands

Trans & Proud: Being Transgender in the Cook Islands
It’s a scene like many others around the world: a loving family pour over childhood photos, giggling and reminiscing about the memories.
Cook Islands

In Pictures: The activists who helped win LGBTI+ rights in the Cook Islands
The Cook Islands has removed a law that criminalizes homosexuality, in a huge victory for the local LGBTI+ community.
Filter our stories by:
- Asociación Pro-Bienestar de la Familia Colombiana
- Associação Moçambicana para Desenvolvimento da Família
- Association Béninoise pour la Promotion de la Famille
- Association Burundaise pour le Bien-Etre Familial
- Association Malienne pour la Protection et la Promotion de la Famille
- Association Tunisienne de la Santé de la Reproduction
- Botswana Family Welfare Association
- Family Guidance Association of Ethiopia
- Family Planning Association of India
- Family Planning Association of Malawi
- Family Planning Association of Nepal
- Family Planning Association of Sri Lanka
- Family Planning Association of Trinidad and Tobago
- Indonesian Planned Parenthood Association
- Kiribati Family Health Association
- Mouvement Français pour le Planning Familial
- Palestinian Family Planning and Protection Association (PFPPA)
- Planned Parenthood Association of Thailand
- Planned Parenthood Association of Zambia
- Planned Parenthood Federation of America
- Pro Familia - Germany
- Reproductive & Family Health Association of Fiji
- Reproductive Health Uganda
- Somaliland Family Health Association
- Tonga Family Health Association
- Vanuatu Family Health Association


| 08 January 2021
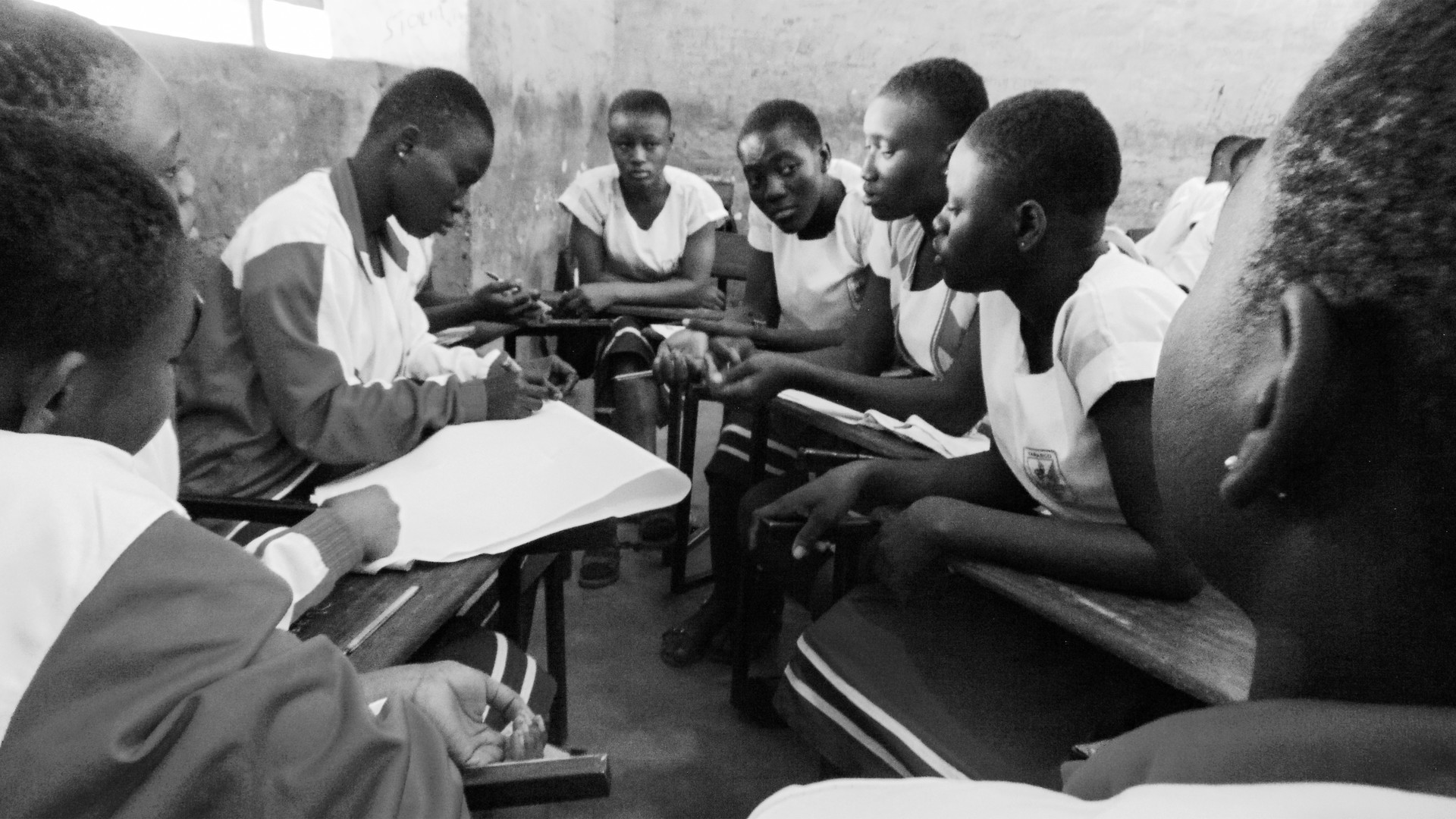
"The movement helps girls to know their rights and their bodies"
My name is Fatoumata Yehiya Maiga. I’m 23-years-old, and I’m an IT specialist. I joined the Youth Action Movement at the end of 2018. The head of the movement in Mali is a friend of mine, and I met her before I knew she was the president. She invited me to their events and over time persuaded me to join. I watched them raising awareness about sexual and reproductive health, using sketches and speeches. I learnt a lot. Overcoming taboos I went home and talked about what I had seen and learnt with my family. In Africa, and even more so in the village where I come from in Gao, northern Mali, people don’t talk about these things. I wanted to take my sisters to the events, but every time I spoke about them my relatives would just say it was to teach girls to have sex, and that it’s taboo. That’s not what I believe. I think the movement helps girls, most of all, to know their sexual rights, their bodies, what to do and what not to do to stay healthy and safe. They don’t understand this concept. My family would say it was just a smokescreen to convince girls to get involved in something dirty. I have had to tell my younger cousins about their periods, for example, when they came from the village to live in the city. One of my cousins was so scared, and told me she was bleeding from her vagina and didn’t know why. We talk about managing periods in the Youth Action Movement, as well as how to manage cramps and feel better. The devastating impact of FGM But there was a much more important reason for me to join the movement. My parents are educated, so me and my sisters were never cut. I learned about female genital mutilation at a conference I attended in 2016. I didn’t know that there were different types of severity and ways that girls could be cut. I hadn’t understood quite how dangerous this practice is. Then, two years ago, I lost my friend Aïssata. She got married young, at 17. She struggled to conceive until she was 23. The day she gave birth, there were complications and she died. The doctors said that the excision was botched and that’s what killed her. From that day on, I decided I needed to teach all the girls in my community about how harmful this practice is for their health. I was so horrified by the way she died. Normally, girls in Mali are cut when they are three or four years old, though for some it’s done at birth. When they are older and get pregnant, I know they face the same challenges as every woman does giving birth, but they also live with the dangerous consequences of this unhealthy practice. The importance of talking openly The problem lies with the families. I want us, as a movement, to talk with the parents and explain to them how they can contribute to their children’s sexual health. I wish it were no longer a taboo between parents and their girls. But if we talk in such direct terms, they only see disobedience, and say that we are encouraging promiscuity. We need to talk to teenagers because they are already parents in many cases. They are the ones who decide to go through with cutting their daughters, or not. A lot of Mali is hard to reach though. We need travelling groups to go to those isolated rural areas and talk to people about sexual health. Pregnancy is the girl’s decision, and girls have a right to be healthy, and to choose their future.

| 19 April 2024
"The movement helps girls to know their rights and their bodies"
My name is Fatoumata Yehiya Maiga. I’m 23-years-old, and I’m an IT specialist. I joined the Youth Action Movement at the end of 2018. The head of the movement in Mali is a friend of mine, and I met her before I knew she was the president. She invited me to their events and over time persuaded me to join. I watched them raising awareness about sexual and reproductive health, using sketches and speeches. I learnt a lot. Overcoming taboos I went home and talked about what I had seen and learnt with my family. In Africa, and even more so in the village where I come from in Gao, northern Mali, people don’t talk about these things. I wanted to take my sisters to the events, but every time I spoke about them my relatives would just say it was to teach girls to have sex, and that it’s taboo. That’s not what I believe. I think the movement helps girls, most of all, to know their sexual rights, their bodies, what to do and what not to do to stay healthy and safe. They don’t understand this concept. My family would say it was just a smokescreen to convince girls to get involved in something dirty. I have had to tell my younger cousins about their periods, for example, when they came from the village to live in the city. One of my cousins was so scared, and told me she was bleeding from her vagina and didn’t know why. We talk about managing periods in the Youth Action Movement, as well as how to manage cramps and feel better. The devastating impact of FGM But there was a much more important reason for me to join the movement. My parents are educated, so me and my sisters were never cut. I learned about female genital mutilation at a conference I attended in 2016. I didn’t know that there were different types of severity and ways that girls could be cut. I hadn’t understood quite how dangerous this practice is. Then, two years ago, I lost my friend Aïssata. She got married young, at 17. She struggled to conceive until she was 23. The day she gave birth, there were complications and she died. The doctors said that the excision was botched and that’s what killed her. From that day on, I decided I needed to teach all the girls in my community about how harmful this practice is for their health. I was so horrified by the way she died. Normally, girls in Mali are cut when they are three or four years old, though for some it’s done at birth. When they are older and get pregnant, I know they face the same challenges as every woman does giving birth, but they also live with the dangerous consequences of this unhealthy practice. The importance of talking openly The problem lies with the families. I want us, as a movement, to talk with the parents and explain to them how they can contribute to their children’s sexual health. I wish it were no longer a taboo between parents and their girls. But if we talk in such direct terms, they only see disobedience, and say that we are encouraging promiscuity. We need to talk to teenagers because they are already parents in many cases. They are the ones who decide to go through with cutting their daughters, or not. A lot of Mali is hard to reach though. We need travelling groups to go to those isolated rural areas and talk to people about sexual health. Pregnancy is the girl’s decision, and girls have a right to be healthy, and to choose their future.

