Spotlight
A selection of stories from across the Federation

France, Germany, Poland, United Kingdom, United States, Colombia, India, Tunisia
Abortion Rights: Latest Decisions and Developments around the World
The global landscape of abortion rights continues to evolve in 2024, with new legislation and feminist movements fighting for better access. Let's take a trip around the world to see the latest developments.
Most Popular This Week
France, Germany, Poland, United Kingdom, United States, Colombia, India, Tunisia

Abortion Rights: Latest Decisions and Developments around the World
Over the past 30 years, more than

Palestine

In their own words: The people providing sexual and reproductive health care under bombardment in Gaza
Week after week, heavy Israeli bombardment from air, land, and sea, has continued across most of the Gaza Strip.
Vanuatu

When getting to the hospital is difficult, Vanuatu mobile outreach can save lives
In the mountains of Kumera on Tanna Island, Vanuatu, the village women of Kamahaul normally spend over 10,000 Vatu ($83 USD) to travel to the nearest hospital.
Vanuatu

Sex: changing minds and winning hearts in Tanna, Vanuatu
“Very traditional.” These two words are often used to describe the people of Tanna in Vanuatu, one of the most populated islands in the small country in the Pacific.
Vanuatu

Vanuatu cyclone response: The mental health toll on humanitarian providers
Girls and women from nearby villages flock to mobile health clinics set up by the Vanuatu Family Health Association (VFHA).
Cook Islands

Trans & Proud: Being Transgender in the Cook Islands
It’s a scene like many others around the world: a loving family pour over childhood photos, giggling and reminiscing about the memories.
Cook Islands

In Pictures: The activists who helped win LGBTI+ rights in the Cook Islands
The Cook Islands has removed a law that criminalizes homosexuality, in a huge victory for the local LGBTI+ community.
Filter our stories by:
- Albanian Center for Population and Development
- Associação Moçambicana para Desenvolvimento da Família
- Association Burundaise pour le Bien-Etre Familial
- Association Malienne pour la Protection et la Promotion de la Famille
- Association Togolaise pour le Bien-Etre Familial
- Botswana Family Welfare Association
- Cameroon National Association for Family Welfare
- Family Guidance Association of Ethiopia
- Family Planning Association of Malawi
- Family Planning Association of Nepal
- Family Planning Association of Sri Lanka
- Family Planning Association of Trinidad and Tobago
- Foundation for the Promotion of Responsible Parenthood - Aruba
- Indonesian Planned Parenthood Association
- Jamaica Family Planning Association
- Kiribati Family Health Association
- Lesotho Planned Parenthood Association
- Palestinian Family Planning and Protection Association (PFPPA)
- Planned Parenthood Association of Ghana
- Planned Parenthood Association of Thailand
- Planned Parenthood Association of Zambia
- Planned Parenthood Federation of America
- Planned Parenthood Federation of Nigeria
- Reproductive & Family Health Association of Fiji
- Reproductive Health Uganda
- Somaliland Family Health Association
- Vanuatu Family Health Association


| 17 August 2021
In pictures: World Humanitarian Day 2021
This World Humanitarian Day we reflect on the incredible work undertaken by our humanitarian response teams over the last 12 months. Last year, IPPF reached approximately 5.5 million people in humanitarian crises through our local Member Associations. This achievement would not have been possible without the dedicated and heroic healthcare teams providing vital sexual and reproductive healthcare in the most fragile humanitarian settings. COVID-19 response in Papua New Guinea Papua New Guinea Family Health Association (PNGFHA) PNGFHA responded to the COVID-19 outbreak in PNG, supported by the Australian government. With access to emergency healthcare facilities now extremely limited, PNGFHA health workers travel to hard-to-reach areas providing sexual and reproductive