Spotlight
A selection of stories from across the Federation

France, Germany, Poland, United Kingdom, United States, Colombia, India, Tunisia
Abortion Rights: Latest Decisions and Developments around the World
The global landscape of abortion rights continues to evolve in 2024, with new legislation and feminist movements fighting for better access. Let's take a trip around the world to see the latest developments.
Most Popular This Week
France, Germany, Poland, United Kingdom, United States, Colombia, India, Tunisia

Abortion Rights: Latest Decisions and Developments around the World
Over the past 30 years, more than

Palestine

In their own words: The people providing sexual and reproductive health care under bombardment in Gaza
Week after week, heavy Israeli bombardment from air, land, and sea, has continued across most of the Gaza Strip.
Vanuatu

When getting to the hospital is difficult, Vanuatu mobile outreach can save lives
In the mountains of Kumera on Tanna Island, Vanuatu, the village women of Kamahaul normally spend over 10,000 Vatu ($83 USD) to travel to the nearest hospital.
Vanuatu

Sex: changing minds and winning hearts in Tanna, Vanuatu
“Very traditional.” These two words are often used to describe the people of Tanna in Vanuatu, one of the most populated islands in the small country in the Pacific.
Vanuatu

Vanuatu cyclone response: The mental health toll on humanitarian providers
Girls and women from nearby villages flock to mobile health clinics set up by the Vanuatu Family Health Association (VFHA).
Cook Islands

Trans & Proud: Being Transgender in the Cook Islands
It’s a scene like many others around the world: a loving family pour over childhood photos, giggling and reminiscing about the memories.
Cook Islands

In Pictures: The activists who helped win LGBTI+ rights in the Cook Islands
The Cook Islands has removed a law that criminalizes homosexuality, in a huge victory for the local LGBTI+ community.
Filter our stories by:
- Albanian Center for Population and Development
- Association Burundaise pour le Bien-Etre Familial
- Association Malienne pour la Protection et la Promotion de la Famille
- Association Togolaise pour le Bien-Etre Familial
- Cameroon National Association for Family Welfare
- Family Guidance Association of Ethiopia
- Family Planning Association of Malawi
- Family Planning Association of Nepal
- Family Planning Association of Sri Lanka
- Foundation for the Promotion of Responsible Parenthood - Aruba
- Palestinian Family Planning and Protection Association (PFPPA)
- Planned Parenthood Association of Ghana
- Planned Parenthood Federation of Nigeria
- Reproductive & Family Health Association of Fiji
- Reproductive Health Association of Cambodia (RHAC)
- Reproductive Health Uganda
- Somaliland Family Health Association
- Vanuatu Family Health Association


| 22 January 2018
"We are non-judgemental; we embark on a mutual learning process."
It used to take Matilda Meke-Banda six hours on her motorbike along dirt roads to reach two remote districts and deliver sexual and reproductive health (SRH) services. In this part of southern Malawi, Machinga, family planning uptake is low, and the fertility rate, at 6.6, is the highest in the country. The Family Planning Association of Malawi, known as FPAM, runs a clinic in the town of Liwonde and it’s from here that Matilda travelled out six times a month. “We have established six watch groups, they are trained to address SRH issues in the community,” she explains. Luc Simon is the chair of one of those groups. “We teach about Family Planning,” he says. “We encourage parents and young people to go for HIV testing. We address forced early marriages, talk to parents and children to save a lot of young people.” And there are a lot of myths to dispel about family planning. Elizabeth Katunga is head of family planning in the district hospital in Machinga: “Family Planning is not very much accepted by the communities. Many women hide the use of contraceptives,” she says. “Injectables are most popular, easy to hide. We have cases here where husbands upon discovery of an implant take a knife and cut it out. It is not that people want big families per se but it is the misconceptions about contraceptives.” FPAM’s projects are based at the Youth Life clinic in Liwonde. The clinic offers integrated services: Family planning, HIV services, STI screening, cervical cancer screening and general healthcare (such as malaria). This joined-up approach has been effective says FPAM’s executive director Thoko Mbendera: “In government health facilities, you have different days, and long queues always, for family planning, for HIV, for general health, which is a challenge if the clinic is a 20 km walk away.There are privacy issues.” But now, FPAM’s services are being cut because of the Global Gag Rule (GGR), mobile clinics are grounded, and there are fears that much progress will be undone. Some of FPAM’s rural clients explain how the Watch Groups work in their community. “It starts with me as a man,” says group member George Mpemba. “We are examples on how to live with our wives. We are non-judgemental; we embark on a mutual learning process. Our meetings are not hearings, but a normal chat, there is laughing and talking. After the discussion we evaluate together and make an action plan.” Katherine, went to the group for help: “There was violence in my marriage; my husband forced himself on me even if I was tired from working in the field. When I complained there was trouble. He did not provide even the bedding. “He is a fisherman and he makes a lot of cash which he used to buy beer but nothing for us.I overheard a watch group meeting once and I realised there was a solution. They talked to him and made him realise that what he was doing was violence and against the law. It was ignorance.Things are better now, he brings money home, sex is consensual and sometimes he helps with household chores.”