| 23 September 2020
In pictures: Innovating during COVID-19
Women around the world have faced multiple barriers to accessing safe abortion care during the COVID-19 pandemic including the de-prioritization of sexual and reproductive healthcare, overwhelmed health systems and restrictions on movement. The COVID-19 crisis has sparked innovation among IPPF Member Associations who responded swiftly by developing new approaches to reach women with safe abortion care including telemedicine and home-based provision of medical abortion. Strong evidence generated from this work supports the continuation and strengthening of these approaches beyond the end of the pandemic. Cameroon Cameroon National Planning Association for Family Welfare (CAMNAFAW) To ensure that quality abortion care can be provided to women during travel restrictions, CAMNAFAW’s service providers travel to partner clinics in underserved areas and to clients’ homes to provide medical and surgical abortion care. This model of taking safe abortion care closer to women will continue even with easing of travel restrictions, as this has been found to be an effective and acceptable approach to increasing access.Photo: IPPF/Xaume Olleros/Cameroon Share on Twitter Share on Facebook Share via WhatsApp Share via Email Guinea Association Guinéenne pour le Bien-Etre Familial (AGBEF) Building on lessons learned during the Ebola crisis in Guinea, AGBEF quickly took measures to prevent infection in its clinics to continue providing sexual and reproductive healthcare, including surgical and medical abortion, in a safe environment. AGBEF donated protective materials to communities, including hand-washing stations, face masks and antibacterial gel, alongside messaging on infection prevention. This community visibility reassures clients they can safely attend AGBEF clinics for abortion and contraceptive care.Photo: AGBEF/Guinea Share on Twitter Share on Facebook Share via WhatsApp Share via Email India Family Planning Association of India (FPA India) FPA India and partners advocated to have sexual and reproductive healthcare, including abortion, recognized as essential by the government, which meant FPA India could continue healthcare delivery during the national lockdown. To reduce in-person clinic visits, FPA India established teleconsultation and counselling for abortion care, and is continuing to provide in-clinic care for both medical and surgical abortion. Photo: IPPF/Alison Joyce/India Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nepal Family Planning Association of Nepal (FPAN) FPAN and partners advocated for interim approval of home provision of medical abortion and telemedicine for abortion counselling during COVID-19. FPAN is now implementing these approaches, ensuring continued access to abortion care in Nepal, where many people live in remote locations with limited mobility, which has been further restricted by COVID-19 lockdowns. Photo: FPAN/Nepal Share on Twitter Share on Facebook Share via WhatsApp Share via Email Pakistan Rahnuma – Family Planning Association of Pakistan (Rahnuma-FPAP) Rahnuma-FPAP and partners successfully advocated for the government to class sexual and reproductive healthcare as ‘essential’, which enabled the team to continue providing post-abortion care during the pandemic. Rahnuma-FPAP expanded its telemedicine and home-based provision for menstrual regulation counselling and post-abortion care. These new approaches have ensured continued access to services for clients unable to reach clinics.Photo: Rahnuma-FPAP/Pakistan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Palestine Palestinian Family Planning and Protection Association (PFPPA) In response to the government-mandated closure of its clinics, PFPPA quickly established a toll-free call centre which provides consultations, counselling, referrals and follow-up, including consultation for abortion care through a harm reduction approach, ensuring that women are provided with accurate information. Due to its success, PFPPA is exploring options for continuing this healthcare delivery model beyond the pandemic, with the aim of keeping it free of charge for users.Photo: SAAF/Samar Hazboun/Palestine Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sudan Sudan Family Planning Association (SFPA) Following a nation-wide shutdown in April, SFPA established a call centre to increase access to healthcare, including abortion and contraceptive counselling and referrals. An unexpected outcome of the new call centre is that it has reached an increased number of young women who regularly call to discuss their reproductive health and rights. SFPA is working towards institutionalizing this model for continuation beyond the pandemic.Photo: SFPA/Sudan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Togo Association Togolaise pour le Bien-Etre Familial (ATBEF) ATBEF adapted its mobile application ‘Infos Ado Jeunes’, adding a toll-free teleconsultation service for young clients to use to access abortion consultations and pre- and post-abortion counselling. This app has given young clients ongoing access to care when they face challenges travelling to clinics. It has also eased overall client flow in clinics at a time when social distancing is being implemented.Photo: ATBEF/Togo Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 19 April 2024
In pictures: Innovating during COVID-19
Women around the world have faced multiple barriers to accessing safe abortion care during the COVID-19 pandemic including the de-prioritization of sexual and reproductive healthcare, overwhelmed health systems and restrictions on movement. The COVID-19 crisis has sparked innovation among IPPF Member Associations who responded swiftly by developing new approaches to reach women with safe abortion care including telemedicine and home-based provision of medical abortion. Strong evidence generated from this work supports the continuation and strengthening of these approaches beyond the end of the pandemic. Cameroon Cameroon National Planning Association for Family Welfare (CAMNAFAW) To ensure that quality abortion care can be provided to women during travel restrictions, CAMNAFAW’s service providers travel to partner clinics in underserved areas and to clients’ homes to provide medical and surgical abortion care. This model of taking safe abortion care closer to women will continue even with easing of travel restrictions, as this has been found to be an effective and acceptable approach to increasing access.Photo: IPPF/Xaume Olleros/Cameroon Share on Twitter Share on Facebook Share via WhatsApp Share via Email Guinea Association Guinéenne pour le Bien-Etre Familial (AGBEF) Building on lessons learned during the Ebola crisis in Guinea, AGBEF quickly took measures to prevent infection in its clinics to continue providing sexual and reproductive healthcare, including surgical and medical abortion, in a safe environment. AGBEF donated protective materials to communities, including hand-washing stations, face masks and antibacterial gel, alongside messaging on infection prevention. This community visibility reassures clients they can safely attend AGBEF clinics for abortion and contraceptive care.Photo: AGBEF/Guinea Share on Twitter Share on Facebook Share via WhatsApp Share via Email India Family Planning Association of India (FPA India) FPA India and partners advocated to have sexual and reproductive healthcare, including abortion, recognized as essential by the government, which meant FPA India could continue healthcare delivery during the national lockdown. To reduce in-person clinic visits, FPA India established teleconsultation and counselling for abortion care, and is continuing to provide in-clinic care for both medical and surgical abortion. Photo: IPPF/Alison Joyce/India Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nepal Family Planning Association of Nepal (FPAN) FPAN and partners advocated for interim approval of home provision of medical abortion and telemedicine for abortion counselling during COVID-19. FPAN is now implementing these approaches, ensuring continued access to abortion care in Nepal, where many people live in remote locations with limited mobility, which has been further restricted by COVID-19 lockdowns. Photo: FPAN/Nepal Share on Twitter Share on Facebook Share via WhatsApp Share via Email Pakistan Rahnuma – Family Planning Association of Pakistan (Rahnuma-FPAP) Rahnuma-FPAP and partners successfully advocated for the government to class sexual and reproductive healthcare as ‘essential’, which enabled the team to continue providing post-abortion care during the pandemic. Rahnuma-FPAP expanded its telemedicine and home-based provision for menstrual regulation counselling and post-abortion care. These new approaches have ensured continued access to services for clients unable to reach clinics.Photo: Rahnuma-FPAP/Pakistan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Palestine Palestinian Family Planning and Protection Association (PFPPA) In response to the government-mandated closure of its clinics, PFPPA quickly established a toll-free call centre which provides consultations, counselling, referrals and follow-up, including consultation for abortion care through a harm reduction approach, ensuring that women are provided with accurate information. Due to its success, PFPPA is exploring options for continuing this healthcare delivery model beyond the pandemic, with the aim of keeping it free of charge for users.Photo: SAAF/Samar Hazboun/Palestine Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sudan Sudan Family Planning Association (SFPA) Following a nation-wide shutdown in April, SFPA established a call centre to increase access to healthcare, including abortion and contraceptive counselling and referrals. An unexpected outcome of the new call centre is that it has reached an increased number of young women who regularly call to discuss their reproductive health and rights. SFPA is working towards institutionalizing this model for continuation beyond the pandemic.Photo: SFPA/Sudan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Togo Association Togolaise pour le Bien-Etre Familial (ATBEF) ATBEF adapted its mobile application ‘Infos Ado Jeunes’, adding a toll-free teleconsultation service for young clients to use to access abortion consultations and pre- and post-abortion counselling. This app has given young clients ongoing access to care when they face challenges travelling to clinics. It has also eased overall client flow in clinics at a time when social distancing is being implemented.Photo: ATBEF/Togo Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 13 August 2020
In pictures: Delivering healthcare to remote communities in Fiji
In early April 2020, the all too familiar destruction of a Tropical Cyclone (TC) – Harold – hit the Solomon Islands, Vanuatu, Fiji and Tonga. One of the worst affected areas was the Eastern part of Fiji. Through support by Department of Foreign Affairs and Trade (DFAT), our Member Association, Reproductive and Family Health Association of Fiji (RFHAF), was quick to respond ensuring access to essential sexual and reproductive healthcare for Kadavu’s women, girls, and vulnerable groups. Fiji's vulnerable coastline Fiji’s worst affected area was the Eastern part, with TC Harold bringing destructive storm force winds and storm surge. RFHAF focused its humanitarian response on the local Kadavu population. This remote area proves a challenge to reach for the team with supplies. Share on Twitter Share on Facebook Share via WhatsApp Share via Email RFHAF's humanitarian response team tackle rough terrain National travel restrictions - due to the current COVID-19 pandemic - on all inter island transfers has slowed the response in some areas, including Kadavu. The island of Kadavu is one of the least developed areas of Fiji, the main source of income is substance living (Yaqona). Transport around the island is difficult, with very few roads, no public water system or electricity. The humanitarian team from RFHAF travels by boat and then on foot. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Asenaca, client Kadavu, the biggest island in the Eastern division has the greatest population (10,897). 197 evacuation centres were activated in total, initially hosting over 6,240 people. Many are women of reproductive age, with an estimated 150 currently pregnant. Asenaca learns about breast cancer self-checks from RFHAF’s healthcare provider, Karo. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nasi, RFHAF healthcare provider The medical mobile team deliver a broad range of healthcare including contraception, information and counselling on sexual health, pregnancy, HIV and STI care and testing. RFHAF Team in Kadavu performing general health checks after TC Harold. Nasi administers a HPV shot to a client. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Kate, client Young women and girls are at the heart of RFHAF’s healthcare provision. Kate walks home with her dignity kit after a health check at the mobile clinic. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Karo, RFHAF healthcare worker RFHAF offers sexual and reproductive healthcare as well as counselling, and referrals for follow up care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Alidi, RFHAF healthcare worker The team ensures young people in the community are not forgotten and provide information and education on relationships and sexual health and rights. Alidi conducting a session with a local group of young people at Gasele, Kadavu.Photos ©IPPF/Rob Rickman/Fiji Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 19 April 2024
In pictures: Delivering healthcare to remote communities in Fiji