healthcare to the most marginalized communities.Clients like Vavine Kila receive a consultation at the PNGFHA mobile clinic. Share on Twitter Share on Facebook Share via WhatsApp Share via Email The humanitarian response teams taking healthcare into people's homes in Gaza Palestinian Family Planning and Protection Association (PFPPA) On 10 May 2021, Israel launched airstrikes on the Gaza Strip, killing over 220 people (including women and children) and leaving over 75,000 displaced. At the time, an estimated 87,000 women in the Gaza Strip and nearby areas were pregnant. The PFPPA humanitarian response team visited families in their homes, with each household expected to have four to five women of reproductive age needing healthcare. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Offering holistic care to families in Gaza Palestinian Family Planning and Protection Association (PFPPA) Children account for close to 50% of the population in Gaza. As part of the response, PFPPA youth volunteers entertained the children while their family members received life-saving sexual and reproductive healthcare and psychosocial support by the humanitarian response teams in privacy. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Ensuring ante- and post-natal care in the aftermath of an earthquake in West Sulawesi Indonesia Planned Parenthood Association (IPPA) On 15 January 2021, a 6.2 magnitude earthquake struck the West Sulawesi province in Indonesia leaving over 15,000 displaced, including many pregnant people and nursing mothers.As part of its response efforts, the IPPA set up mobile clinics near the shelters to provide vital ante- and post-natal care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email A super cyclone and a pandemic Family Planning Association of India (FPAI) On 20 May 2020, severe Cyclone Amphan hit the Indian state of West Bengal, affecting millions of people in and around the state capital Kolkata. Emergency crises during the COVID-19 pandemic intensifies the impact of the disaster and puts a strain on health systems and access to sexual and reproductive healthcare.FPAI responded by providing emergency sexual and reproductive healthcare to affected communities, particularly focusing on the most marginalized and vulnerable people including the LGBTI community, sex workers, pregnant women, and survivors of sexual and gender-based violence (SGBV). Share on Twitter Share on Facebook Share via WhatsApp Share via Email Providing healthcare to hardest hit communities after Cyclone Yasa The Reproductive and Family Health Association of Fiji (RFHAF) In mid-December 2020, a category 5 severe Tropical Cyclone Yasa hit the island of Fiji and neighbouring Lau group of Islands. IPPF’s Member Association, RFHAF, was supported by the Australian government to provide life-saving sexual and reproductive healthcare in the hardest hit communities, including counselling on STI risk reduction, first-line support for survivors of SGBV, and contraceptive and ante-natal care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 24 April 2024
In pictures: World Humanitarian Day 2021
This World Humanitarian Day we reflect on the incredible work undertaken by our humanitarian response teams over the last 12 months. Last year, IPPF reached approximately 5.5 million people in humanitarian crises through our local Member Associations. This achievement would not have been possible without the dedicated and heroic healthcare teams providing vital sexual and reproductive healthcare in the most fragile humanitarian settings. COVID-19 response in Papua New Guinea Papua New Guinea Family Health Association (PNGFHA) PNGFHA responded to the COVID-19 outbreak in PNG, supported by the Australian government. With access to emergency healthcare facilities now extremely limited, PNGFHA health workers travel to hard-to-reach areas providing sexual and reproductive healthcare to the most marginalized communities.Clients like Vavine Kila receive a consultation at the PNGFHA mobile clinic. Share on Twitter Share on Facebook Share via WhatsApp Share via Email The humanitarian response teams taking healthcare into people's homes in Gaza Palestinian Family Planning and Protection Association (PFPPA) On 10 May 2021, Israel launched airstrikes on the Gaza Strip, killing over 220 people (including women and children) and leaving over 75,000 displaced. At the time, an estimated 87,000 women in the Gaza Strip and nearby areas were pregnant. The PFPPA humanitarian response team visited families in their homes, with each household expected to have four to five women of reproductive age needing healthcare. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Offering holistic care to families in Gaza Palestinian Family Planning and Protection Association (PFPPA) Children account for close to 50% of the population in Gaza. As part of the response, PFPPA youth volunteers entertained the children while their family members received life-saving sexual and reproductive healthcare and psychosocial support by the humanitarian response teams in privacy. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Ensuring ante- and post-natal care in the aftermath of an earthquake in West Sulawesi Indonesia Planned Parenthood Association (IPPA) On 15 January 2021, a 6.2 magnitude earthquake struck the West Sulawesi province in Indonesia leaving over 15,000 displaced, including many pregnant people and nursing mothers.As part of its response efforts, the IPPA set up mobile clinics near the shelters to provide vital ante- and post-natal care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email A super cyclone and a pandemic Family Planning Association of India (FPAI) On 20 May 2020, severe Cyclone Amphan hit the Indian state of West Bengal, affecting millions of people in and around the state capital Kolkata. Emergency crises during the COVID-19 pandemic intensifies the impact of the disaster and puts a strain on health systems and access to sexual and reproductive healthcare.FPAI responded by providing emergency sexual and reproductive healthcare to affected communities, particularly focusing on the most marginalized and vulnerable people including the LGBTI community, sex workers, pregnant women, and survivors of sexual and gender-based violence (SGBV). Share on Twitter Share on Facebook Share via WhatsApp Share via Email Providing healthcare to hardest hit communities after Cyclone Yasa The Reproductive and Family Health Association of Fiji (RFHAF) In mid-December 2020, a category 5 severe Tropical Cyclone Yasa hit the island of Fiji and neighbouring Lau group of Islands. IPPF’s Member Association, RFHAF, was supported by the Australian government to provide life-saving sexual and reproductive healthcare in the hardest hit communities, including counselling on STI risk reduction, first-line support for survivors of SGBV, and contraceptive and ante-natal care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 10 August 2021
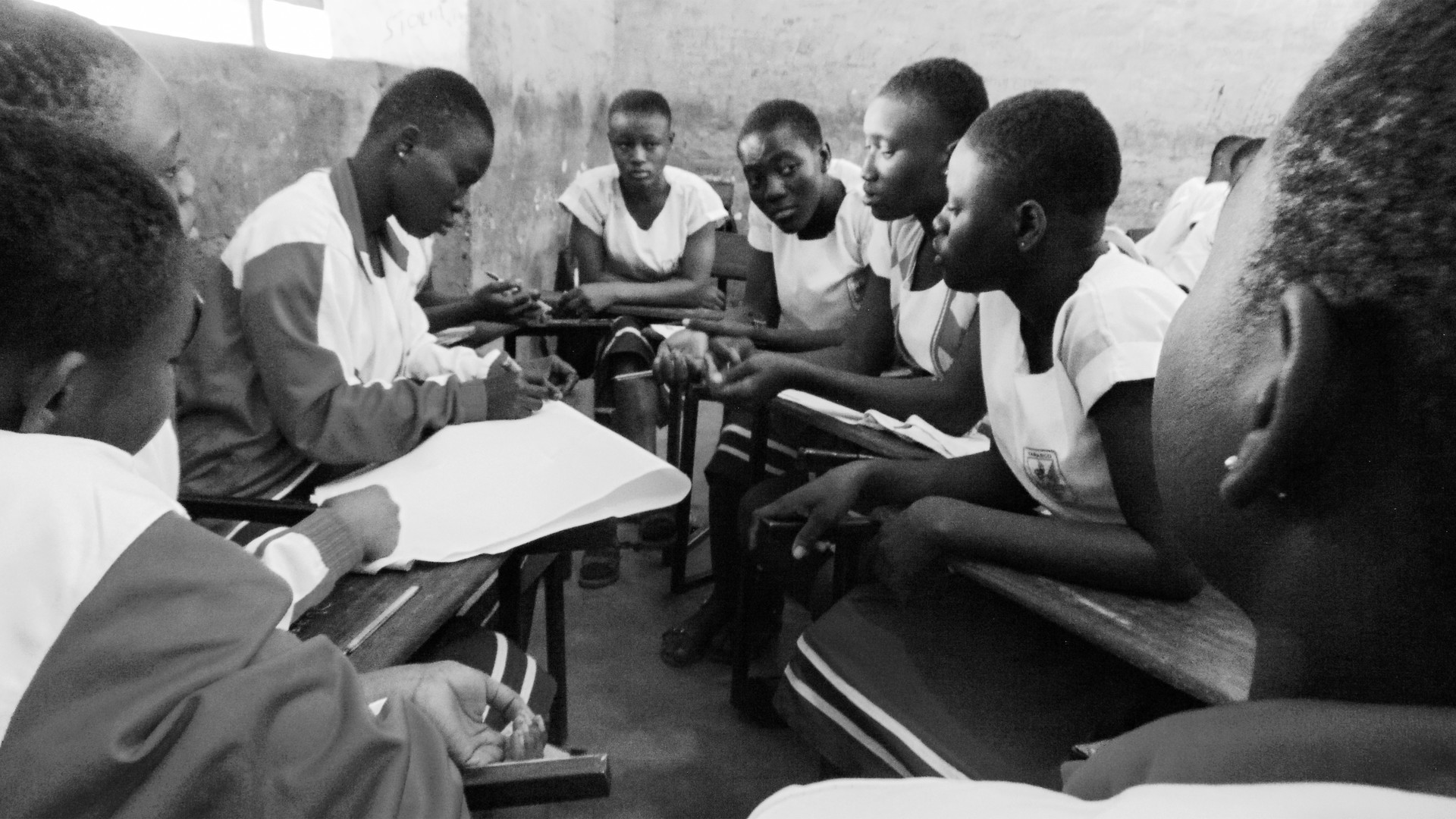
In Pictures: International Youth Day 2021
Last year, IPPF and our global Member Associations delivered a staggering 98.2 million sexual and reproductive health services to young people aged 25 and under – that’s approximately 45% of all services delivered. When young people are able to access and manage their sexual and reproductive health and rights (SRHR) with dignity and care, their chances of thriving in life increase, and as such we work with and for youth populations around the world in many ways. Take a look at some of the ways we have been involved with this and, more importantly, how young people themselves have been the driving force behind the fight for SRHR for all. Malawi Young volunteers connect their peers to information and contraceptive care Kondwani, a 22-year-old Youth Action Movement (YAM) volunteer, not only distributes condoms locally, she also challenges her peers to show her on a wooden model how to use them, because she knows that this can pose a problem for some people.Activities like this in hard-to-reach areas are one of many that