| 19 April 2024
"We are non-judgemental; we embark on a mutual learning process."
It used to take Matilda Meke-Banda six hours on her motorbike along dirt roads to reach two remote districts and deliver sexual and reproductive health (SRH) services. In this part of southern Malawi, Machinga, family planning uptake is low, and the fertility rate, at 6.6, is the highest in the country. The Family Planning Association of Malawi, known as FPAM, runs a clinic in the town of Liwonde and it’s from here that Matilda travelled out six times a month. “We have established six watch groups, they are trained to address SRH issues in the community,” she explains. Luc Simon is the chair of one of those groups. “We teach about Family Planning,” he says. “We encourage parents and young people to go for HIV testing. We address forced early marriages, talk to parents and children to save a lot of young people.” And there are a lot of myths to dispel about family planning. Elizabeth Katunga is head of family planning in the district hospital in Machinga: “Family Planning is not very much accepted by the communities. Many women hide the use of contraceptives,” she says. “Injectables are most popular, easy to hide. We have cases here where husbands upon discovery of an implant take a knife and cut it out. It is not that people want big families per se but it is the misconceptions about contraceptives.” FPAM’s projects are based at the Youth Life clinic in Liwonde. The clinic offers integrated services: Family planning, HIV services, STI screening, cervical cancer screening and general healthcare (such as malaria). This joined-up approach has been effective says FPAM’s executive director Thoko Mbendera: “In government health facilities, you have different days, and long queues always, for family planning, for HIV, for general health, which is a challenge if the clinic is a 20 km walk away.There are privacy issues.” But now, FPAM’s services are being cut because of the Global Gag Rule (GGR), mobile clinics are grounded, and there are fears that much progress will be undone. Some of FPAM’s rural clients explain how the Watch Groups work in their community. “It starts with me as a man,” says group member George Mpemba. “We are examples on how to live with our wives. We are non-judgemental; we embark on a mutual learning process. Our meetings are not hearings, but a normal chat, there is laughing and talking. After the discussion we evaluate together and make an action plan.” Katherine, went to the group for help: “There was violence in my marriage; my husband forced himself on me even if I was tired from working in the field. When I complained there was trouble. He did not provide even the bedding. “He is a fisherman and he makes a lot of cash which he used to buy beer but nothing for us.I overheard a watch group meeting once and I realised there was a solution. They talked to him and made him realise that what he was doing was violence and against the law. It was ignorance.Things are better now, he brings money home, sex is consensual and sometimes he helps with household chores.”
| 19 January 2018
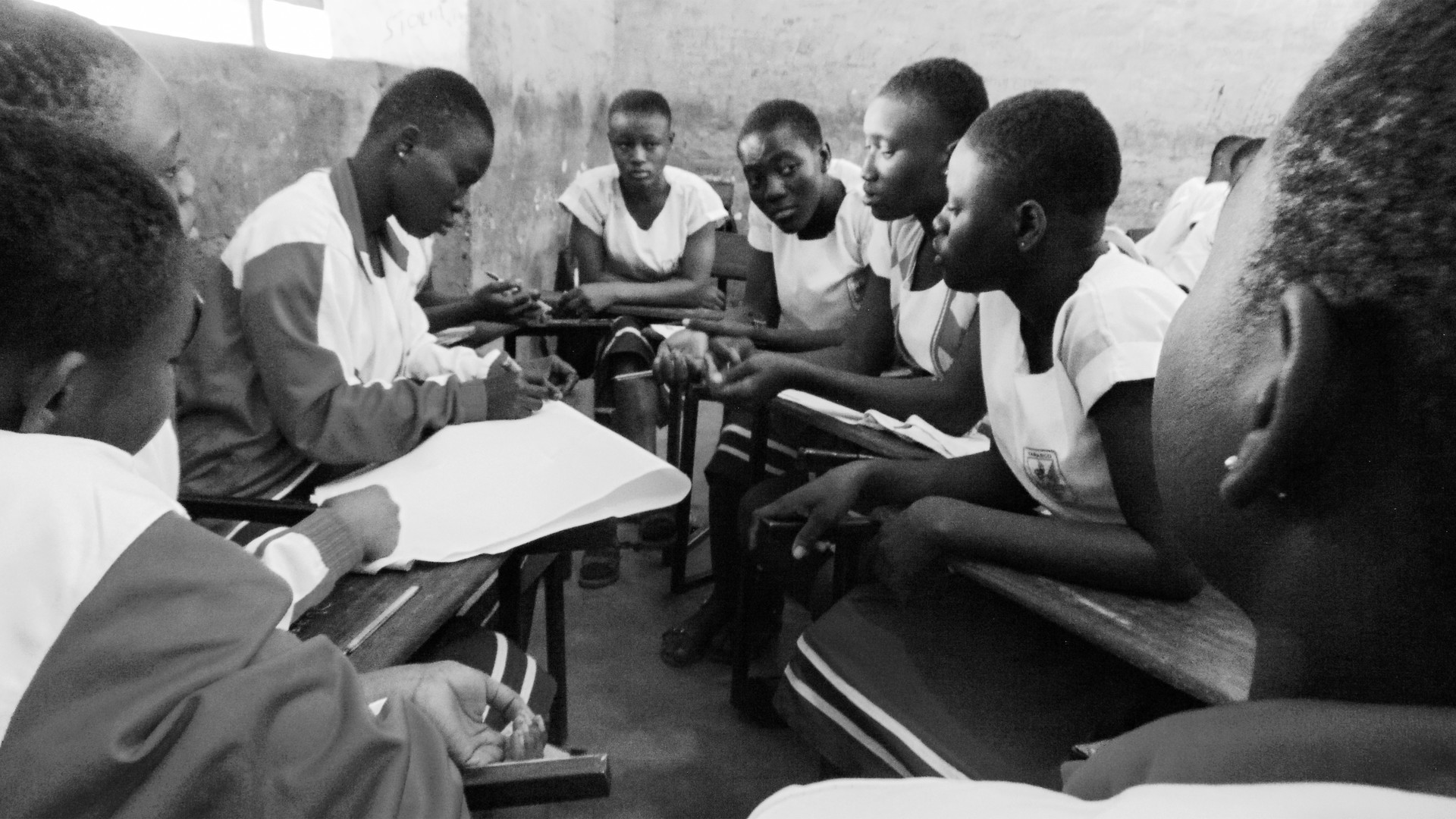
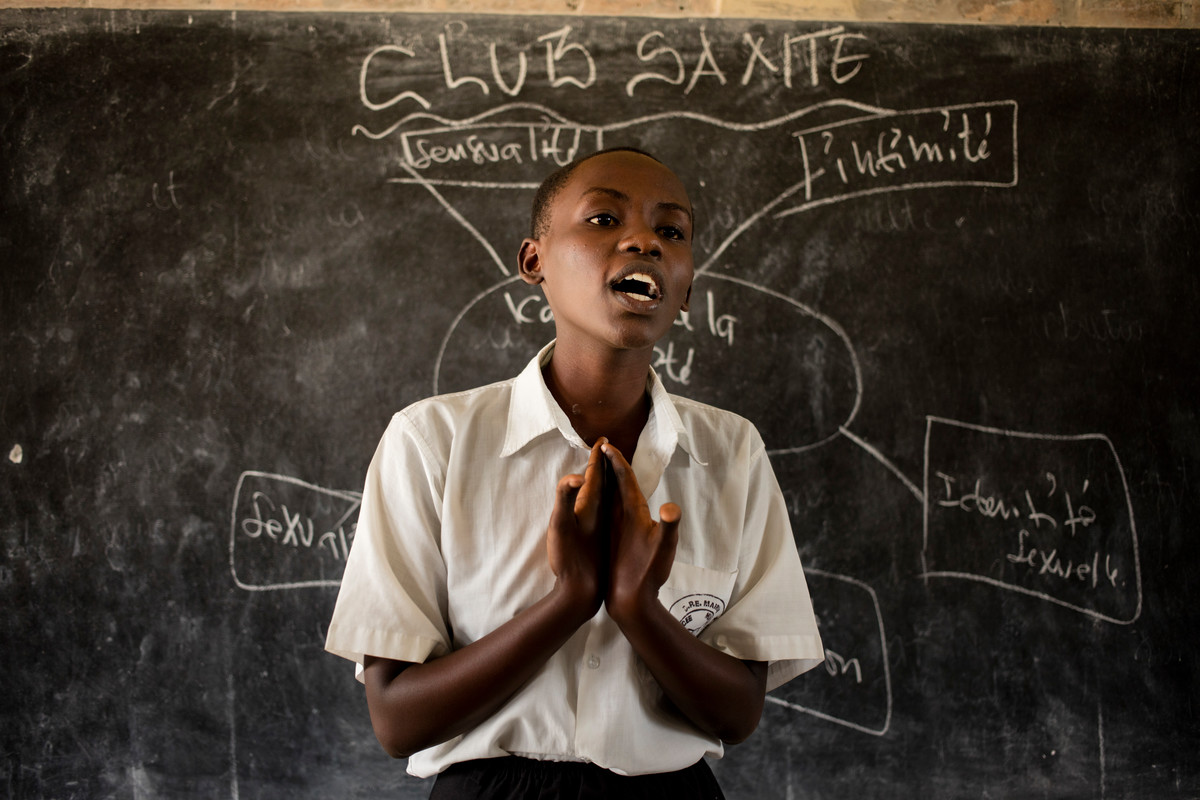
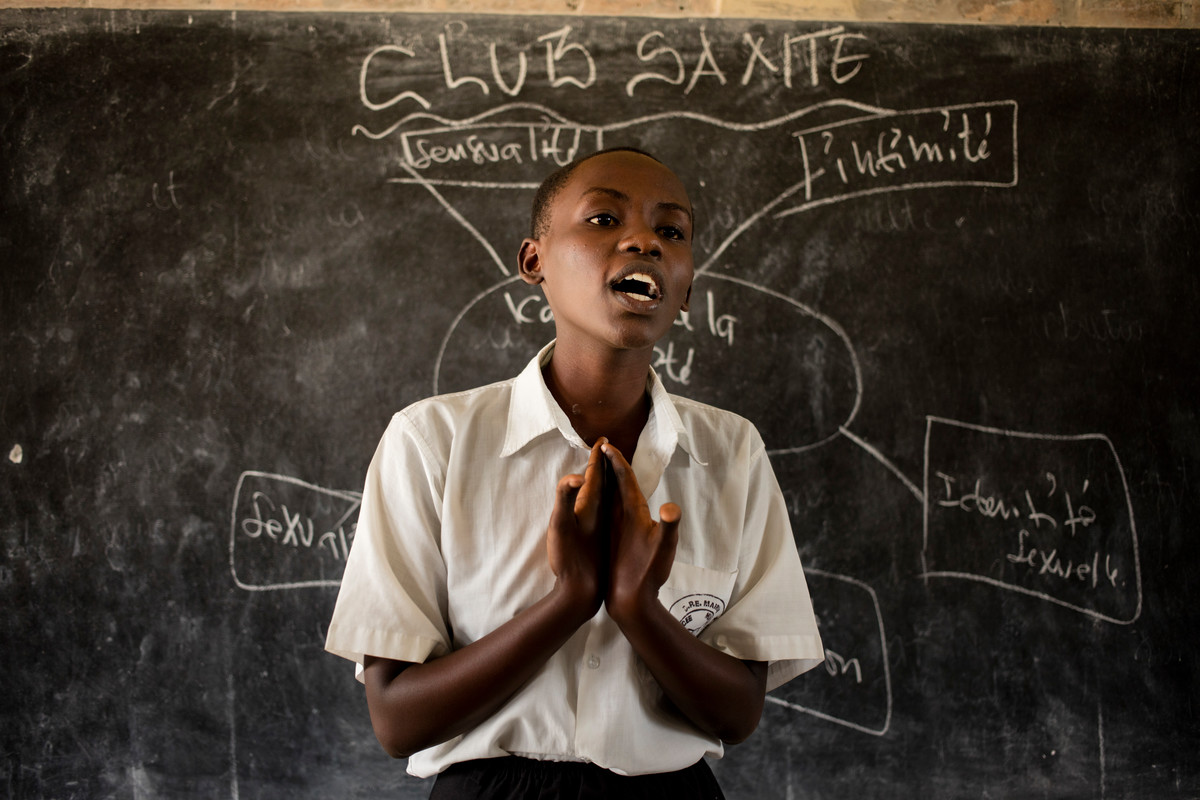
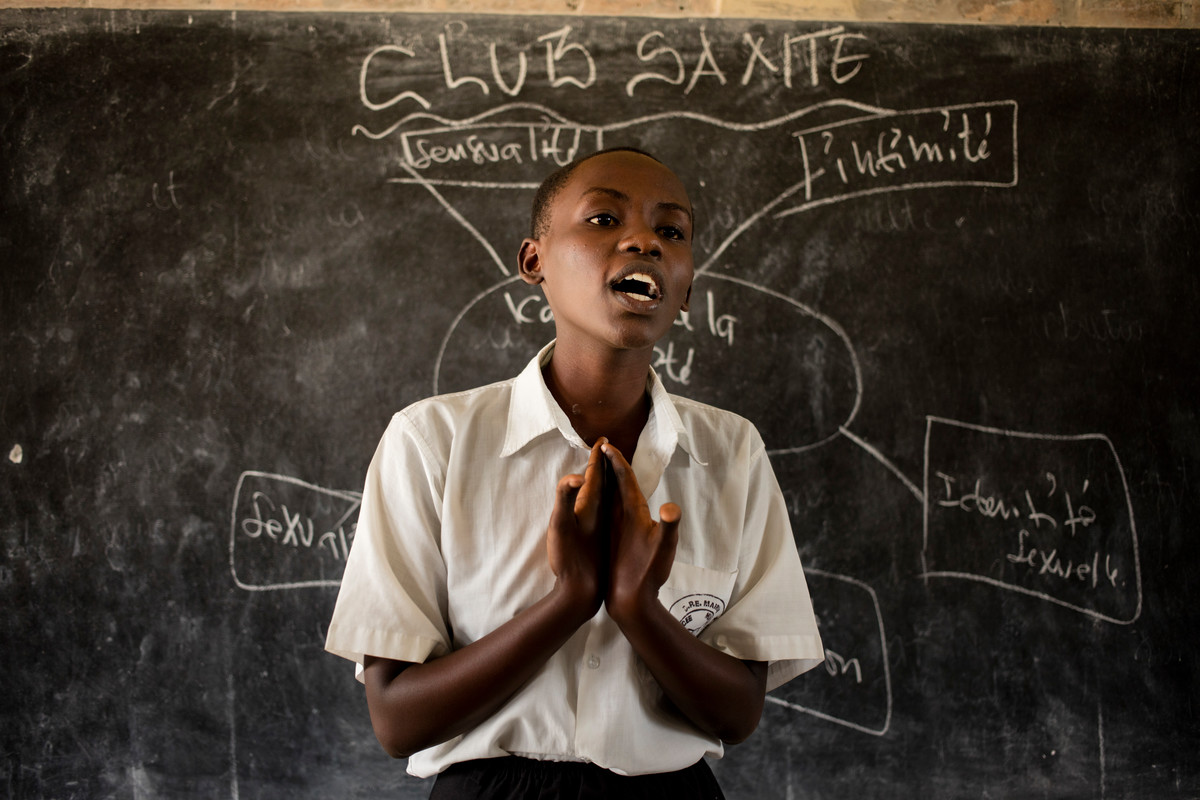
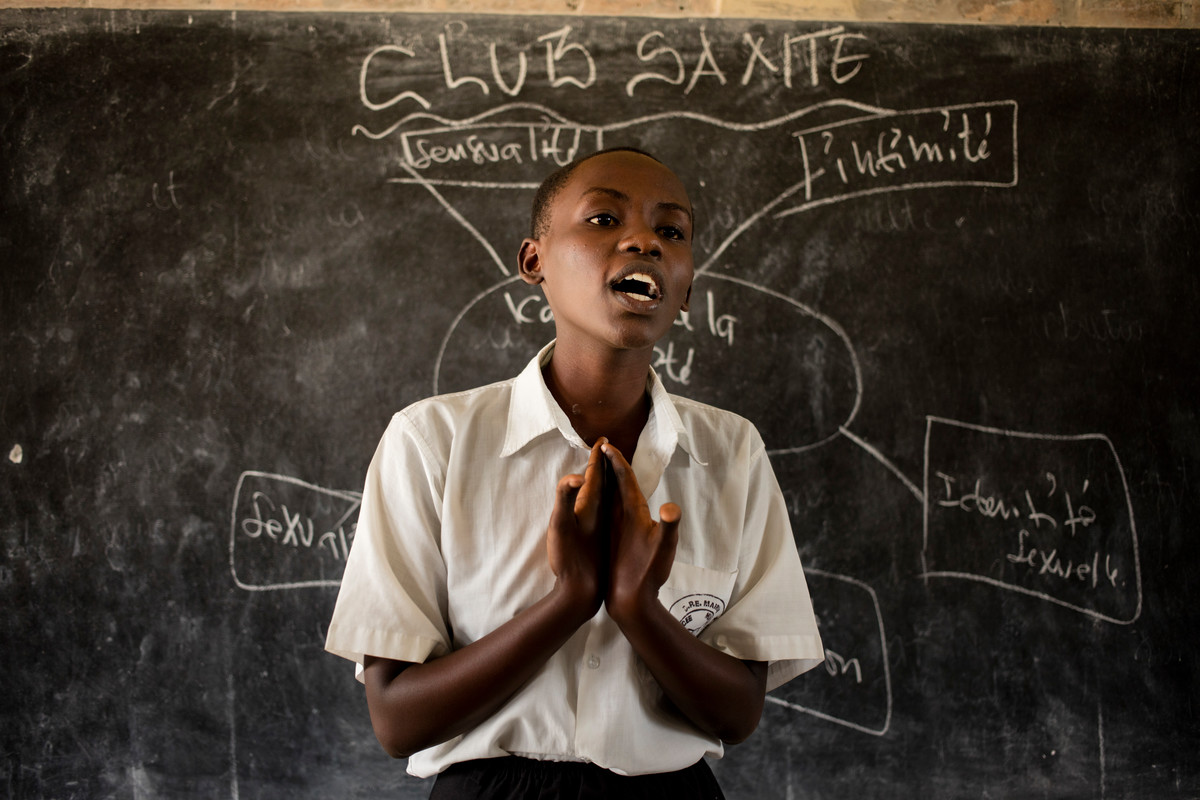
“I am afraid what will happen when there will be no more projects like this one"
On Friday afternoon in Municipal Lycee of Nyakabiga, Burundi, headmistress Chantal Keza is introducing her students to the medical staff from Association Burundaise pour le Bien-Etre Familial (ABUBEF). Peer educators at the school, trained by ABUBEF, will perform a short drama based around sexual health and will answer questions about contraception methods from students. One of the actresses is peer educator Ammande Berlyne Dushime. Ammande, who is 17 years old is one of three peer educators at the school. Ammande, together with her friends, perform their short drama on the stage based on a young girls quest for information on contraception. It ends on a positive note, with the girl receiving useful and correct information from a peer educator at her school. A story that could be a very real life scenario at her school. Peer programmes that trained Ammande, are under threat of closure due to the Global Gag rule. Ammande says, “I am afraid what will happen when there will be no more projects like this one. I am ready to go on with work as peer educator, but if there are not going to be regular visits by the medical stuff from the clinic, then we will have no one to seek information and advice from. I am just a teenager, I know so little. Not only I will lose my support, but also I will not be taken serious by my schoolmates. With such important topic like sexual education and contraception, I am not the authority. I can only show the right way to go. And this road leads to ABUBEF.” She says “As peer educator I am responsible for Saturday morning meetings at the clinic. We sing songs, play games, have fun and learn new things about sex education, contraception, HIV protection and others. Visiting the clinic is then very easy, and no student has to be afraid, that showing up at the clinic that treats HIV positive people, will ruin their reputation. Now they know that we can meet there openly, and undercover of these meetings seek for help, information, professional advice and contraception methods” Peer educator classes are a safe and open place for students to openly talk about their sexual health. The Global Gage Rule will force peer educator programmes like this to close due to lack of funding. Help us bridge the funding gap Learn more about the Global Gag Rule
| 19 April 2024
“I am afraid what will happen when there will be no more projects like this one"
On Friday afternoon in Municipal Lycee of Nyakabiga, Burundi, headmistress Chantal Keza is introducing her students to the medical staff from Association Burundaise pour le Bien-Etre Familial (ABUBEF). Peer educators at the school, trained by ABUBEF, will perform a short drama based around sexual health and will answer questions about contraception methods from students. One of the actresses is peer educator Ammande Berlyne Dushime. Ammande, who is 17 years old is one of three peer educators at the school. Ammande, together with her friends, perform their short drama on the stage based on a young girls quest for information on contraception. It ends on a positive note, with the girl receiving useful and correct information from a peer educator at her school. A story that could be a very real life scenario at her school. Peer programmes that trained Ammande, are under threat of closure due to the Global Gag rule. Ammande says, “I am afraid what will happen when there will be no more projects like this one. I am ready to go on with work as peer educator, but if there are not going to be regular visits by the medical stuff from the clinic, then we will have no one to seek information and advice from. I am just a teenager, I know so little. Not only I will lose my support, but also I will not be taken serious by my schoolmates. With such important topic like sexual education and contraception, I am not the authority. I can only show the right way to go. And this road leads to ABUBEF.” She says “As peer educator I am responsible for Saturday morning meetings at the clinic. We sing songs, play games, have fun and learn new things about sex education, contraception, HIV protection and others. Visiting the clinic is then very easy, and no student has to be afraid, that showing up at the clinic that treats HIV positive people, will ruin their reputation. Now they know that we can meet there openly, and undercover of these meetings seek for help, information, professional advice and contraception methods” Peer educator classes are a safe and open place for students to openly talk about their sexual health. The Global Gage Rule will force peer educator programmes like this to close due to lack of funding. Help us bridge the funding gap Learn more about the Global Gag Rule