In early April 2020, the all too familiar destruction of a Tropical Cyclone (TC) – Harold – hit the Solomon Islands, Vanuatu, Fiji and Tonga. One of the worst affected areas was the Eastern part of Fiji. Through support by Department of Foreign Affairs and Trade (DFAT), our Member Association, Reproductive and Family Health Association of Fiji (RFHAF), was quick to respond ensuring access to essential sexual and reproductive healthcare for Kadavu’s women, girls, and vulnerable groups. Fiji's vulnerable coastline Fiji’s worst affected area was the Eastern part, with TC Harold bringing destructive storm force winds and storm surge. RFHAF focused its humanitarian response on the local Kadavu population. This remote area proves a challenge to reach for the team with supplies. Share on Twitter Share on Facebook Share via WhatsApp Share via Email RFHAF's humanitarian response team tackle rough terrain National travel restrictions - due to the current COVID-19 pandemic - on all inter island transfers has slowed the response in some areas, including Kadavu. The island of Kadavu is one of the least developed areas of Fiji, the main source of income is substance living (Yaqona). Transport around the island is difficult, with very few roads, no public water system or electricity. The humanitarian team from RFHAF travels by boat and then on foot. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Asenaca, client Kadavu, the biggest island in the Eastern division has the greatest population (10,897). 197 evacuation centres were activated in total, initially hosting over 6,240 people. Many are women of reproductive age, with an estimated 150 currently pregnant. Asenaca learns about breast cancer self-checks from RFHAF’s healthcare provider, Karo. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nasi, RFHAF healthcare provider The medical mobile team deliver a broad range of healthcare including contraception, information and counselling on sexual health, pregnancy, HIV and STI care and testing. RFHAF Team in Kadavu performing general health checks after TC Harold. Nasi administers a HPV shot to a client. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Kate, client Young women and girls are at the heart of RFHAF’s healthcare provision. Kate walks home with her dignity kit after a health check at the mobile clinic. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Karo, RFHAF healthcare worker RFHAF offers sexual and reproductive healthcare as well as counselling, and referrals for follow up care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Alidi, RFHAF healthcare worker The team ensures young people in the community are not forgotten and provide information and education on relationships and sexual health and rights. Alidi conducting a session with a local group of young people at Gasele, Kadavu.Photos ©IPPF/Rob Rickman/Fiji Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 16 July 2020
"Before, there was no safe abortion"
Rewda Kedir works as a midwife in a rural area of the Oromia region in southwest Ethiopia. Only 14% of married women are using any method of contraception here. The government hospital Rewda works in is supported to provide a full range of sexual and reproductive healthcare, which includes providing free contraceptives and comprehensive abortion care. In January 2017, the maternal healthcare clinic faced shortages of contraceptives after the US administration reactivated and expanded the Global Gag Rule, which does not allow any funding to go to organizations associated with providing abortion care. Fortunately in this case, the shortages only lasted a month due to the government of the Netherlands stepping in and matching lost funding. “Before, we had a shortage of contraceptive pills and emergency contraceptives. We would have to give people prescriptions and they would go to private clinics and where they had to pay," Rewda tells us. "When I first came to this clinic, there was a real shortage of people trained in family planning. I was the only one. Now there are many people trained on family planning, and when I’m not here, people can help." "There used to be a shortage of choice and alternatives, and now there are many. And the implant procedures are better because there are newer products that are much smaller so putting them in is less invasive.” Opening a dialogue on contraception The hospital has been providing medical abortions for six years. “Before, there was no safe abortion," says Rewda. She explains how people would go to 'traditional' healers and then come to the clinic with complications like sepsis, bleeding, anaemia and toxic shock. If they had complications or infections above nine weeks, Rewda and her colleagues would send them to Jimma, the regional capital. "Before, it was very difficult to persuade them to use family planning, and we had to have a lot of conversations. Now, they come 45 days after delivery to speak to us about this and get their babies immunised," she explains. "They want contraceptives to space out their children. Sometimes their husbands don’t like them coming to get family planning so we have to lock their appointment cards away. Their husbands want more children and they think that women who do not keep having their children will go with other men." "More kids, more wealth" Rewda tells us that they've used family counselling to try and persuade men to reconsider their ideas about contraception, by explaining to them that continuously giving birth under unsafe circumstances can affect a woman's health and might lead to maternal death, damage the uterus and lead to long-term complications. "Here, people believe that more kids means more wealth, and religion restricts family planning services. Before, they did not have good training on family planning and abortion. Now, women that have abortions get proper care and the counseling and education has improved. There are still unsafe abortions but they have really reduced. We used to see about 40 a year and now it’s one or two." However, problems still exist. "There are some complications, like irregular bleeding from some contraceptives," Rewda says, and that "women still face conflict with their husbands over family planning and sometimes have to go to court to fight this or divorce them.”

| 19 April 2024
"Before, there was no safe abortion"
Rewda Kedir works as a midwife in a rural area of the Oromia region in southwest Ethiopia. Only 14% of married women are using any method of contraception here. The government hospital Rewda works in is supported to provide a full range of sexual and reproductive healthcare, which includes providing free contraceptives and comprehensive abortion care. In January 2017, the maternal healthcare clinic faced shortages of contraceptives after the US administration reactivated and expanded the Global Gag Rule, which does not allow any funding to go to organizations associated with providing abortion care. Fortunately in this case, the shortages only lasted a month due to the government of the Netherlands stepping in and matching lost funding. “Before, we had a shortage of contraceptive pills and emergency contraceptives. We would have to give people prescriptions and they would go to private clinics and where they had to pay," Rewda tells us. "When I first came to this clinic, there was a real shortage of people trained in family planning. I was the only one. Now there are many people trained on family planning, and when I’m not here, people can help." "There used to be a shortage of choice and alternatives, and now there are many. And the implant procedures are better because there are newer products that are much smaller so putting them in is less invasive.” Opening a dialogue on contraception The hospital has been providing medical abortions for six years. “Before, there was no safe abortion," says Rewda. She explains how people would go to 'traditional' healers and then come to the clinic with complications like sepsis, bleeding, anaemia and toxic shock. If they had complications or infections above nine weeks, Rewda and her colleagues would send them to Jimma, the regional capital. "Before, it was very difficult to persuade them to use family planning, and we had to have a lot of conversations. Now, they come 45 days after delivery to speak to us about this and get their babies immunised," she explains. "They want contraceptives to space out their children. Sometimes their husbands don’t like them coming to get family planning so we have to lock their appointment cards away. Their husbands want more children and they think that women who do not keep having their children will go with other men." "More kids, more wealth" Rewda tells us that they've used family counselling to try and persuade men to reconsider their ideas about contraception, by explaining to them that continuously giving birth under unsafe circumstances can affect a woman's health and might lead to maternal death, damage the uterus and lead to long-term complications. "Here, people believe that more kids means more wealth, and religion restricts family planning services. Before, they did not have good training on family planning and abortion. Now, women that have abortions get proper care and the counseling and education has improved. There are still unsafe abortions but they have really reduced. We used to see about 40 a year and now it’s one or two." However, problems still exist. "There are some complications, like irregular bleeding from some contraceptives," Rewda says, and that "women still face conflict with their husbands over family planning and sometimes have to go to court to fight this or divorce them.”

| 18 June 2020
In pictures: Healthcare in the face of the climate crisis in Kiribati
Humanitarian crises Largely brought on by sudden onset and slow-onset natural disasters, humanitarian crises are increasingly prevalent in the Pacific. During responses to humanitarian crises in the Pacific, sexual and reproductive healthcare is often under-prioritised and under-resourced. As a result, women and girls of reproductive age and vulnerable and marginalized groups are disproportionately affected and facing increased health and psychosocial risks. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Fragile environments Low topography, rising sea levels and insufficient fresh water supply leaves Kiribati’s population vulnerable to the effects of the climate crisis. The fragility of the outer islands of Kiribati during natural disasters is compounded by their geographic isolation, which makes transportation and communication during post-disaster relief and response both expensive and difficult. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Coastal exposure The majority of the population of 115,000 people live a subsistence lifestyle. Communities are geographically dispersed across 33 atolls covering 3.5 million square kilometres in the central Pacific Ocean. The population and infrastructure within Kiribati are largely concentrated on the coast, where communities face increased exposure to climate threats and natural hazards such as tsunamis, earthquakes, king tides, flooding, droughts, and occasionally cyclones. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Takaria, leader and youth organizer in the Tebikenikua community Takaria will be running to be a Member of Parliament in Kiribati in 2020. “I assist the youth with family problems and family planning and disasters. In our community there are unforeseen pregnancies, domestic violence, and disasters such as high tide waters and strong winds, which can also affect this community. The Kiribati Family Health Association (KFHA) is the key point for us with outreach and training so people in this community know how to prevent and treat STIs, etc. They all know where the KFHA clinic is and that they can get counselling or services there. The problem now is you can’t survive with the sea rise levels. I want all members of my community to live better and have better health and peace.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Susan*, sex worker Susan receives care at the Kiribati Family Health Association (KFHA) including a pap smear. Susan*, 28, is a sex worker from the town of Betio on the main island of Kiribati. Originally from an outlying island, she moved into Tarawa to seek work. Unable to find employment that would fulfill her dream of sending money back to her two children, she was introduced to sex work. With other sex workers, she regularly travels out to the large cargo ships from China, Philippines and Korea anchored off the coast of Kiribati. Despite her new income, she still can’t speak with her children or see them due to the restrictive costs involved of travel between islands.*pseudonym Share on Twitter Share on Facebook Share via WhatsApp Share via Email Theta, 25-year-old mother and youth volunteer Theta is part of the Humanitarian Youth Club set up by the Kiribati Family Health Association in her village. “We face a lot of situations here, one of them is disasters and the second is unemployment and school drop out with our youth. I have helped the Humanitarian Youth Club to apply for financial grants from the Australian High Commission [for $1,000] I am recognized as the smartest member who can write in English. We have learned how to design a disaster plan for the community and share our ideas on sexual and reproductive issues such as STIs. We discuss what we can do for the next strong tide, where we can gather as a community and what we can do if even the maneabe (town hall) floods? If the tide and wind is too strong, we need to go to another safer place, such as another community’s town hall. For now, I want to enjoy the chance to be in our own beloved country. I won’t move until the majority have already left. I want my daughter to grow up in the same place I grew up in.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Beitau, youth volunteer Beitau is the Chairperson of the Humanitarian Youth Club. “I was lucky to be selected as Chairperson as the Humanitarian Youth Club. I feel like I get more respect from the community now I am in this position. I would love advanced training on leadership now, to further assist the club. As I am the Chairperson of the HYC, my main target is to help people during a disaster. I have attended training through KFHA. What I took from this is that when a disaster strikes, we have to do our best for pregnant women, small children and people with disabilities. They more vulnerable and less able to survive a disaster.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Abe, youth officer Abe was involved with KFHA since 2012. “I was inspired by what they KFHA was doing and the issues they were addressing that affects youth. I was surprised to see how many young people come to the clinic as they are affected by STIs, HIV and teenage pregnancy. The lack of education here is a big problem, most people here have a lot of children and yet can’t afford to send them to school. Sexual and reproductive health is our responsibility and we must talk about it with young people. Climate change affects many countries, but Kiribati is small and low lying. I used to go visit a very nice beach with a lot of nice trees and plants. Now, the trees are gone, and the waves have taken over, and the houses have disappeared so no one can build there. In my role as a youth worker and activist, I tell people to fight climate change: to grow more mangroves, to clean up the beach, because we love our Kiribati.”©IPPF/Hannah Maule-Ffinch/Kiribati Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 19 April 2024
In pictures: Healthcare in the face of the climate crisis in Kiribati