the YAM delivers across Malawi. Trained and hosted by Youth Life Centres, which provide sexual and reproductive healthcare aimed at youth, volunteers like Kondwani meet up regularly and reach out to their peers in schools, universities, and on social media.Learn more about Kondwani Share on Twitter Share on Facebook Share via WhatsApp Share via Email Poland Defending human rights in the face of unrelenting attacks Nadia believes activism can change the world. Over the last few years in Poland, women’s reproductive choices have been stripped back at an alarming rate. The young activist wants to reverse this erosion of women’s rights by campaigning for better reproductive, labour and social rights across the country. Nadia is painfully aware that in Poland, where public discourse is dominated by men, the belief that “children and young women have no voice” still reigns.As a result of her activism, Nadia has become the target of visceral personal attacks online, unrelenting violent behaviour, sexism & discrimination – but she hasn't given up.Learn more about Nadia Share on Twitter Share on Facebook Share via WhatsApp Share via Email Mali Using street dance to teach about consent, contraception and more Abdoulaye Camara is the best dancer in the neighbourhood, and he’s not afraid to show it. But Abdoulaye’s moves aren't just for fun – he's head of the dance troupe of the Youth Action Movement, belonging to the Association Malienne pour la Protection et la Promotion de la Famille, which uses dance and comedy sketches to talk about sex.“We distract them with dance and humour and then we transmit those important messages about sex without offending them,” explains Abdoulaye. Sexuality, STIs, consent, early/unintended pregnancy, contraception, and more – no topic is off the table for Abdoulaye and his troupe. Learn more about Abdoulaye Share on Twitter Share on Facebook Share via WhatsApp Share via Email Aruba Providing information and contraceptive care to young people in school Access to information and contraceptives has always been a priority for Famia Planea Aruba (FPA) – whether through their office, a delivery service, or in schools. For over 15 years FPA has worked in partnership with one of the largest secondary schools on the island. The FPA team visits the school every month to provide guidance, counselling, and contraceptive care to students, and to help ensure they stay in school to complete their education.The FPA team works with students to build trust and ensure they feel safe to talk openly. This helps to provide a sense of consistency for the student and the team, who are better able to notice if something changes, and if a student needs a referral to a medical doctor or other organization for additional treatment.Learn more about FPA Share on Twitter Share on Facebook Share via WhatsApp Share via Email Indonesia Surviving an earthquake as a young mother during COVID-19 Shortly after becoming a mother at 18, Herlina’s home was struck by a powerful earthquake in January, forcing her and her baby Nur to flee. She had to deal with this terrifying situation alone, all during the COVID-19 pandemic as well.The Indonesia Planned Parenthood Association (IPPA) health volunteer team were able to support Herlina by providing sexual and reproductive healthcare services, specifically advising Herlina on postpartum care. The team also gave Herlina dignity kits, which included sanitary pads, underclothes, and soap to maintain proper hygiene, which is a common challenge in displaced communities.Learn more about Herlina Share on Twitter Share on Facebook Share via WhatsApp Share via Email Kiribati Abe the ‘Youth Warrior’ “It’s time to be talking about sexual and reproductive health and rights (SRHR) early on, let’s not wait until young people get in trouble.” Abe's voice reveals the energy and passion of someone who is doing what they were destined to do.He is a proud member of the LGBTI community, as well as of his local church – two worlds he tries to bring together in order to spread important