| 17 November 2017
“The doctors have also been giving me advice on how to look after myself and the baby"
When garment worker Ny thought she might be pregnant with her first child, a home test kit quickly confirmed her suspicions. But the 23-year-old – who is originally from Takeo province but moved to Phnom Penh to take up a job in the garment industry – did not know where to go to seek prenatal care. After a cousin recommended that she visit a nearby Reproductive Health Association of Cambodia clinic, Ny took her relative’s advice – and has gone back eight times to date. “I come here every month to check on the baby,” she says, cradling her belly. “I had never been before I got pregnant.” During her visits to the medical clinic, Ny says, she has had a raft of standard tests and procedures as part of her prenatal care, including two ultrasounds, blood and urine tests, and vaccinations. “The doctors have also been giving me advice on how to look after myself and the baby [such as] to eat nutritious food and not to carry heavy things,” she says. As well as caring for the health of mother and unborn child, RHAC staff have also offered up valuable family planning information. “I did not know about how to plan to have children before I came to the clinic,” Ny says. “The doctors here told me that there are three different methods of [long-term] contraception: medication, an implant and an IUD.” Ny, who sews winter clothing at a factory while her husband also works in a nearby garment factory, says she was very glad to learn about her options. “This child was unplanned, but I don’t feel any regret because I had already been married for two years. But after having the baby I plan to use birth control, though I don’t know what method I will use,” she says. “I know that I don’t want to have another child straight away. It may be two or three years until I have the next one, as I want to wait until my family’s finances improve.”