Humanitarian crises Largely brought on by sudden onset and slow-onset natural disasters, humanitarian crises are increasingly prevalent in the Pacific. During responses to humanitarian crises in the Pacific, sexual and reproductive healthcare is often under-prioritised and under-resourced. As a result, women and girls of reproductive age and vulnerable and marginalized groups are disproportionately affected and facing increased health and psychosocial risks. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Fragile environments Low topography, rising sea levels and insufficient fresh water supply leaves Kiribati’s population vulnerable to the effects of the climate crisis. The fragility of the outer islands of Kiribati during natural disasters is compounded by their geographic isolation, which makes transportation and communication during post-disaster relief and response both expensive and difficult. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Coastal exposure The majority of the population of 115,000 people live a subsistence lifestyle. Communities are geographically dispersed across 33 atolls covering 3.5 million square kilometres in the central Pacific Ocean. The population and infrastructure within Kiribati are largely concentrated on the coast, where communities face increased exposure to climate threats and natural hazards such as tsunamis, earthquakes, king tides, flooding, droughts, and occasionally cyclones. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Takaria, leader and youth organizer in the Tebikenikua community Takaria will be running to be a Member of Parliament in Kiribati in 2020. “I assist the youth with family problems and family planning and disasters. In our community there are unforeseen pregnancies, domestic violence, and disasters such as high tide waters and strong winds, which can also affect this community. The Kiribati Family Health Association (KFHA) is the key point for us with outreach and training so people in this community know how to prevent and treat STIs, etc. They all know where the KFHA clinic is and that they can get counselling or services there. The problem now is you can’t survive with the sea rise levels. I want all members of my community to live better and have better health and peace.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Susan*, sex worker Susan receives care at the Kiribati Family Health Association (KFHA) including a pap smear. Susan*, 28, is a sex worker from the town of Betio on the main island of Kiribati. Originally from an outlying island, she moved into Tarawa to seek work. Unable to find employment that would fulfill her dream of sending money back to her two children, she was introduced to sex work. With other sex workers, she regularly travels out to the large cargo ships from China, Philippines and Korea anchored off the coast of Kiribati. Despite her new income, she still can’t speak with her children or see them due to the restrictive costs involved of travel between islands.*pseudonym Share on Twitter Share on Facebook Share via WhatsApp Share via Email Theta, 25-year-old mother and youth volunteer Theta is part of the Humanitarian Youth Club set up by the Kiribati Family Health Association in her village. “We face a lot of situations here, one of them is disasters and the second is unemployment and school drop out with our youth. I have helped the Humanitarian Youth Club to apply for financial grants from the Australian High Commission [for $1,000] I am recognized as the smartest member who can write in English. We have learned how to design a disaster plan for the community and share our ideas on sexual and reproductive issues such as STIs. We discuss what we can do for the next strong tide, where we can gather as a community and what we can do if even the maneabe (town hall) floods? If the tide and wind is too strong, we need to go to another safer place, such as another community’s town hall. For now, I want to enjoy the chance to be in our own beloved country. I won’t move until the majority have already left. I want my daughter to grow up in the same place I grew up in.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Beitau, youth volunteer Beitau is the Chairperson of the Humanitarian Youth Club. “I was lucky to be selected as Chairperson as the Humanitarian Youth Club. I feel like I get more respect from the community now I am in this position. I would love advanced training on leadership now, to further assist the club. As I am the Chairperson of the HYC, my main target is to help people during a disaster. I have attended training through KFHA. What I took from this is that when a disaster strikes, we have to do our best for pregnant women, small children and people with disabilities. They more vulnerable and less able to survive a disaster.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Abe, youth officer Abe was involved with KFHA since 2012. “I was inspired by what they KFHA was doing and the issues they were addressing that affects youth. I was surprised to see how many young people come to the clinic as they are affected by STIs, HIV and teenage pregnancy. The lack of education here is a big problem, most people here have a lot of children and yet can’t afford to send them to school. Sexual and reproductive health is our responsibility and we must talk about it with young people. Climate change affects many countries, but Kiribati is small and low lying. I used to go visit a very nice beach with a lot of nice trees and plants. Now, the trees are gone, and the waves have taken over, and the houses have disappeared so no one can build there. In my role as a youth worker and activist, I tell people to fight climate change: to grow more mangroves, to clean up the beach, because we love our Kiribati.”©IPPF/Hannah Maule-Ffinch/Kiribati Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 04 June 2020
In pictures: Resilience and innovation in the face of COVID-19
Healthcare providers in their PPE Lebanon Association for Family Health (SALAMA) “After the extension of the general mobilization and in order to provide the services to the most in need population, we decided to re-open the clinic. For this purpose, we are developing a plan for the work during the next weeks, taking into consideration the protocols and procedures taken in Lebanon. This will include an isolation room before the consultation and an assessment of the patient’s status and any symptoms that may relate to the coronavirus. In addition to all the precaution procedures including separation, our clinic was sterilized by a specialized company.”Lina Sabra, the Executive Director of the Lebanese Association for Family Health (SALAMA) Share on Twitter Share on Facebook Share via WhatsApp Share via Email Youth volunteers sort through medical donations China Family Planning Association The China Youth Network set up a donation working group and with the support of the China Family Planning Association and Hubei Family Planning Association, they received donations of menstruation supplies, and medical equipment. By March they had successfully donated 5,680 sanitary towels, 3,280 medical face shields, 1,200 hand disinfectants, 925 disposable beddings, 500 air disinfectants and some medical machines to 87 hospitals in Hubei Province. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Erbol, 17, is the chair of the youth committee of the Issyk-Kul branch Reproductive Health Alliance of Kyrgyzstan “At the present time we are using Instagram with detailed information about our organization and articles on sexual and reproductive health issues. We found new technologies and approaches to organize online meetings with the youth volunteers and planning of future branch activities through Zoom. It is planned to consider additional options in creation of channels on Telegram and Twitter because they are very popular among young people.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Healthcare providers put together hygiene kits for local communities Family Planning Association of Sri Lanka FPA Sri Lanka assembled 5,000 hygiene kits to be distributed to promote and enable frequent hand washing, personal hygiene and menstrual hygiene among vulnerable women and girls with limited incomes. These women and girls include mothers, widows with children, families who care for a member living with a disability, and women and girls living in slums during lockdown in high-risk areas for COVID-19. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Healthcare outreach teams distribute contraception and hygiene kits Family Health Association Iran “To reduce the number of visits to our clinics, we made some changes in the way we deliver services. We provide counselling services through online systems and creating different groups for clients to provide online educational training about COVID-19 for them, as well as some components of life skills and SGBV. For the vulnerable groups including sex workers and substance users we distribute contraceptives, COVID-19 preventive packages, and food through the outreach team instead of static clinics.”Zahra Fathi, Executive Director of the Family Health Association Iran (FHA Iran) Share on Twitter Share on Facebook Share via WhatsApp Share via Email Outreach teams sanitize people's homes in remote communities Sudan Family Planning Association Staff at the Sudan Family Planning Association conduct outreach work in local communities, including offering to sanitize people's homes. Remote areas in Sudan with no medical services will be affected with discontinued mobile clinics services. Access to all family planning, antenatal care, and postnatal care services will be affected due to restricted movement. Sudan, as will many other countries, will be impacted by any decrease in activity in the supply chain for healthcare supplies. Share on Twitter Share on Facebook Share via WhatsApp Share via Email A watercolour entry for a social media art competition Santé Sexuelle Suisse/Sexuelle Gesundheit Schweiz “With our Youth Network we created an artistic competition on our FB and Instagram platforms on issues such as masturbation, menstruation, coming out, female genitalia, pornography. The aim is to enhance creativity and make young people reflect about sexual and reproductive health and rights in a creative way during the corona pandemic. The aim was also to offer something fun and positive in this difficult time.”Noemi, 24, is the co-founder and coordinator of Santé Sexuelle Suisse/Sexuelle Gesundheit Schweiz's youth network. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Volunteers make hand sanitizer kits at a SFPA clinic. Syria Family Planning Association When the lockdown was announced SFPA had to stop running their mobile clinics but recently resumed this service. To keep the health facilities open they implemented a new shift rota for staff. The clinics are also following an extremely high-standard of sterilization procedures in all facilities to reduce the risk of catching or spreading coronavirus. SFPA started using social media to spread information on COVID-19. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Belmar Franceshi, Executive Director Asociacion Civil de Planificacion Familiar “The work we do is very important – despite being in our homes, we continue to work, research and look for alternatives to serve the hundreds of people who daily seek our services. It is one more challenge that we must face and will strengthen our actions, our interventions and the activities we carry out daily with communities, women and girls.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Enusring client and staff safety with PPE Family Planning Organisation of the Philippines The Family Planning Organisation of the Philippines (FPOP) is working safely with PPE equipment to ensure uninterrupted access to antenatal care and family planning methods for women and young girls through their clinics. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Delivering essential healthcare to women Family Planning Association of Nepal With PPE and hygiene kits FPAN’s healthcare providers can safely engage in delivering essential care to communities, including counselling, contraception methods, safe abortion, HIV/STI care, obstetrics and gynaecology care and sexual and gender-based violence support. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Reaching local communities Family Health Association Bangladesh FPAB key health workers have continued to provide essential sexual and reproductive healthcare in local communities during COVID-19. Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 19 April 2024
In pictures: Resilience and innovation in the face of COVID-19
Healthcare providers in their PPE Lebanon Association for Family Health (SALAMA) “After the extension of the general mobilization and in order to provide the services to the most in need population, we decided to re-open the clinic. For this purpose, we are developing a plan for the work during the next weeks, taking into consideration the protocols and procedures taken in Lebanon. This will include an isolation room before the consultation and an assessment of the patient’s status and any symptoms that may relate to the coronavirus. In addition to all the precaution procedures including separation, our clinic was sterilized by a specialized company.”Lina Sabra, the Executive Director of the Lebanese Association for Family Health (SALAMA) Share on Twitter Share on Facebook Share via WhatsApp Share via Email Youth volunteers sort through medical donations China Family Planning Association The China Youth Network set up a donation working group and with the support of the China Family Planning Association and Hubei Family Planning Association, they received donations of menstruation supplies, and medical equipment. By March they had successfully donated 5,680 sanitary towels, 3,280 medical face shields, 1,200 hand disinfectants, 925 disposable beddings, 500 air disinfectants and some medical machines to 87 hospitals in Hubei Province. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Erbol, 17, is the chair of the youth committee of the Issyk-Kul branch Reproductive Health Alliance of Kyrgyzstan “At the present time we are using Instagram with detailed information about our organization and articles on sexual and reproductive health issues. We found new technologies and approaches to organize online meetings with the youth volunteers and planning of future branch activities through Zoom. It is planned to consider additional options in creation of channels on Telegram and Twitter because they are very popular among young people.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Healthcare providers put together hygiene kits for local communities Family Planning Association of Sri Lanka FPA Sri Lanka assembled 5,000 hygiene kits to be distributed to promote and enable frequent hand washing, personal hygiene and menstrual hygiene among vulnerable women and girls with limited incomes. These women and girls include mothers, widows with children, families who care for a member living with a disability, and women and girls living in slums during lockdown in high-risk areas for COVID-19. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Healthcare outreach teams distribute contraception and hygiene kits Family Health Association Iran “To reduce the number of visits to our clinics, we made some changes in the way we deliver services. We provide counselling services through online systems and creating different groups for clients to provide online educational training about COVID-19 for them, as well as some components of life skills and SGBV. For the vulnerable groups including sex workers and substance users we distribute contraceptives, COVID-19 preventive packages, and food through the outreach team instead of static clinics.”Zahra Fathi, Executive Director of the Family Health Association Iran (FHA Iran) Share on Twitter Share on Facebook Share via WhatsApp Share via Email Outreach teams sanitize people's homes in remote communities Sudan Family Planning Association Staff at the Sudan Family Planning Association conduct outreach work in local communities, including offering to sanitize people's homes. Remote areas in Sudan with no medical services will be affected with discontinued mobile clinics services. Access to all family planning, antenatal care, and postnatal care services will be affected due to restricted movement. Sudan, as will many other countries, will be impacted by any decrease in activity in the supply chain for healthcare supplies. Share on Twitter Share on Facebook Share via WhatsApp Share via Email A watercolour entry for a social media art competition Santé Sexuelle Suisse/Sexuelle Gesundheit Schweiz “With our Youth Network we created an artistic competition on our FB and Instagram platforms on issues such as masturbation, menstruation, coming out, female genitalia, pornography. The aim is to enhance creativity and make young people reflect about sexual and reproductive health and rights in a creative way during the corona pandemic. The aim was also to offer something fun and positive in this difficult time.”Noemi, 24, is the co-founder and coordinator of Santé Sexuelle Suisse/Sexuelle Gesundheit Schweiz's youth network. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Volunteers make hand sanitizer kits at a SFPA clinic. Syria Family Planning Association When the lockdown was announced SFPA had to stop running their mobile clinics but recently resumed this service. To keep the health facilities open they implemented a new shift rota for staff. The clinics are also following an extremely high-standard of sterilization procedures in all facilities to reduce the risk of catching or spreading coronavirus. SFPA started using social media to spread information on COVID-19. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Belmar Franceshi, Executive Director Asociacion Civil de Planificacion Familiar “The work we do is very important – despite being in our homes, we continue to work, research and look for alternatives to serve the hundreds of people who daily seek our services. It is one more challenge that we must face and will strengthen our actions, our interventions and the activities we carry out daily with communities, women and girls.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Enusring client and staff safety with PPE Family Planning Organisation of the Philippines The Family Planning Organisation of the Philippines (FPOP) is working safely with PPE equipment to ensure uninterrupted access to antenatal care and family planning methods for women and young girls through their clinics. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Delivering essential healthcare to women Family Planning Association of Nepal With PPE and hygiene kits FPAN’s healthcare providers can safely engage in delivering essential care to communities, including counselling, contraception methods, safe abortion, HIV/STI care, obstetrics and gynaecology care and sexual and gender-based violence support. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Reaching local communities Family Health Association Bangladesh FPAB key health workers have continued to provide essential sexual and reproductive healthcare in local communities during COVID-19. Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 08 January 2021
"The movement helps girls to know their rights and their bodies"
My name is Fatoumata Yehiya Maiga. I’m 23-years-old, and I’m an IT specialist. I joined the Youth Action Movement at the end of 2018. The head of the movement in Mali is a friend of mine, and I met her before I knew she was the president. She invited me to their events and over time persuaded me to join. I watched them raising awareness about sexual and reproductive health, using sketches and speeches. I learnt a lot. Overcoming taboos I went home and talked about what I had seen and learnt with my family. In Africa, and even more so in the village where I come from in Gao, northern Mali, people don’t talk about these things. I wanted to take my sisters to the events, but every time I spoke about them my relatives would just say it was to teach girls to have sex, and that it’s taboo. That’s not what I believe. I think the movement helps girls, most of all, to know their sexual rights, their bodies, what to do and what not to do to stay healthy and safe. They don’t understand this concept. My family would say it was just a smokescreen to convince girls to get involved in something dirty. I have had to tell my younger cousins about their periods, for example, when they came from the village to live in the city. One of my cousins was so scared, and told me she was bleeding from her vagina and didn’t know why. We talk about managing periods in the Youth Action Movement, as well as how to manage cramps and feel better. The devastating impact of FGM But there was a much more important reason for me to join the movement. My parents are educated, so me and my sisters were never cut. I learned about female genital mutilation at a conference I attended in 2016. I didn’t know that there were different types of severity and ways that girls could be cut. I hadn’t understood quite how dangerous this practice is. Then, two years ago, I lost my friend Aïssata. She got married young, at 17. She struggled to conceive until she was 23. The day she gave birth, there were complications and she died. The doctors said that the excision was botched and that’s what killed her. From that day on, I decided I needed to teach all the girls in my community about how harmful this practice is for their health. I was so horrified by the way she died. Normally, girls in Mali are cut when they are three or four years old, though for some it’s done at birth. When they are older and get pregnant, I know they face the same challenges as every woman does giving birth, but they also live with the dangerous consequences of this unhealthy practice. The importance of talking openly The problem lies with the families. I want us, as a movement, to talk with the parents and explain to them how they can contribute to their children’s sexual health. I wish it were no longer a taboo between parents and their girls. But if we talk in such direct terms, they only see disobedience, and say that we are encouraging promiscuity. We need to talk to teenagers because they are already parents in many cases. They are the ones who decide to go through with cutting their daughters, or not. A lot of Mali is hard to reach though. We need travelling groups to go to those isolated rural areas and talk to people about sexual health. Pregnancy is the girl’s decision, and girls have a right to be healthy, and to choose their future.

| 19 April 2024
"The movement helps girls to know their rights and their bodies"
My name is Fatoumata Yehiya Maiga. I’m 23-years-old, and I’m an IT specialist. I joined the Youth Action Movement at the end of 2018. The head of the movement in Mali is a friend of mine, and I met her before I knew she was the president. She invited me to their events and over time persuaded me to join. I watched them raising awareness about sexual and reproductive health, using sketches and speeches. I learnt a lot. Overcoming taboos I went home and talked about what I had seen and learnt with my family. In Africa, and even more so in the village where I come from in Gao, northern Mali, people don’t talk about these things. I wanted to take my sisters to the events, but every time I spoke about them my relatives would just say it was to teach girls to have sex, and that it’s taboo. That’s not what I believe. I think the movement helps girls, most of all, to know their sexual rights, their bodies, what to do and what not to do to stay healthy and safe. They don’t understand this concept. My family would say it was just a smokescreen to convince girls to get involved in something dirty. I have had to tell my younger cousins about their periods, for example, when they came from the village to live in the city. One of my cousins was so scared, and told me she was bleeding from her vagina and didn’t know why. We talk about managing periods in the Youth Action Movement, as well as how to manage cramps and feel better. The devastating impact of FGM But there was a much more important reason for me to join the movement. My parents are educated, so me and my sisters were never cut. I learned about female genital mutilation at a conference I attended in 2016. I didn’t know that there were different types of severity and ways that girls could be cut. I hadn’t understood quite how dangerous this practice is. Then, two years ago, I lost my friend Aïssata. She got married young, at 17. She struggled to conceive until she was 23. The day she gave birth, there were complications and she died. The doctors said that the excision was botched and that’s what killed her. From that day on, I decided I needed to teach all the girls in my community about how harmful this practice is for their health. I was so horrified by the way she died. Normally, girls in Mali are cut when they are three or four years old, though for some it’s done at birth. When they are older and get pregnant, I know they face the same challenges as every woman does giving birth, but they also live with the dangerous consequences of this unhealthy practice. The importance of talking openly The problem lies with the families. I want us, as a movement, to talk with the parents and explain to them how they can contribute to their children’s sexual health. I wish it were no longer a taboo between parents and their girls. But if we talk in such direct terms, they only see disobedience, and say that we are encouraging promiscuity. We need to talk to teenagers because they are already parents in many cases. They are the ones who decide to go through with cutting their daughters, or not. A lot of Mali is hard to reach though. We need travelling groups to go to those isolated rural areas and talk to people about sexual health. Pregnancy is the girl’s decision, and girls have a right to be healthy, and to choose their future.

| 23 September 2020
In pictures: Innovating during COVID-19
Women around the world have faced multiple barriers to accessing safe abortion care during the COVID-19 pandemic including the de-prioritization of sexual and reproductive healthcare, overwhelmed health systems and restrictions on movement. The COVID-19 crisis has sparked innovation among IPPF Member Associations who responded swiftly by developing new approaches to reach women with safe abortion care including telemedicine and home-based provision of medical abortion. Strong evidence generated from this work supports the continuation and strengthening of these approaches beyond the end of the pandemic. Cameroon Cameroon National Planning Association for Family Welfare (CAMNAFAW) To ensure that quality abortion care can be provided to women during travel restrictions, CAMNAFAW’s service providers travel to partner clinics in underserved areas and to clients’ homes to provide medical and surgical abortion care. This model of taking safe abortion care closer to women will continue even with easing of travel restrictions, as this has been found to be an effective and acceptable approach to increasing access.Photo: IPPF/Xaume Olleros/Cameroon Share on Twitter Share on Facebook Share via WhatsApp Share via Email Guinea Association Guinéenne pour le Bien-Etre Familial (AGBEF) Building on lessons learned during the Ebola crisis in Guinea, AGBEF quickly took measures to prevent infection in its clinics to continue providing sexual and reproductive healthcare, including surgical and medical abortion, in a safe environment. AGBEF donated protective materials to communities, including hand-washing stations, face masks and antibacterial gel, alongside messaging on infection prevention. This community visibility reassures clients they can safely attend AGBEF clinics for abortion and contraceptive care.Photo: AGBEF/Guinea Share on Twitter Share on Facebook Share via WhatsApp Share via Email India Family Planning Association of India (FPA India) FPA India and partners advocated to have sexual and reproductive healthcare, including abortion, recognized as essential by the government, which meant FPA India could continue healthcare delivery during the national lockdown. To reduce in-person clinic visits, FPA India established teleconsultation and counselling for abortion care, and is continuing to provide in-clinic care for both medical and surgical abortion. Photo: IPPF/Alison Joyce/India Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nepal Family Planning Association of Nepal (FPAN) FPAN and partners advocated for interim approval of home provision of medical abortion and telemedicine for abortion counselling during COVID-19. FPAN is now implementing these approaches, ensuring continued access to abortion care in Nepal, where many people live in remote locations with limited mobility, which has been further restricted by COVID-19 lockdowns. Photo: FPAN/Nepal Share on Twitter Share on Facebook Share via WhatsApp Share via Email Pakistan Rahnuma – Family Planning Association of Pakistan (Rahnuma-FPAP) Rahnuma-FPAP and partners successfully advocated for the government to class sexual and reproductive healthcare as ‘essential’, which enabled the team to continue providing post-abortion care during the pandemic. Rahnuma-FPAP expanded its telemedicine and home-based provision for menstrual regulation counselling and post-abortion care. These new approaches have ensured continued access to services for clients unable to reach clinics.Photo: Rahnuma-FPAP/Pakistan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Palestine Palestinian Family Planning and Protection Association (PFPPA) In response to the government-mandated closure of its clinics, PFPPA quickly established a toll-free call centre which provides consultations, counselling, referrals and follow-up, including consultation for abortion care through a harm reduction approach, ensuring that women are provided with accurate information. Due to its success, PFPPA is exploring options for continuing this healthcare delivery model beyond the pandemic, with the aim of keeping it free of charge for users.Photo: SAAF/Samar Hazboun/Palestine Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sudan Sudan Family Planning Association (SFPA) Following a nation-wide shutdown in April, SFPA established a call centre to increase access to healthcare, including abortion and contraceptive counselling and referrals. An unexpected outcome of the new call centre is that it has reached an increased number of young women who regularly call to discuss their reproductive health and rights. SFPA is working towards institutionalizing this model for continuation beyond the pandemic.Photo: SFPA/Sudan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Togo Association Togolaise pour le Bien-Etre Familial (ATBEF) ATBEF adapted its mobile application ‘Infos Ado Jeunes’, adding a toll-free teleconsultation service for young clients to use to access abortion consultations and pre- and post-abortion counselling. This app has given young clients ongoing access to care when they face challenges travelling to clinics. It has also eased overall client flow in clinics at a time when social distancing is being implemented.Photo: ATBEF/Togo Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 19 April 2024