healthcare messages among other young people.Along with SRHR, Abe also cares deeply about tackling climate change: "In my role as a youth worker and activist, I tell people to fight climate change: to grow more mangroves and to clean up the beach. Because we love our Kiribati."Learn more about Abe Share on Twitter Share on Facebook Share via WhatsApp Share via Email Tanzania Creating safe spaces for young people to get healthcare services without judgement 20-year-old Zahra Amri has been working with Chama cha Uzazi na Malezi Bora Tanzania (UMATI) since she was 13. Starting out as a Youth Action Movement member, she then became a peer educator for young people and now works at UMATI’s Youth Center.“There are several issues that as youth we must talk about, no matter what,” says Zahra. “The community and parents have myths and misconceptions that youth should not be able to speak about sexual reproductive health. But this situation affects most adolescents who face many challenges in life.For Zahra, it’s imperative that young people are educated about how to identify and report gender-based violence (GBV), as well as learning all about menstruation (particularly for girls living in poverty), gender equality and more.Learn more about Zahra Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 24 April 2024
In Pictures: International Youth Day 2021
Last year, IPPF and our global Member Associations delivered a staggering 98.2 million sexual and reproductive health services to young people aged 25 and under – that’s approximately 45% of all services delivered. When young people are able to access and manage their sexual and reproductive health and rights (SRHR) with dignity and care, their chances of thriving in life increase, and as such we work with and for youth populations around the world in many ways. Take a look at some of the ways we have been involved with this and, more importantly, how young people themselves have been the driving force behind the fight for SRHR for all. Malawi Young volunteers connect their peers to information and contraceptive care Kondwani, a 22-year-old Youth Action Movement (YAM) volunteer, not only distributes condoms locally, she also challenges her peers to show her on a wooden model how to use them, because she knows that this can pose a problem for some people.Activities like this in hard-to-reach areas are one of many that the YAM delivers across Malawi. Trained and hosted by Youth Life Centres, which provide sexual and reproductive healthcare aimed at youth, volunteers like Kondwani meet up regularly and reach out to their peers in schools, universities, and on social media.Learn more about Kondwani Share on Twitter Share on Facebook Share via WhatsApp Share via Email Poland Defending human rights in the face of unrelenting attacks Nadia believes activism can change the world. Over the last few years in Poland, women’s reproductive choices have been stripped back at an alarming rate. The young activist wants to reverse this erosion of women’s rights by campaigning for better reproductive, labour and social rights across the country. Nadia is painfully aware that in Poland, where public discourse is dominated by men, the belief that “children and young women have no voice” still reigns.As a result of her activism, Nadia has become the target of visceral personal attacks online, unrelenting violent behaviour, sexism & discrimination – but she hasn't given up.Learn more about Nadia Share on Twitter Share on Facebook Share via WhatsApp Share via Email Mali Using street dance to teach about consent, contraception and more Abdoulaye Camara is the best dancer in the neighbourhood, and he’s not afraid to show it. But Abdoulaye’s moves aren't just for fun – he's head of the dance troupe of the Youth Action Movement, belonging to the Association Malienne pour la Protection et la Promotion de la Famille, which uses dance and comedy sketches to talk about sex.