| 19 April 2024
“The doctors have also been giving me advice on how to look after myself and the baby"
When garment worker Ny thought she might be pregnant with her first child, a home test kit quickly confirmed her suspicions. But the 23-year-old – who is originally from Takeo province but moved to Phnom Penh to take up a job in the garment industry – did not know where to go to seek prenatal care. After a cousin recommended that she visit a nearby Reproductive Health Association of Cambodia clinic, Ny took her relative’s advice – and has gone back eight times to date. “I come here every month to check on the baby,” she says, cradling her belly. “I had never been before I got pregnant.” During her visits to the medical clinic, Ny says, she has had a raft of standard tests and procedures as part of her prenatal care, including two ultrasounds, blood and urine tests, and vaccinations. “The doctors have also been giving me advice on how to look after myself and the baby [such as] to eat nutritious food and not to carry heavy things,” she says. As well as caring for the health of mother and unborn child, RHAC staff have also offered up valuable family planning information. “I did not know about how to plan to have children before I came to the clinic,” Ny says. “The doctors here told me that there are three different methods of [long-term] contraception: medication, an implant and an IUD.” Ny, who sews winter clothing at a factory while her husband also works in a nearby garment factory, says she was very glad to learn about her options. “This child was unplanned, but I don’t feel any regret because I had already been married for two years. But after having the baby I plan to use birth control, though I don’t know what method I will use,” she says. “I know that I don’t want to have another child straight away. It may be two or three years until I have the next one, as I want to wait until my family’s finances improve.”

| 16 November 2017
“When they don’t dare to ask questions about sensitive health topics, they don’t have the information they need"
Female workers, many of them undereducated migrants from rural areas, dominate the garment sector in Cambodia. And Propitious garment factory in Takhmao, a small city that lies just south of the capital Phnom Penh, is no exception. Women make up more than 90 percent of the factory’s workforce. Helping to oversee the 3,700-strong workforce is human resources manager Kouch Davy, who has worked at Propitious since it opened four years ago. Seeing a need to improve the workers’ sexual and reproductive health knowledge, she says she decided to work with the Reproductive Health Association of Cambodia (RHAC) because of its reputation for providing high-quality services. “I raised it in a management meeting, and the board was happy to explore it,” she says. For almost two years, trained staff from RHAC have been visiting the factory twice a month to meet with workers during their lunch break. They answer questions on topics ranging from birth control to STIs and abortion. The organisation has also provided training to the nurses who work in the factory’s on-site medical clinic. Davy says the factory’s female garment workers have changed as a result. “They are more open to asking questions about sexual health and they have also become more informed about the subject,” she says. “When they don’t dare to ask questions about sensitive health topics, they don’t have the information they need, so they tend to exaggerate their problems and ask for sick leave. But when they go to see an RHAC clinic and get proper treatment, there is less sick leave. “Now that they understand about contraception, there are fewer women getting pregnant and taking maternity leave, so that also helps with the workflow. ” Davy says the factory has seen requests for sick leave drop by an average of between 100 to 200 cases a month – and any decrease in absenteeism is a major boon for productivity. “The factory works like a chain: if just one person on the production line takes a day off, it affects the overall productivity,” she says. “And if a worker comes to work sick, they have problems concentrating.” Even Davy says she has gone to RHAC to seek medical care, visiting one of their clinics a few months ago for a breast examination. Meanwhile, the company that owns Propitious has extended its partnership with RHAC to a second factory in Phnom Penh. The firm has even requested that the NGO starts visiting its largest factory, which is situated in a rural province and has 10,000 workers, in the future.

| 19 April 2024
“When they don’t dare to ask questions about sensitive health topics, they don’t have the information they need"
Female workers, many of them undereducated migrants from rural areas, dominate the garment sector in Cambodia. And Propitious garment factory in Takhmao, a small city that lies just south of the capital Phnom Penh, is no exception. Women make up more than 90 percent of the factory’s workforce. Helping to oversee the 3,700-strong workforce is human resources manager Kouch Davy, who has worked at Propitious since it opened four years ago. Seeing a need to improve the workers’ sexual and reproductive health knowledge, she says she decided to work with the Reproductive Health Association of Cambodia (RHAC) because of its reputation for providing high-quality services. “I raised it in a management meeting, and the board was happy to explore it,” she says. For almost two years, trained staff from RHAC have been visiting the factory twice a month to meet with workers during their lunch break. They answer questions on topics ranging from birth control to STIs and abortion. The organisation has also provided training to the nurses who work in the factory’s on-site medical clinic. Davy says the factory’s female garment workers have changed as a result. “They are more open to asking questions about sexual health and they have also become more informed about the subject,” she says. “When they don’t dare to ask questions about sensitive health topics, they don’t have the information they need, so they tend to exaggerate their problems and ask for sick leave. But when they go to see an RHAC clinic and get proper treatment, there is less sick leave. “Now that they understand about contraception, there are fewer women getting pregnant and taking maternity leave, so that also helps with the workflow. ” Davy says the factory has seen requests for sick leave drop by an average of between 100 to 200 cases a month – and any decrease in absenteeism is a major boon for productivity. “The factory works like a chain: if just one person on the production line takes a day off, it affects the overall productivity,” she says. “And if a worker comes to work sick, they have problems concentrating.” Even Davy says she has gone to RHAC to seek medical care, visiting one of their clinics a few months ago for a breast examination. Meanwhile, the company that owns Propitious has extended its partnership with RHAC to a second factory in Phnom Penh. The firm has even requested that the NGO starts visiting its largest factory, which is situated in a rural province and has 10,000 workers, in the future.