In pictures: Innovating during COVID-19
Women around the world have faced multiple barriers to accessing safe abortion care during the COVID-19 pandemic including the de-prioritization of sexual and reproductive healthcare, overwhelmed health systems and restrictions on movement. The COVID-19 crisis has sparked innovation among IPPF Member Associations who responded swiftly by developing new approaches to reach women with safe abortion care including telemedicine and home-based provision of medical abortion. Strong evidence generated from this work supports the continuation and strengthening of these approaches beyond the end of the pandemic. Cameroon Cameroon National Planning Association for Family Welfare (CAMNAFAW) To ensure that quality abortion care can be provided to women during travel restrictions, CAMNAFAW’s service providers travel to partner clinics in underserved areas and to clients’ homes to provide medical and surgical abortion care. This model of taking safe abortion care closer to women will continue even with easing of travel restrictions, as this has been found to be an effective and acceptable approach to increasing access.Photo: IPPF/Xaume Olleros/Cameroon Share on Twitter Share on Facebook Share via WhatsApp Share via Email Guinea Association Guinéenne pour le Bien-Etre Familial (AGBEF) Building on lessons learned during the Ebola crisis in Guinea, AGBEF quickly took measures to prevent infection in its clinics to continue providing sexual and reproductive healthcare, including surgical and medical abortion, in a safe environment. AGBEF donated protective materials to communities, including hand-washing stations, face masks and antibacterial gel, alongside messaging on infection prevention. This community visibility reassures clients they can safely attend AGBEF clinics for abortion and contraceptive care.Photo: AGBEF/Guinea Share on Twitter Share on Facebook Share via WhatsApp Share via Email India Family Planning Association of India (FPA India) FPA India and partners advocated to have sexual and reproductive healthcare, including abortion, recognized as essential by the government, which meant FPA India could continue healthcare delivery during the national lockdown. To reduce in-person clinic visits, FPA India established teleconsultation and counselling for abortion care, and is continuing to provide in-clinic care for both medical and surgical abortion. Photo: IPPF/Alison Joyce/India Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nepal Family Planning Association of Nepal (FPAN) FPAN and partners advocated for interim approval of home provision of medical abortion and telemedicine for abortion counselling during COVID-19. FPAN is now implementing these approaches, ensuring continued access to abortion care in Nepal, where many people live in remote locations with limited mobility, which has been further restricted by COVID-19 lockdowns. Photo: FPAN/Nepal Share on Twitter Share on Facebook Share via WhatsApp Share via Email Pakistan Rahnuma – Family Planning Association of Pakistan (Rahnuma-FPAP) Rahnuma-FPAP and partners successfully advocated for the government to class sexual and reproductive healthcare as ‘essential’, which enabled the team to continue providing post-abortion care during the pandemic. Rahnuma-FPAP expanded its telemedicine and home-based provision for menstrual regulation counselling and post-abortion care. These new approaches have ensured continued access to services for clients unable to reach clinics.Photo: Rahnuma-FPAP/Pakistan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Palestine Palestinian Family Planning and Protection Association (PFPPA) In response to the government-mandated closure of its clinics, PFPPA quickly established a toll-free call centre which provides consultations, counselling, referrals and follow-up, including consultation for abortion care through a harm reduction approach, ensuring that women are provided with accurate information. Due to its success, PFPPA is exploring options for continuing this healthcare delivery model beyond the pandemic, with the aim of keeping it free of charge for users.Photo: SAAF/Samar Hazboun/Palestine Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sudan Sudan Family Planning Association (SFPA) Following a nation-wide shutdown in April, SFPA established a call centre to increase access to healthcare, including abortion and contraceptive counselling and referrals. An unexpected outcome of the new call centre is that it has reached an increased number of young women who regularly call to discuss their reproductive health and rights. SFPA is working towards institutionalizing this model for continuation beyond the pandemic.Photo: SFPA/Sudan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Togo Association Togolaise pour le Bien-Etre Familial (ATBEF) ATBEF adapted its mobile application ‘Infos Ado Jeunes’, adding a toll-free teleconsultation service for young clients to use to access abortion consultations and pre- and post-abortion counselling. This app has given young clients ongoing access to care when they face challenges travelling to clinics. It has also eased overall client flow in clinics at a time when social distancing is being implemented.Photo: ATBEF/Togo Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 13 August 2020
In pictures: Delivering healthcare to remote communities in Fiji
In early April 2020, the all too familiar destruction of a Tropical Cyclone (TC) – Harold – hit the Solomon Islands, Vanuatu, Fiji and Tonga. One of the worst affected areas was the Eastern part of Fiji. Through support by Department of Foreign Affairs and Trade (DFAT), our Member Association, Reproductive and Family Health Association of Fiji (RFHAF), was quick to respond ensuring access to essential sexual and reproductive healthcare for Kadavu’s women, girls, and vulnerable groups. Fiji's vulnerable coastline Fiji’s worst affected area was the Eastern part, with TC Harold bringing destructive storm force winds and storm surge. RFHAF focused its humanitarian response on the local Kadavu population. This remote area proves a challenge to reach for the team with supplies. Share on Twitter Share on Facebook Share via WhatsApp Share via Email RFHAF's humanitarian response team tackle rough terrain National travel restrictions - due to the current COVID-19 pandemic - on all inter island transfers has slowed the response in some areas, including Kadavu. The island of Kadavu is one of the least developed areas of Fiji, the main source of income is substance living (Yaqona). Transport around the island is difficult, with very few roads, no public water system or electricity. The humanitarian team from RFHAF travels by boat and then on foot. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Asenaca, client Kadavu, the biggest island in the Eastern division has the greatest population (10,897). 197 evacuation centres were activated in total, initially hosting over 6,240 people. Many are women of reproductive age, with an estimated 150 currently pregnant. Asenaca learns about breast cancer self-checks from RFHAF’s healthcare provider, Karo. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nasi, RFHAF healthcare provider The medical mobile team deliver a broad range of healthcare including contraception, information and counselling on sexual health, pregnancy, HIV and STI care and testing. RFHAF Team in Kadavu performing general health checks after TC Harold. Nasi administers a HPV shot to a client. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Kate, client Young women and girls are at the heart of RFHAF’s healthcare provision. Kate walks home with her dignity kit after a health check at the mobile clinic. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Karo, RFHAF healthcare worker RFHAF offers sexual and reproductive healthcare as well as counselling, and referrals for follow up care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Alidi, RFHAF healthcare worker The team ensures young people in the community are not forgotten and provide information and education on relationships and sexual health and rights. Alidi conducting a session with a local group of young people at Gasele, Kadavu.Photos ©IPPF/Rob Rickman/Fiji Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 19 April 2024
In pictures: Delivering healthcare to remote communities in Fiji
In early April 2020, the all too familiar destruction of a Tropical Cyclone (TC) – Harold – hit the Solomon Islands, Vanuatu, Fiji and Tonga. One of the worst affected areas was the Eastern part of Fiji. Through support by Department of Foreign Affairs and Trade (DFAT), our Member Association, Reproductive and Family Health Association of Fiji (RFHAF), was quick to respond ensuring access to essential sexual and reproductive healthcare for Kadavu’s women, girls, and vulnerable groups. Fiji's vulnerable coastline Fiji’s worst affected area was the Eastern part, with TC Harold bringing destructive storm force winds and storm surge. RFHAF focused its humanitarian response on the local Kadavu population. This remote area proves a challenge to reach for the team with supplies. Share on Twitter Share on Facebook Share via WhatsApp Share via Email RFHAF's humanitarian response team tackle rough terrain National travel restrictions - due to the current COVID-19 pandemic - on all inter island transfers has slowed the response in some areas, including Kadavu. The island of Kadavu is one of the least developed areas of Fiji, the main source of income is substance living (Yaqona). Transport around the island is difficult, with very few roads, no public water system or electricity. The humanitarian team from RFHAF travels by boat and then on foot. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Asenaca, client Kadavu, the biggest island in the Eastern division has the greatest population (10,897). 197 evacuation centres were activated in total, initially hosting over 6,240 people. Many are women of reproductive age, with an estimated 150 currently pregnant. Asenaca learns about breast cancer self-checks from RFHAF’s healthcare provider, Karo. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nasi, RFHAF healthcare provider The medical mobile team deliver a broad range of healthcare including contraception, information and counselling on sexual health, pregnancy, HIV and STI care and testing. RFHAF Team in Kadavu performing general health checks after TC Harold. Nasi administers a HPV shot to a client. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Kate, client Young women and girls are at the heart of RFHAF’s healthcare provision. Kate walks home with her dignity kit after a health check at the mobile clinic. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Karo, RFHAF healthcare worker RFHAF offers sexual and reproductive healthcare as well as counselling, and referrals for follow up care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Alidi, RFHAF healthcare worker The team ensures young people in the community are not forgotten and provide information and education on relationships and sexual health and rights. Alidi conducting a session with a local group of young people at Gasele, Kadavu.Photos ©IPPF/Rob Rickman/Fiji Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 16 July 2020
"Before, there was no safe abortion"
Rewda Kedir works as a midwife in a rural area of the Oromia region in southwest Ethiopia. Only 14% of married women are using any method of contraception here. The government hospital Rewda works in is supported to provide a full range of sexual and reproductive healthcare, which includes providing free contraceptives and comprehensive abortion care. In January 2017, the maternal healthcare clinic faced shortages of contraceptives after the US administration reactivated and expanded the Global Gag Rule, which does not allow any funding to go to organizations associated with providing abortion care. Fortunately in this case, the shortages only lasted a month due to the government of the Netherlands stepping in and matching lost funding. “Before, we had a shortage of contraceptive pills and emergency contraceptives. We would have to give people prescriptions and they would go to private clinics and where they had to pay," Rewda tells us. "When I first came to this clinic, there was a real shortage of people trained in family planning. I was the only one. Now there are many people trained on family planning, and when I’m not here, people can help." "There used to be a shortage of choice and alternatives, and now there are many. And the implant procedures are better because there are newer products that are much smaller so putting them in is less invasive.” Opening a dialogue on contraception The hospital has been providing medical abortions for six years. “Before, there was no safe abortion," says Rewda. She explains how people would go to 'traditional' healers and then come to the clinic with complications like sepsis, bleeding, anaemia and toxic shock. If they had complications or infections above nine weeks, Rewda and her colleagues would send them to Jimma, the regional capital. "Before, it was very difficult to persuade them to use family planning, and we had to have a lot of conversations. Now, they come 45 days after delivery to speak to us about this and get their babies immunised," she explains. "They want contraceptives to space out their children. Sometimes their husbands don’t like them coming to get family planning so we have to lock their appointment cards away. Their husbands want more children and they think that women who do not keep having their children will go with other men." "More kids, more wealth" Rewda tells us that they've used family counselling to try and persuade men to reconsider their ideas about contraception, by explaining to them that continuously giving birth under unsafe circumstances can affect a woman's health and might lead to maternal death, damage the uterus and lead to long-term complications. "Here, people believe that more kids means more wealth, and religion restricts family planning services. Before, they did not have good training on family planning and abortion. Now, women that have abortions get proper care and the counseling and education has improved. There are still unsafe abortions but they have really reduced. We used to see about 40 a year and now it’s one or two." However, problems still exist. "There are some complications, like irregular bleeding from some contraceptives," Rewda says, and that "women still face conflict with their husbands over family planning and sometimes have to go to court to fight this or divorce them.”