“We distract them with dance and humour and then we transmit those important messages about sex without offending them,” explains Abdoulaye. Sexuality, STIs, consent, early/unintended pregnancy, contraception, and more – no topic is off the table for Abdoulaye and his troupe. Learn more about Abdoulaye Share on Twitter Share on Facebook Share via WhatsApp Share via Email Aruba Providing information and contraceptive care to young people in school Access to information and contraceptives has always been a priority for Famia Planea Aruba (FPA) – whether through their office, a delivery service, or in schools. For over 15 years FPA has worked in partnership with one of the largest secondary schools on the island. The FPA team visits the school every month to provide guidance, counselling, and contraceptive care to students, and to help ensure they stay in school to complete their education.The FPA team works with students to build trust and ensure they feel safe to talk openly. This helps to provide a sense of consistency for the student and the team, who are better able to notice if something changes, and if a student needs a referral to a medical doctor or other organization for additional treatment.Learn more about FPA Share on Twitter Share on Facebook Share via WhatsApp Share via Email Indonesia Surviving an earthquake as a young mother during COVID-19 Shortly after becoming a mother at 18, Herlina’s home was struck by a powerful earthquake in January, forcing her and her baby Nur to flee. She had to deal with this terrifying situation alone, all during the COVID-19 pandemic as well.The Indonesia Planned Parenthood Association (IPPA) health volunteer team were able to support Herlina by providing sexual and reproductive healthcare services, specifically advising Herlina on postpartum care. The team also gave Herlina dignity kits, which included sanitary pads, underclothes, and soap to maintain proper hygiene, which is a common challenge in displaced communities.Learn more about Herlina Share on Twitter Share on Facebook Share via WhatsApp Share via Email Kiribati Abe the ‘Youth Warrior’ “It’s time to be talking about sexual and reproductive health and rights (SRHR) early on, let’s not wait until young people get in trouble.” Abe's voice reveals the energy and passion of someone who is doing what they were destined to do.He is a proud member of the LGBTI community, as well as of his local church – two worlds he tries to bring together in order to spread important healthcare messages among other young people.Along with SRHR, Abe also cares deeply about tackling climate change: "In my role as a youth worker and activist, I tell people to fight climate change: to grow more mangroves and to clean up the beach. Because we love our Kiribati."Learn more about Abe Share on Twitter Share on Facebook Share via WhatsApp Share via Email Tanzania Creating safe spaces for young people to get healthcare services without judgement 20-year-old Zahra Amri has been working with Chama cha Uzazi na Malezi Bora Tanzania (UMATI) since she was 13. Starting out as a Youth Action Movement member, she then became a peer educator for young people and now works at UMATI’s Youth Center.“There are several issues that as youth we must talk about, no matter what,” says Zahra. “The community and parents have myths and misconceptions that youth should not be able to speak about sexual reproductive health. But this situation affects most adolescents who face many challenges in life.For Zahra, it’s imperative that young people are educated about how to identify and report gender-based violence (GBV), as well as learning all about menstruation (particularly for girls living in poverty), gender equality and more.Learn more about Zahra Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 24 June 2021
Changing mindsets through medicine and motivation