| 16 November 2017
"During the pregnancy I was very worried”
Sophorn, a garment worker for the past decade, first visited a Reproductive Health Association of Cambodia (RHAC) clinic when she was pregnant with her first child. She returned for health checks each month until, at five months pregnant, she lost the baby. Her second pregnancy also resulted in a miscarriage, leaving her distraught. Then, she got pregnant a third time, in 2013. “I started to discuss with the doctors how to protect my child,” she says. “They gave me medication to strengthen my cervix, which I took for six months. In the seventh month, I gave birth prematurely.” Doctors told Sophorn that her baby girl was health, but she only weighed in at 1.7 kilograms. The infant was taken to a specialist children’s hospital, where she was cared for an additional two weeks. “During the pregnancy I was very worried,” Sophorn says. “I felt so happy when I finally delivered my child.” Her daughter was born without any complications is now a happy and healthy four years old. In initial stages of her third pregnancy, Sophorn’s friends told her that she would have to undergo surgery on her cervix or have injections to help her carry her baby to term, and doctors at a private clinic confirmed their suggestions. However, she decided to seek a second opinion at RHAC, where doctors instead gave her a prescription to strengthen her cervix. “When I heard I needed to have that surgery I was very scared, so I was relieved when the doctor at RHAC told me to take the medication instead,” she says. “While I was taking the medication I observed my body and any changes to it, so when I felt unwell I would go to the doctors and consult them, so I felt comfortable to continue taking it.” Sophorn also went for appointments at a government-run hospital, but found that their services were also lacking. “I told the doctors about losing my first and second babies, but they only weighed me and measured my stomach. There weren’t any more examinations or very much care,” she says. “When I went to RHAC they did so many examinations and had so many services, so I think it’s really better to go to RHAC for these kinds of services.” She estimates that during her third pregnancy, she had ten appointments at RHAC clinics at a cost of 40,000 to 60,000 riel (£7.40 to £11.15) each time. Compared to just 2,000 riel for an obstetrics appointment at the public hospital, the difference in cost is significant. “It’s expensive for me because my salary is little.” Despite the relatively high prices, Sophorn already knows where she will go for medical care in the future. “I want to have one more child, and I have already planned that when I decide to do it I will go to RHAC to get my cervix checked first,” she says. Until that day comes, Sophorn is taking the oral contraceptive after receiving advice about birth control from RHAC’s clinicians, with a midwife from the NGO making regular visits to the factory.

| 19 April 2024
"During the pregnancy I was very worried”
Sophorn, a garment worker for the past decade, first visited a Reproductive Health Association of Cambodia (RHAC) clinic when she was pregnant with her first child. She returned for health checks each month until, at five months pregnant, she lost the baby. Her second pregnancy also resulted in a miscarriage, leaving her distraught. Then, she got pregnant a third time, in 2013. “I started to discuss with the doctors how to protect my child,” she says. “They gave me medication to strengthen my cervix, which I took for six months. In the seventh month, I gave birth prematurely.” Doctors told Sophorn that her baby girl was health, but she only weighed in at 1.7 kilograms. The infant was taken to a specialist children’s hospital, where she was cared for an additional two weeks. “During the pregnancy I was very worried,” Sophorn says. “I felt so happy when I finally delivered my child.” Her daughter was born without any complications is now a happy and healthy four years old. In initial stages of her third pregnancy, Sophorn’s friends told her that she would have to undergo surgery on her cervix or have injections to help her carry her baby to term, and doctors at a private clinic confirmed their suggestions. However, she decided to seek a second opinion at RHAC, where doctors instead gave her a prescription to strengthen her cervix. “When I heard I needed to have that surgery I was very scared, so I was relieved when the doctor at RHAC told me to take the medication instead,” she says. “While I was taking the medication I observed my body and any changes to it, so when I felt unwell I would go to the doctors and consult them, so I felt comfortable to continue taking it.” Sophorn also went for appointments at a government-run hospital, but found that their services were also lacking. “I told the doctors about losing my first and second babies, but they only weighed me and measured my stomach. There weren’t any more examinations or very much care,” she says. “When I went to RHAC they did so many examinations and had so many services, so I think it’s really better to go to RHAC for these kinds of services.” She estimates that during her third pregnancy, she had ten appointments at RHAC clinics at a cost of 40,000 to 60,000 riel (£7.40 to £11.15) each time. Compared to just 2,000 riel for an obstetrics appointment at the public hospital, the difference in cost is significant. “It’s expensive for me because my salary is little.” Despite the relatively high prices, Sophorn already knows where she will go for medical care in the future. “I want to have one more child, and I have already planned that when I decide to do it I will go to RHAC to get my cervix checked first,” she says. Until that day comes, Sophorn is taking the oral contraceptive after receiving advice about birth control from RHAC’s clinicians, with a midwife from the NGO making regular visits to the factory.

| 16 November 2017
“Just yesterday during the outreach service, a woman asked me why she didn’t get her period after having an abortion..."
Pann Chandy gave her first sexual education lesson when she was still at school as a volunteer youth social worker with the Reproductive Health Association of Cambodia (RHAC). She had no qualms about standing up in front of her classmates to discuss culturally taboo topics when she was just a teenager. Now aged 25 and in possession of a Bachelor degree in midwifery, Chandy has been employed by RHAC for less than a year, working as part of the organisation’s health outreach team. The job is demanding: she is tasked with regularly visiting four karaoke parlours, eight garment factories and 20 villages in Phnom Penh, with plans to expand to two universities imminently. Travelling for hours A round trip to some communities can take two hours or more on her motorcycle, travelling alone into areas that are not always easily accessible. “Sometimes I have the clinic staff with me, but rarely,” Chandy says. “I promote the health services provided by Reproductive Health Association of Cambodia as well. If they are interested in going to a clinic, I give them a referral,” she says. One of the factories on her regular roster is Propitious garment factory in Takhmao, a small city south of Phnom Penh. Chandy spends two days a month at the factory, where she speaks to groups of women or has one-on-one discussions about sensitive topics. Passionate about the job “Just yesterday during the outreach service, a woman asked me why she didn’t get her period after having an abortion. She wanted to know what was wrong,” she says. “It’s common for women to use unsafe abortion methods. Mainly they take medicine from a pharmacy, and the pharmacy doesn’t give them any advice on how to use it. Often they go to cheap, unlicensed clinics near the factories for medical abortions.” Chandy is passionate about her job at Reproductive Health Association of Cambodia, and dreams about one day setting up her own pharmacy where she could provide comprehensive advice to clients. “There are a lot of unlicensed pharmacists in this country,” she says, many of which prescribe the counterfeit medicines that have inundated the market. “I think I may have the capacity to become a licensed one."