| 19 April 2024
"Before, there was no safe abortion"
Rewda Kedir works as a midwife in a rural area of the Oromia region in southwest Ethiopia. Only 14% of married women are using any method of contraception here. The government hospital Rewda works in is supported to provide a full range of sexual and reproductive healthcare, which includes providing free contraceptives and comprehensive abortion care. In January 2017, the maternal healthcare clinic faced shortages of contraceptives after the US administration reactivated and expanded the Global Gag Rule, which does not allow any funding to go to organizations associated with providing abortion care. Fortunately in this case, the shortages only lasted a month due to the government of the Netherlands stepping in and matching lost funding. “Before, we had a shortage of contraceptive pills and emergency contraceptives. We would have to give people prescriptions and they would go to private clinics and where they had to pay," Rewda tells us. "When I first came to this clinic, there was a real shortage of people trained in family planning. I was the only one. Now there are many people trained on family planning, and when I’m not here, people can help." "There used to be a shortage of choice and alternatives, and now there are many. And the implant procedures are better because there are newer products that are much smaller so putting them in is less invasive.” Opening a dialogue on contraception The hospital has been providing medical abortions for six years. “Before, there was no safe abortion," says Rewda. She explains how people would go to 'traditional' healers and then come to the clinic with complications like sepsis, bleeding, anaemia and toxic shock. If they had complications or infections above nine weeks, Rewda and her colleagues would send them to Jimma, the regional capital. "Before, it was very difficult to persuade them to use family planning, and we had to have a lot of conversations. Now, they come 45 days after delivery to speak to us about this and get their babies immunised," she explains. "They want contraceptives to space out their children. Sometimes their husbands don’t like them coming to get family planning so we have to lock their appointment cards away. Their husbands want more children and they think that women who do not keep having their children will go with other men." "More kids, more wealth" Rewda tells us that they've used family counselling to try and persuade men to reconsider their ideas about contraception, by explaining to them that continuously giving birth under unsafe circumstances can affect a woman's health and might lead to maternal death, damage the uterus and lead to long-term complications. "Here, people believe that more kids means more wealth, and religion restricts family planning services. Before, they did not have good training on family planning and abortion. Now, women that have abortions get proper care and the counseling and education has improved. There are still unsafe abortions but they have really reduced. We used to see about 40 a year and now it’s one or two." However, problems still exist. "There are some complications, like irregular bleeding from some contraceptives," Rewda says, and that "women still face conflict with their husbands over family planning and sometimes have to go to court to fight this or divorce them.”

| 18 June 2020
In pictures: Healthcare in the face of the climate crisis in Kiribati
Humanitarian crises Largely brought on by sudden onset and slow-onset natural disasters, humanitarian crises are increasingly prevalent in the Pacific. During responses to humanitarian crises in the Pacific, sexual and reproductive healthcare is often under-prioritised and under-resourced. As a result, women and girls of reproductive age and vulnerable and marginalized groups are disproportionately affected and facing increased health and psychosocial risks. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Fragile environments Low topography, rising sea levels and insufficient fresh water supply leaves Kiribati’s population vulnerable to the effects of the climate crisis. The fragility of the outer islands of Kiribati during natural disasters is compounded by their geographic isolation, which makes transportation and communication during post-disaster relief and response both expensive and difficult. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Coastal exposure The majority of the population of 115,000 people live a subsistence lifestyle. Communities are geographically dispersed across 33 atolls covering 3.5 million square kilometres in the central Pacific Ocean. The population and infrastructure within Kiribati are largely concentrated on the coast, where communities face increased exposure to climate threats and natural hazards such as tsunamis, earthquakes, king tides, flooding, droughts, and occasionally cyclones. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Takaria, leader and youth organizer in the Tebikenikua community Takaria will be running to be a Member of Parliament in Kiribati in 2020. “I assist the youth with family problems and family planning and disasters. In our community there are unforeseen pregnancies, domestic violence, and disasters such as high tide waters and strong winds, which can also affect this community. The Kiribati Family Health Association (KFHA) is the key point for us with outreach and training so people in this community know how to prevent and treat STIs, etc. They all know where the KFHA clinic is and that they can get counselling or services there. The problem now is you can’t survive with the sea rise levels. I want all members of my community to live better and have better health and peace.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Susan*, sex worker Susan receives care at the Kiribati Family Health Association (KFHA) including a pap smear. Susan*, 28, is a sex worker from the town of Betio on the main island of Kiribati. Originally from an outlying island, she moved into Tarawa to seek work. Unable to find employment that would fulfill her dream of sending money back to her two children, she was introduced to sex work. With other sex workers, she regularly travels out to the large cargo ships from China, Philippines and Korea anchored off the coast of Kiribati. Despite her new income, she still can’t speak with her children or see them due to the restrictive costs involved of travel between islands.*pseudonym Share on Twitter Share on Facebook Share via WhatsApp Share via Email Theta, 25-year-old mother and youth volunteer Theta is part of the Humanitarian Youth Club set up by the Kiribati Family Health Association in her village. “We face a lot of situations here, one of them is disasters and the second is unemployment and school drop out with our youth. I have helped the Humanitarian Youth Club to apply for financial grants from the Australian High Commission [for $1,000] I am recognized as the smartest member who can write in English. We have learned how to design a disaster plan for the community and share our ideas on sexual and reproductive issues such as STIs. We discuss what we can do for the next strong tide, where we can gather as a community and what we can do if even the maneabe (town hall) floods? If the tide and wind is too strong, we need to go to another safer place, such as another community’s town hall. For now, I want to enjoy the chance to be in our own beloved country. I won’t move until the majority have already left. I want my daughter to grow up in the same place I grew up in.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Beitau, youth volunteer Beitau is the Chairperson of the Humanitarian Youth Club. “I was lucky to be selected as Chairperson as the Humanitarian Youth Club. I feel like I get more respect from the community now I am in this position. I would love advanced training on leadership now, to further assist the club. As I am the Chairperson of the HYC, my main target is to help people during a disaster. I have attended training through KFHA. What I took from this is that when a disaster strikes, we have to do our best for pregnant women, small children and people with disabilities. They more vulnerable and less able to survive a disaster.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Abe, youth officer Abe was involved with KFHA since 2012. “I was inspired by what they KFHA was doing and the issues they were addressing that affects youth. I was surprised to see how many young people come to the clinic as they are affected by STIs, HIV and teenage pregnancy. The lack of education here is a big problem, most people here have a lot of children and yet can’t afford to send them to school. Sexual and reproductive health is our responsibility and we must talk about it with young people. Climate change affects many countries, but Kiribati is small and low lying. I used to go visit a very nice beach with a lot of nice trees and plants. Now, the trees are gone, and the waves have taken over, and the houses have disappeared so no one can build there. In my role as a youth worker and activist, I tell people to fight climate change: to grow more mangroves, to clean up the beach, because we love our Kiribati.”©IPPF/Hannah Maule-Ffinch/Kiribati Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 19 April 2024
In pictures: Healthcare in the face of the climate crisis in Kiribati
Humanitarian crises Largely brought on by sudden onset and slow-onset natural disasters, humanitarian crises are increasingly prevalent in the Pacific. During responses to humanitarian crises in the Pacific, sexual and reproductive healthcare is often under-prioritised and under-resourced. As a result, women and girls of reproductive age and vulnerable and marginalized groups are disproportionately affected and facing increased health and psychosocial risks. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Fragile environments Low topography, rising sea levels and insufficient fresh water supply leaves Kiribati’s population vulnerable to the effects of the climate crisis. The fragility of the outer islands of Kiribati during natural disasters is compounded by their geographic isolation, which makes transportation and communication during post-disaster relief and response both expensive and difficult. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Coastal exposure The majority of the population of 115,000 people live a subsistence lifestyle. Communities are geographically dispersed across 33 atolls covering 3.5 million square kilometres in the central Pacific Ocean. The population and infrastructure within Kiribati are largely concentrated on the coast, where communities face increased exposure to climate threats and natural hazards such as tsunamis, earthquakes, king tides, flooding, droughts, and occasionally cyclones. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Takaria, leader and youth organizer in the Tebikenikua community Takaria will be running to be a Member of Parliament in Kiribati in 2020. “I assist the youth with family problems and family planning and disasters. In our community there are unforeseen pregnancies, domestic violence, and disasters such as high tide waters and strong winds, which can also affect this community. The Kiribati Family Health Association (KFHA) is the key point for us with outreach and training so people in this community know how to prevent and treat STIs, etc. They all know where the KFHA clinic is and that they can get counselling or services there. The problem now is you can’t survive with the sea rise levels. I want all members of my community to live better and have better health and peace.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Susan*, sex worker Susan receives care at the Kiribati Family Health Association (KFHA) including a pap smear. Susan*, 28, is a sex worker from the town of Betio on the main island of Kiribati. Originally from an outlying island, she moved into Tarawa to seek work. Unable to find employment that would fulfill her dream of sending money back to her two children, she was introduced to sex work. With other sex workers, she regularly travels out to the large cargo ships from China, Philippines and Korea anchored off the coast of Kiribati. Despite her new income, she still can’t speak with her children or see them due to the restrictive costs involved of travel between islands.*pseudonym Share on Twitter Share on Facebook Share via WhatsApp Share via Email Theta, 25-year-old mother and youth volunteer Theta is part of the Humanitarian Youth Club set up by the Kiribati Family Health Association in her village. “We face a lot of situations here, one of them is disasters and the second is unemployment and school drop out with our youth. I have helped the Humanitarian Youth Club to apply for financial grants from the Australian High Commission [for $1,000] I am recognized as the smartest member who can write in English. We have learned how to design a disaster plan for the community and share our ideas on sexual and reproductive issues such as STIs. We discuss what we can do for the next strong tide, where we can gather as a community and what we can do if even the maneabe (town hall) floods? If the tide and wind is too strong, we need to go to another safer place, such as another community’s town hall. For now, I want to enjoy the chance to be in our own beloved country. I won’t move until the majority have already left. I want my daughter to grow up in the same place I grew up in.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Beitau, youth volunteer Beitau is the Chairperson of the Humanitarian Youth Club. “I was lucky to be selected as Chairperson as the Humanitarian Youth Club. I feel like I get more respect from the community now I am in this position. I would love advanced training on leadership now, to further assist the club. As I am the Chairperson of the HYC, my main target is to help people during a disaster. I have attended training through KFHA. What I took from this is that when a disaster strikes, we have to do our best for pregnant women, small children and people with disabilities. They more vulnerable and less able to survive a disaster.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Abe, youth officer Abe was involved with KFHA since 2012. “I was inspired by what they KFHA was doing and the issues they were addressing that affects youth. I was surprised to see how many young people come to the clinic as they are affected by STIs, HIV and teenage pregnancy. The lack of education here is a big problem, most people here have a lot of children and yet can’t afford to send them to school. Sexual and reproductive health is our responsibility and we must talk about it with young people. Climate change affects many countries, but Kiribati is small and low lying. I used to go visit a very nice beach with a lot of nice trees and plants. Now, the trees are gone, and the waves have taken over, and the houses have disappeared so no one can build there. In my role as a youth worker and activist, I tell people to fight climate change: to grow more mangroves, to clean up the beach, because we love our Kiribati.”©IPPF/Hannah Maule-Ffinch/Kiribati Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 04 June 2020