| 19 April 2024
“Just yesterday during the outreach service, a woman asked me why she didn’t get her period after having an abortion..."
Pann Chandy gave her first sexual education lesson when she was still at school as a volunteer youth social worker with the Reproductive Health Association of Cambodia (RHAC). She had no qualms about standing up in front of her classmates to discuss culturally taboo topics when she was just a teenager. Now aged 25 and in possession of a Bachelor degree in midwifery, Chandy has been employed by RHAC for less than a year, working as part of the organisation’s health outreach team. The job is demanding: she is tasked with regularly visiting four karaoke parlours, eight garment factories and 20 villages in Phnom Penh, with plans to expand to two universities imminently. Travelling for hours A round trip to some communities can take two hours or more on her motorcycle, travelling alone into areas that are not always easily accessible. “Sometimes I have the clinic staff with me, but rarely,” Chandy says. “I promote the health services provided by Reproductive Health Association of Cambodia as well. If they are interested in going to a clinic, I give them a referral,” she says. One of the factories on her regular roster is Propitious garment factory in Takhmao, a small city south of Phnom Penh. Chandy spends two days a month at the factory, where she speaks to groups of women or has one-on-one discussions about sensitive topics. Passionate about the job “Just yesterday during the outreach service, a woman asked me why she didn’t get her period after having an abortion. She wanted to know what was wrong,” she says. “It’s common for women to use unsafe abortion methods. Mainly they take medicine from a pharmacy, and the pharmacy doesn’t give them any advice on how to use it. Often they go to cheap, unlicensed clinics near the factories for medical abortions.” Chandy is passionate about her job at Reproductive Health Association of Cambodia, and dreams about one day setting up her own pharmacy where she could provide comprehensive advice to clients. “There are a lot of unlicensed pharmacists in this country,” she says, many of which prescribe the counterfeit medicines that have inundated the market. “I think I may have the capacity to become a licensed one."

| 22 January 2018
"We are non-judgemental; we embark on a mutual learning process."
It used to take Matilda Meke-Banda six hours on her motorbike along dirt roads to reach two remote districts and deliver sexual and reproductive health (SRH) services. In this part of southern Malawi, Machinga, family planning uptake is low, and the fertility rate, at 6.6, is the highest in the country. The Family Planning Association of Malawi, known as FPAM, runs a clinic in the town of Liwonde and it’s from here that Matilda travelled out six times a month. “We have established six watch groups, they are trained to address SRH issues in the community,” she explains. Luc Simon is the chair of one of those groups. “We teach about Family Planning,” he says. “We encourage parents and young people to go for HIV testing. We address forced early marriages, talk to parents and children to save a lot of young people.” And there are a lot of myths to dispel about family planning. Elizabeth Katunga is head of family planning in the district hospital in Machinga: “Family Planning is not very much accepted by the communities. Many women hide the use of contraceptives,” she says. “Injectables are most popular, easy to hide. We have cases here where husbands upon discovery of an implant take a knife and cut it out. It is not that people want big families per se but it is the misconceptions about contraceptives.” FPAM’s projects are based at the Youth Life clinic in Liwonde. The clinic offers integrated services: Family planning, HIV services, STI screening, cervical cancer screening and general healthcare (such as malaria). This joined-up approach has been effective says FPAM’s executive director Thoko Mbendera: “In government health facilities, you have different days, and long queues always, for family planning, for HIV, for general health, which is a challenge if the clinic is a 20 km walk away.There are privacy issues.” But now, FPAM’s services are being cut because of the Global Gag Rule (GGR), mobile clinics are grounded, and there are fears that much progress will be undone. Some of FPAM’s rural clients explain how the Watch Groups work in their community. “It starts with me as a man,” says group member George Mpemba. “We are examples on how to live with our wives. We are non-judgemental; we embark on a mutual learning process. Our meetings are not hearings, but a normal chat, there is laughing and talking. After the discussion we evaluate together and make an action plan.” Katherine, went to the group for help: “There was violence in my marriage; my husband forced himself on me even if I was tired from working in the field. When I complained there was trouble. He did not provide even the bedding. “He is a fisherman and he makes a lot of cash which he used to buy beer but nothing for us.I overheard a watch group meeting once and I realised there was a solution. They talked to him and made him realise that what he was doing was violence and against the law. It was ignorance.Things are better now, he brings money home, sex is consensual and sometimes he helps with household chores.”

| 19 April 2024
"We are non-judgemental; we embark on a mutual learning process."
It used to take Matilda Meke-Banda six hours on her motorbike along dirt roads to reach two remote districts and deliver sexual and reproductive health (SRH) services. In this part of southern Malawi, Machinga, family planning uptake is low, and the fertility rate, at 6.6, is the highest in the country. The Family Planning Association of Malawi, known as FPAM, runs a clinic in the town of Liwonde and it’s from here that Matilda travelled out six times a month. “We have established six watch groups, they are trained to address SRH issues in the community,” she explains. Luc Simon is the chair of one of those groups. “We teach about Family Planning,” he says. “We encourage parents and young people to go for HIV testing. We address forced early marriages, talk to parents and children to save a lot of young people.” And there are a lot of myths to dispel about family planning. Elizabeth Katunga is head of family planning in the district hospital in Machinga: “Family Planning is not very much accepted by the communities. Many women hide the use of contraceptives,” she says. “Injectables are most popular, easy to hide. We have cases here where husbands upon discovery of an implant take a knife and cut it out. It is not that people want big families per se but it is the misconceptions about contraceptives.” FPAM’s projects are based at the Youth Life clinic in Liwonde. The clinic offers integrated services: Family planning, HIV services, STI screening, cervical cancer screening and general healthcare (such as malaria). This joined-up approach has been effective says FPAM’s executive director Thoko Mbendera: “In government health facilities, you have different days, and long queues always, for family planning, for HIV, for general health, which is a challenge if the clinic is a 20 km walk away.There are privacy issues.” But now, FPAM’s services are being cut because of the Global Gag Rule (GGR), mobile clinics are grounded, and there are fears that much progress will be undone. Some of FPAM’s rural clients explain how the Watch Groups work in their community. “It starts with me as a man,” says group member George Mpemba. “We are examples on how to live with our wives. We are non-judgemental; we embark on a mutual learning process. Our meetings are not hearings, but a normal chat, there is laughing and talking. After the discussion we evaluate together and make an action plan.” Katherine, went to the group for help: “There was violence in my marriage; my husband forced himself on me even if I was tired from working in the field. When I complained there was trouble. He did not provide even the bedding. “He is a fisherman and he makes a lot of cash which he used to buy beer but nothing for us.I overheard a watch group meeting once and I realised there was a solution. They talked to him and made him realise that what he was doing was violence and against the law. It was ignorance.Things are better now, he brings money home, sex is consensual and sometimes he helps with household chores.”
| 19 January 2018
“I am afraid what will happen when there will be no more projects like this one"
On Friday afternoon in Municipal Lycee of Nyakabiga, Burundi, headmistress Chantal Keza is introducing her students to the medical staff from Association Burundaise pour le Bien-Etre Familial (ABUBEF). Peer educators at the school, trained by ABUBEF, will perform a short drama based around sexual health and will answer questions about contraception methods from students. One of the actresses is peer educator Ammande Berlyne Dushime. Ammande, who is 17 years old is one of three peer educators at the school. Ammande, together with her friends, perform their short drama on the stage based on a young girls quest for information on contraception. It ends on a positive note, with the girl receiving useful and correct information from a peer educator at her school. A story that could be a very real life scenario at her school. Peer programmes that trained Ammande, are under threat of closure due to the Global Gag rule. Ammande says, “I am afraid what will happen when there will be no more projects like this one. I am ready to go on with work as peer educator, but if there are not going to be regular visits by the medical stuff from the clinic, then we will have no one to seek information and advice from. I am just a teenager, I know so little. Not only I will lose my support, but also I will not be taken serious by my schoolmates. With such important topic like sexual education and contraception, I am not the authority. I can only show the right way to go. And this road leads to ABUBEF.” She says “As peer educator I am responsible for Saturday morning meetings at the clinic. We sing songs, play games, have fun and learn new things about sex education, contraception, HIV protection and others. Visiting the clinic is then very easy, and no student has to be afraid, that showing up at the clinic that treats HIV positive people, will ruin their reputation. Now they know that we can meet there openly, and undercover of these meetings seek for help, information, professional advice and contraception methods” Peer educator classes are a safe and open place for students to openly talk about their sexual health. The Global Gage Rule will force peer educator programmes like this to close due to lack of funding. Help us bridge the funding gap Learn more about the Global Gag Rule
| 19 April 2024
“I am afraid what will happen when there will be no more projects like this one"
On Friday afternoon in Municipal Lycee of Nyakabiga, Burundi, headmistress Chantal Keza is introducing her students to the medical staff from Association Burundaise pour le Bien-Etre Familial (ABUBEF). Peer educators at the school, trained by ABUBEF, will perform a short drama based around sexual health and will answer questions about contraception methods from students. One of the actresses is peer educator Ammande Berlyne Dushime. Ammande, who is 17 years old is one of three peer educators at the school. Ammande, together with her friends, perform their short drama on the stage based on a young girls quest for information on contraception. It ends on a positive note, with the girl receiving useful and correct information from a peer educator at her school. A story that could be a very real life scenario at her school. Peer programmes that trained Ammande, are under threat of closure due to the Global Gag rule. Ammande says, “I am afraid what will happen when there will be no more projects like this one. I am ready to go on with work as peer educator, but if there are not going to be regular visits by the medical stuff from the clinic, then we will have no one to seek information and advice from. I am just a teenager, I know so little. Not only I will lose my support, but also I will not be taken serious by my schoolmates. With such important topic like sexual education and contraception, I am not the authority. I can only show the right way to go. And this road leads to ABUBEF.” She says “As peer educator I am responsible for Saturday morning meetings at the clinic. We sing songs, play games, have fun and learn new things about sex education, contraception, HIV protection and others. Visiting the clinic is then very easy, and no student has to be afraid, that showing up at the clinic that treats HIV positive people, will ruin their reputation. Now they know that we can meet there openly, and undercover of these meetings seek for help, information, professional advice and contraception methods” Peer educator classes are a safe and open place for students to openly talk about their sexual health. The Global Gage Rule will force peer educator programmes like this to close due to lack of funding. Help us bridge the funding gap Learn more about the Global Gag Rule

| 17 November 2017
“The doctors have also been giving me advice on how to look after myself and the baby"
When garment worker Ny thought she might be pregnant with her first child, a home test kit quickly confirmed her suspicions. But the 23-year-old – who is originally from Takeo province but moved to Phnom Penh to take up a job in the garment industry – did not know where to go to seek prenatal care. After a cousin recommended that she visit a nearby Reproductive Health Association of Cambodia clinic, Ny took her relative’s advice – and has gone back eight times to date. “I come here every month to check on the baby,” she says, cradling her belly. “I had never been before I got pregnant.” During her visits to the medical clinic, Ny says, she has had a raft of standard tests and procedures as part of her prenatal care, including two ultrasounds, blood and urine tests, and vaccinations. “The doctors have also been giving me advice on how to look after myself and the baby [such as] to eat nutritious food and not to carry heavy things,” she says. As well as caring for the health of mother and unborn child, RHAC staff have also offered up valuable family planning information. “I did not know about how to plan to have children before I came to the clinic,” Ny says. “The doctors here told me that there are three different methods of [long-term] contraception: medication, an implant and an IUD.” Ny, who sews winter clothing at a factory while her husband also works in a nearby garment factory, says she was very glad to learn about her options. “This child was unplanned, but I don’t feel any regret because I had already been married for two years. But after having the baby I plan to use birth control, though I don’t know what method I will use,” she says. “I know that I don’t want to have another child straight away. It may be two or three years until I have the next one, as I want to wait until my family’s finances improve.”

| 19 April 2024
“The doctors have also been giving me advice on how to look after myself and the baby"
When garment worker Ny thought she might be pregnant with her first child, a home test kit quickly confirmed her suspicions. But the 23-year-old – who is originally from Takeo province but moved to Phnom Penh to take up a job in the garment industry – did not know where to go to seek prenatal care. After a cousin recommended that she visit a nearby Reproductive Health Association of Cambodia clinic, Ny took her relative’s advice – and has gone back eight times to date. “I come here every month to check on the baby,” she says, cradling her belly. “I had never been before I got pregnant.” During her visits to the medical clinic, Ny says, she has had a raft of standard tests and procedures as part of her prenatal care, including two ultrasounds, blood and urine tests, and vaccinations. “The doctors have also been giving me advice on how to look after myself and the baby [such as] to eat nutritious food and not to carry heavy things,” she says. As well as caring for the health of mother and unborn child, RHAC staff have also offered up valuable family planning information. “I did not know about how to plan to have children before I came to the clinic,” Ny says. “The doctors here told me that there are three different methods of [long-term] contraception: medication, an implant and an IUD.” Ny, who sews winter clothing at a factory while her husband also works in a nearby garment factory, says she was very glad to learn about her options. “This child was unplanned, but I don’t feel any regret because I had already been married for two years. But after having the baby I plan to use birth control, though I don’t know what method I will use,” she says. “I know that I don’t want to have another child straight away. It may be two or three years until I have the next one, as I want to wait until my family’s finances improve.”

| 16 November 2017
“When they don’t dare to ask questions about sensitive health topics, they don’t have the information they need"
Female workers, many of them undereducated migrants from rural areas, dominate the garment sector in Cambodia. And Propitious garment factory in Takhmao, a small city that lies just south of the capital Phnom Penh, is no exception. Women make up more than 90 percent of the factory’s workforce. Helping to oversee the 3,700-strong workforce is human resources manager Kouch Davy, who has worked at Propitious since it opened four years ago. Seeing a need to improve the workers’ sexual and reproductive health knowledge, she says she decided to work with the Reproductive Health Association of Cambodia (RHAC) because of its reputation for providing high-quality services. “I raised it in a management meeting, and the board was happy to explore it,” she says. For almost two years, trained staff from RHAC have been visiting the factory twice a month to meet with workers during their lunch break. They answer questions on topics ranging from birth control to STIs and abortion. The organisation has also provided training to the nurses who work in the factory’s on-site medical clinic. Davy says the factory’s female garment workers have changed as a result. “They are more open to asking questions about sexual health and they have also become more informed about the subject,” she says. “When they don’t dare to ask questions about sensitive health topics, they don’t have the information they need, so they tend to exaggerate their problems and ask for sick leave. But when they go to see an RHAC clinic and get proper treatment, there is less sick leave. “Now that they understand about contraception, there are fewer women getting pregnant and taking maternity leave, so that also helps with the workflow. ” Davy says the factory has seen requests for sick leave drop by an average of between 100 to 200 cases a month – and any decrease in absenteeism is a major boon for productivity. “The factory works like a chain: if just one person on the production line takes a day off, it affects the overall productivity,” she says. “And if a worker comes to work sick, they have problems concentrating.” Even Davy says she has gone to RHAC to seek medical care, visiting one of their clinics a few months ago for a breast examination. Meanwhile, the company that owns Propitious has extended its partnership with RHAC to a second factory in Phnom Penh. The firm has even requested that the NGO starts visiting its largest factory, which is situated in a rural province and has 10,000 workers, in the future.

| 19 April 2024
“When they don’t dare to ask questions about sensitive health topics, they don’t have the information they need"
Female workers, many of them undereducated migrants from rural areas, dominate the garment sector in Cambodia. And Propitious garment factory in Takhmao, a small city that lies just south of the capital Phnom Penh, is no exception. Women make up more than 90 percent of the factory’s workforce. Helping to oversee the 3,700-strong workforce is human resources manager Kouch Davy, who has worked at Propitious since it opened four years ago. Seeing a need to improve the workers’ sexual and reproductive health knowledge, she says she decided to work with the Reproductive Health Association of Cambodia (RHAC) because of its reputation for providing high-quality services. “I raised it in a management meeting, and the board was happy to explore it,” she says. For almost two years, trained staff from RHAC have been visiting the factory twice a month to meet with workers during their lunch break. They answer questions on topics ranging from birth control to STIs and abortion. The organisation has also provided training to the nurses who work in the factory’s on-site medical clinic. Davy says the factory’s female garment workers have changed as a result. “They are more open to asking questions about sexual health and they have also become more informed about the subject,” she says. “When they don’t dare to ask questions about sensitive health topics, they don’t have the information they need, so they tend to exaggerate their problems and ask for sick leave. But when they go to see an RHAC clinic and get proper treatment, there is less sick leave. “Now that they understand about contraception, there are fewer women getting pregnant and taking maternity leave, so that also helps with the workflow. ” Davy says the factory has seen requests for sick leave drop by an average of between 100 to 200 cases a month – and any decrease in absenteeism is a major boon for productivity. “The factory works like a chain: if just one person on the production line takes a day off, it affects the overall productivity,” she says. “And if a worker comes to work sick, they have problems concentrating.” Even Davy says she has gone to RHAC to seek medical care, visiting one of their clinics a few months ago for a breast examination. Meanwhile, the company that owns Propitious has extended its partnership with RHAC to a second factory in Phnom Penh. The firm has even requested that the NGO starts visiting its largest factory, which is situated in a rural province and has 10,000 workers, in the future.