In pictures: Resilience and innovation in the face of COVID-19
Healthcare providers in their PPE Lebanon Association for Family Health (SALAMA) “After the extension of the general mobilization and in order to provide the services to the most in need population, we decided to re-open the clinic. For this purpose, we are developing a plan for the work during the next weeks, taking into consideration the protocols and procedures taken in Lebanon. This will include an isolation room before the consultation and an assessment of the patient’s status and any symptoms that may relate to the coronavirus. In addition to all the precaution procedures including separation, our clinic was sterilized by a specialized company.”Lina Sabra, the Executive Director of the Lebanese Association for Family Health (SALAMA) Share on Twitter Share on Facebook Share via WhatsApp Share via Email Youth volunteers sort through medical donations China Family Planning Association The China Youth Network set up a donation working group and with the support of the China Family Planning Association and Hubei Family Planning Association, they received donations of menstruation supplies, and medical equipment. By March they had successfully donated 5,680 sanitary towels, 3,280 medical face shields, 1,200 hand disinfectants, 925 disposable beddings, 500 air disinfectants and some medical machines to 87 hospitals in Hubei Province. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Erbol, 17, is the chair of the youth committee of the Issyk-Kul branch Reproductive Health Alliance of Kyrgyzstan “At the present time we are using Instagram with detailed information about our organization and articles on sexual and reproductive health issues. We found new technologies and approaches to organize online meetings with the youth volunteers and planning of future branch activities through Zoom. It is planned to consider additional options in creation of channels on Telegram and Twitter because they are very popular among young people.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Healthcare providers put together hygiene kits for local communities Family Planning Association of Sri Lanka FPA Sri Lanka assembled 5,000 hygiene kits to be distributed to promote and enable frequent hand washing, personal hygiene and menstrual hygiene among vulnerable women and girls with limited incomes. These women and girls include mothers, widows with children, families who care for a member living with a disability, and women and girls living in slums during lockdown in high-risk areas for COVID-19. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Healthcare outreach teams distribute contraception and hygiene kits Family Health Association Iran “To reduce the number of visits to our clinics, we made some changes in the way we deliver services. We provide counselling services through online systems and creating different groups for clients to provide online educational training about COVID-19 for them, as well as some components of life skills and SGBV. For the vulnerable groups including sex workers and substance users we distribute contraceptives, COVID-19 preventive packages, and food through the outreach team instead of static clinics.”Zahra Fathi, Executive Director of the Family Health Association Iran (FHA Iran) Share on Twitter Share on Facebook Share via WhatsApp Share via Email Outreach teams sanitize people's homes in remote communities Sudan Family Planning Association Staff at the Sudan Family Planning Association conduct outreach work in local communities, including offering to sanitize people's homes. Remote areas in Sudan with no medical services will be affected with discontinued mobile clinics services. Access to all family planning, antenatal care, and postnatal care services will be affected due to restricted movement. Sudan, as will many other countries, will be impacted by any decrease in activity in the supply chain for healthcare supplies. Share on Twitter Share on Facebook Share via WhatsApp Share via Email A watercolour entry for a social media art competition Santé Sexuelle Suisse/Sexuelle Gesundheit Schweiz “With our Youth Network we created an artistic competition on our FB and Instagram platforms on issues such as masturbation, menstruation, coming out, female genitalia, pornography. The aim is to enhance creativity and make young people reflect about sexual and reproductive health and rights in a creative way during the corona pandemic. The aim was also to offer something fun and positive in this difficult time.”Noemi, 24, is the co-founder and coordinator of Santé Sexuelle Suisse/Sexuelle Gesundheit Schweiz's youth network. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Volunteers make hand sanitizer kits at a SFPA clinic. Syria Family Planning Association When the lockdown was announced SFPA had to stop running their mobile clinics but recently resumed this service. To keep the health facilities open they implemented a new shift rota for staff. The clinics are also following an extremely high-standard of sterilization procedures in all facilities to reduce the risk of catching or spreading coronavirus. SFPA started using social media to spread information on COVID-19. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Belmar Franceshi, Executive Director Asociacion Civil de Planificacion Familiar “The work we do is very important – despite being in our homes, we continue to work, research and look for alternatives to serve the hundreds of people who daily seek our services. It is one more challenge that we must face and will strengthen our actions, our interventions and the activities we carry out daily with communities, women and girls.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Enusring client and staff safety with PPE Family Planning Organisation of the Philippines The Family Planning Organisation of the Philippines (FPOP) is working safely with PPE equipment to ensure uninterrupted access to antenatal care and family planning methods for women and young girls through their clinics. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Delivering essential healthcare to women Family Planning Association of Nepal With PPE and hygiene kits FPAN’s healthcare providers can safely engage in delivering essential care to communities, including counselling, contraception methods, safe abortion, HIV/STI care, obstetrics and gynaecology care and sexual and gender-based violence support. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Reaching local communities Family Health Association Bangladesh FPAB key health workers have continued to provide essential sexual and reproductive healthcare in local communities during COVID-19. Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 19 April 2024
In pictures: Resilience and innovation in the face of COVID-19
Healthcare providers in their PPE Lebanon Association for Family Health (SALAMA) “After the extension of the general mobilization and in order to provide the services to the most in need population, we decided to re-open the clinic. For this purpose, we are developing a plan for the work during the next weeks, taking into consideration the protocols and procedures taken in Lebanon. This will include an isolation room before the consultation and an assessment of the patient’s status and any symptoms that may relate to the coronavirus. In addition to all the precaution procedures including separation, our clinic was sterilized by a specialized company.”Lina Sabra, the Executive Director of the Lebanese Association for Family Health (SALAMA) Share on Twitter Share on Facebook Share via WhatsApp Share via Email Youth volunteers sort through medical donations China Family Planning Association The China Youth Network set up a donation working group and with the support of the China Family Planning Association and Hubei Family Planning Association, they received donations of menstruation supplies, and medical equipment. By March they had successfully donated 5,680 sanitary towels, 3,280 medical face shields, 1,200 hand disinfectants, 925 disposable beddings, 500 air disinfectants and some medical machines to 87 hospitals in Hubei Province. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Erbol, 17, is the chair of the youth committee of the Issyk-Kul branch Reproductive Health Alliance of Kyrgyzstan “At the present time we are using Instagram with detailed information about our organization and articles on sexual and reproductive health issues. We found new technologies and approaches to organize online meetings with the youth volunteers and planning of future branch activities through Zoom. It is planned to consider additional options in creation of channels on Telegram and Twitter because they are very popular among young people.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Healthcare providers put together hygiene kits for local communities Family Planning Association of Sri Lanka FPA Sri Lanka assembled 5,000 hygiene kits to be distributed to promote and enable frequent hand washing, personal hygiene and menstrual hygiene among vulnerable women and girls with limited incomes. These women and girls include mothers, widows with children, families who care for a member living with a disability, and women and girls living in slums during lockdown in high-risk areas for COVID-19. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Healthcare outreach teams distribute contraception and hygiene kits Family Health Association Iran “To reduce the number of visits to our clinics, we made some changes in the way we deliver services. We provide counselling services through online systems and creating different groups for clients to provide online educational training about COVID-19 for them, as well as some components of life skills and SGBV. For the vulnerable groups including sex workers and substance users we distribute contraceptives, COVID-19 preventive packages, and food through the outreach team instead of static clinics.”Zahra Fathi, Executive Director of the Family Health Association Iran (FHA Iran) Share on Twitter Share on Facebook Share via WhatsApp Share via Email Outreach teams sanitize people's homes in remote communities Sudan Family Planning Association Staff at the Sudan Family Planning Association conduct outreach work in local communities, including offering to sanitize people's homes. Remote areas in Sudan with no medical services will be affected with discontinued mobile clinics services. Access to all family planning, antenatal care, and postnatal care services will be affected due to restricted movement. Sudan, as will many other countries, will be impacted by any decrease in activity in the supply chain for healthcare supplies. Share on Twitter Share on Facebook Share via WhatsApp Share via Email A watercolour entry for a social media art competition Santé Sexuelle Suisse/Sexuelle Gesundheit Schweiz “With our Youth Network we created an artistic competition on our FB and Instagram platforms on issues such as masturbation, menstruation, coming out, female genitalia, pornography. The aim is to enhance creativity and make young people reflect about sexual and reproductive health and rights in a creative way during the corona pandemic. The aim was also to offer something fun and positive in this difficult time.”Noemi, 24, is the co-founder and coordinator of Santé Sexuelle Suisse/Sexuelle Gesundheit Schweiz's youth network. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Volunteers make hand sanitizer kits at a SFPA clinic. Syria Family Planning Association When the lockdown was announced SFPA had to stop running their mobile clinics but recently resumed this service. To keep the health facilities open they implemented a new shift rota for staff. The clinics are also following an extremely high-standard of sterilization procedures in all facilities to reduce the risk of catching or spreading coronavirus. SFPA started using social media to spread information on COVID-19. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Belmar Franceshi, Executive Director Asociacion Civil de Planificacion Familiar “The work we do is very important – despite being in our homes, we continue to work, research and look for alternatives to serve the hundreds of people who daily seek our services. It is one more challenge that we must face and will strengthen our actions, our interventions and the activities we carry out daily with communities, women and girls.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Enusring client and staff safety with PPE Family Planning Organisation of the Philippines The Family Planning Organisation of the Philippines (FPOP) is working safely with PPE equipment to ensure uninterrupted access to antenatal care and family planning methods for women and young girls through their clinics. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Delivering essential healthcare to women Family Planning Association of Nepal With PPE and hygiene kits FPAN’s healthcare providers can safely engage in delivering essential care to communities, including counselling, contraception methods, safe abortion, HIV/STI care, obstetrics and gynaecology care and sexual and gender-based violence support. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Reaching local communities Family Health Association Bangladesh FPAB key health workers have continued to provide essential sexual and reproductive healthcare in local communities during COVID-19. Share on Twitter Share on Facebook Share via WhatsApp Share via Email