| 16 November 2017
"During the pregnancy I was very worried”
Sophorn, a garment worker for the past decade, first visited a Reproductive Health Association of Cambodia (RHAC) clinic when she was pregnant with her first child. She returned for health checks each month until, at five months pregnant, she lost the baby. Her second pregnancy also resulted in a miscarriage, leaving her distraught. Then, she got pregnant a third time, in 2013. “I started to discuss with the doctors how to protect my child,” she says. “They gave me medication to strengthen my cervix, which I took for six months. In the seventh month, I gave birth prematurely.” Doctors told Sophorn that her baby girl was health, but she only weighed in at 1.7 kilograms. The infant was taken to a specialist children’s hospital, where she was cared for an additional two weeks. “During the pregnancy I was very worried,” Sophorn says. “I felt so happy when I finally delivered my child.” Her daughter was born without any complications is now a happy and healthy four years old. In initial stages of her third pregnancy, Sophorn’s friends told her that she would have to undergo surgery on her cervix or have injections to help her carry her baby to term, and doctors at a private clinic confirmed their suggestions. However, she decided to seek a second opinion at RHAC, where doctors instead gave her a prescription to strengthen her cervix. “When I heard I needed to have that surgery I was very scared, so I was relieved when the doctor at RHAC told me to take the medication instead,” she says. “While I was taking the medication I observed my body and any changes to it, so when I felt unwell I would go to the doctors and consult them, so I felt comfortable to continue taking it.” Sophorn also went for appointments at a government-run hospital, but found that their services were also lacking. “I told the doctors about losing my first and second babies, but they only weighed me and measured my stomach. There weren’t any more examinations or very much care,” she says. “When I went to RHAC they did so many examinations and had so many services, so I think it’s really better to go to RHAC for these kinds of services.” She estimates that during her third pregnancy, she had ten appointments at RHAC clinics at a cost of 40,000 to 60,000 riel (£7.40 to £11.15) each time. Compared to just 2,000 riel for an obstetrics appointment at the public hospital, the difference in cost is significant. “It’s expensive for me because my salary is little.” Despite the relatively high prices, Sophorn already knows where she will go for medical care in the future. “I want to have one more child, and I have already planned that when I decide to do it I will go to RHAC to get my cervix checked first,” she says. Until that day comes, Sophorn is taking the oral contraceptive after receiving advice about birth control from RHAC’s clinicians, with a midwife from the NGO making regular visits to the factory.

| 19 April 2024
"During the pregnancy I was very worried”
Sophorn, a garment worker for the past decade, first visited a Reproductive Health Association of Cambodia (RHAC) clinic when she was pregnant with her first child. She returned for health checks each month until, at five months pregnant, she lost the baby. Her second pregnancy also resulted in a miscarriage, leaving her distraught. Then, she got pregnant a third time, in 2013. “I started to discuss with the doctors how to protect my child,” she says. “They gave me medication to strengthen my cervix, which I took for six months. In the seventh month, I gave birth prematurely.” Doctors told Sophorn that her baby girl was health, but she only weighed in at 1.7 kilograms. The infant was taken to a specialist children’s hospital, where she was cared for an additional two weeks. “During the pregnancy I was very worried,” Sophorn says. “I felt so happy when I finally delivered my child.” Her daughter was born without any complications is now a happy and healthy four years old. In initial stages of her third pregnancy, Sophorn’s friends told her that she would have to undergo surgery on her cervix or have injections to help her carry her baby to term, and doctors at a private clinic confirmed their suggestions. However, she decided to seek a second opinion at RHAC, where doctors instead gave her a prescription to strengthen her cervix. “When I heard I needed to have that surgery I was very scared, so I was relieved when the doctor at RHAC told me to take the medication instead,” she says. “While I was taking the medication I observed my body and any changes to it, so when I felt unwell I would go to the doctors and consult them, so I felt comfortable to continue taking it.” Sophorn also went for appointments at a government-run hospital, but found that their services were also lacking. “I told the doctors about losing my first and second babies, but they only weighed me and measured my stomach. There weren’t any more examinations or very much care,” she says. “When I went to RHAC they did so many examinations and had so many services, so I think it’s really better to go to RHAC for these kinds of services.” She estimates that during her third pregnancy, she had ten appointments at RHAC clinics at a cost of 40,000 to 60,000 riel (£7.40 to £11.15) each time. Compared to just 2,000 riel for an obstetrics appointment at the public hospital, the difference in cost is significant. “It’s expensive for me because my salary is little.” Despite the relatively high prices, Sophorn already knows where she will go for medical care in the future. “I want to have one more child, and I have already planned that when I decide to do it I will go to RHAC to get my cervix checked first,” she says. Until that day comes, Sophorn is taking the oral contraceptive after receiving advice about birth control from RHAC’s clinicians, with a midwife from the NGO making regular visits to the factory.

| 16 November 2017
“Just yesterday during the outreach service, a woman asked me why she didn’t get her period after having an abortion..."
Pann Chandy gave her first sexual education lesson when she was still at school as a volunteer youth social worker with the Reproductive Health Association of Cambodia (RHAC). She had no qualms about standing up in front of her classmates to discuss culturally taboo topics when she was just a teenager. Now aged 25 and in possession of a Bachelor degree in midwifery, Chandy has been employed by RHAC for less than a year, working as part of the organisation’s health outreach team. The job is demanding: she is tasked with regularly visiting four karaoke parlours, eight garment factories and 20 villages in Phnom Penh, with plans to expand to two universities imminently. Travelling for hours A round trip to some communities can take two hours or more on her motorcycle, travelling alone into areas that are not always easily accessible. “Sometimes I have the clinic staff with me, but rarely,” Chandy says. “I promote the health services provided by Reproductive Health Association of Cambodia as well. If they are interested in going to a clinic, I give them a referral,” she says. One of the factories on her regular roster is Propitious garment factory in Takhmao, a small city south of Phnom Penh. Chandy spends two days a month at the factory, where she speaks to groups of women or has one-on-one discussions about sensitive topics. Passionate about the job “Just yesterday during the outreach service, a woman asked me why she didn’t get her period after having an abortion. She wanted to know what was wrong,” she says. “It’s common for women to use unsafe abortion methods. Mainly they take medicine from a pharmacy, and the pharmacy doesn’t give them any advice on how to use it. Often they go to cheap, unlicensed clinics near the factories for medical abortions.” Chandy is passionate about her job at Reproductive Health Association of Cambodia, and dreams about one day setting up her own pharmacy where she could provide comprehensive advice to clients. “There are a lot of unlicensed pharmacists in this country,” she says, many of which prescribe the counterfeit medicines that have inundated the market. “I think I may have the capacity to become a licensed one."

| 19 April 2024
“Just yesterday during the outreach service, a woman asked me why she didn’t get her period after having an abortion..."
Pann Chandy gave her first sexual education lesson when she was still at school as a volunteer youth social worker with the Reproductive Health Association of Cambodia (RHAC). She had no qualms about standing up in front of her classmates to discuss culturally taboo topics when she was just a teenager. Now aged 25 and in possession of a Bachelor degree in midwifery, Chandy has been employed by RHAC for less than a year, working as part of the organisation’s health outreach team. The job is demanding: she is tasked with regularly visiting four karaoke parlours, eight garment factories and 20 villages in Phnom Penh, with plans to expand to two universities imminently. Travelling for hours A round trip to some communities can take two hours or more on her motorcycle, travelling alone into areas that are not always easily accessible. “Sometimes I have the clinic staff with me, but rarely,” Chandy says. “I promote the health services provided by Reproductive Health Association of Cambodia as well. If they are interested in going to a clinic, I give them a referral,” she says. One of the factories on her regular roster is Propitious garment factory in Takhmao, a small city south of Phnom Penh. Chandy spends two days a month at the factory, where she speaks to groups of women or has one-on-one discussions about sensitive topics. Passionate about the job “Just yesterday during the outreach service, a woman asked me why she didn’t get her period after having an abortion. She wanted to know what was wrong,” she says. “It’s common for women to use unsafe abortion methods. Mainly they take medicine from a pharmacy, and the pharmacy doesn’t give them any advice on how to use it. Often they go to cheap, unlicensed clinics near the factories for medical abortions.” Chandy is passionate about her job at Reproductive Health Association of Cambodia, and dreams about one day setting up her own pharmacy where she could provide comprehensive advice to clients. “There are a lot of unlicensed pharmacists in this country,” she says, many of which prescribe the counterfeit medicines that have inundated the market. “I think I may have the capacity to become a licensed one."