“You work with people who have HIV? Why?” That was the question Dr. Gregory Boyce was asked by the young intern that stood before him. He had come to the hospital ward to visit a client who was known to be living with HIV. He approached the intern at the desk and gave his name and designation. The intern looked at him, confused and somewhat amused and asked the question that he has neither forgotten, nor understood to this day. However, this young intern’s question comes from a mindset that Dr. Boyce is working fervently to change. As Deputy Director of the Medical Research Foundation of Trinidad and Tobago (MRF), Dr. Boyce provides clinical and administrative support to a team of doctors and nurses providing care to their clients who are living with HIV. Due to MRF’s long-standing work in HIV research and healthcare, the Family Planning Association of Trinidad and Tobago (FPATT), has referred many clients to Dr. Boyce and his team, and especially clients from the LGBTI+ community. Providing specialist care and support “Persons coming to us from key populations, have very layered needs. They are facing unique challenges in addition to living with the virus. There is still that myth that being HIV positive means that you will positively die. Added to that, there’s the discrimination that the community faces in every aspect of their lives on a daily basis. As a staff, we’ve had to seek special training to guide the way we interact with these clients so that we can meet all their needs appropriately and sensitively,” explains Dr. Boyce. “Apart from medical interventions which are needed to ensure that our clients continue to live healthy lives, we focus heavily on their psychosocial needs. It’s easy to think that because a client is physically healthy that they are also emotionally healthy. We have clients that won’t leave abusive relationships because they think no one else would accept them. We have other clients that are dealing with long-term medication fatigue because they have been taking pills for over 10 years. With that sometimes comes depression and other drug addictions, which is why it’s necessary for us to maintain open and honest relationships to address those accompanying issues.” Making HIV a non-issue Dr Boyce has been committed to providing treatment and care to clients living with HIV for over 20 years. He had worked at the Port of Spain General Hospital after graduating, during which time, medicine for persons living with HIV was expensive and out of reach for many. A few years later, through government programmes, medicine became more affordable, and treatment centres were opening up across the island. However, Dr. Boyce realized that the mortality rate had not changed by much. He wondered why people were still dying from a virus when medicine was easily accessible. “That first conversation – giving a client the news that they’ve tested positive – is very important. We get to show them that HIV is not an impediment. Most times, with the wrong information, they start to draw up a list of things that they can no longer do, like go after a promotion or start a family. Then they go through life shrunken and unrecognizable, not the person they once were. So to answer that intern’s question about why I work with persons living with HIV: I want to make HIV a non-issue,” he states. Dr. Boyce hopes to see HIV disclosure become as acceptable as other chronic illnesses such as cancer or diabetes, where an entire family would work towards caring for the affected person, instead of alienating them. He also hopes to see more inclusion and tolerance towards persons living with HIV, especially those within the LGBTI+ community. “Until a gay or transgender person can walk the streets freely and not be jeered at by passers-by, we still have a long way to go. Until they can access treatment at any public facility without fear or judgment, we have a lot of work to do. It would take a lot of education to change the stigma and discrimination but there is absolutely no reason why another person’s life should be miserable because their expression is different to ours.” He commends the work of FPATT in upholding the sexual and reproductive health and rights of the LGBTI+ community, through ensuring that they have a safe and non-judgmental environment for treatment and care. He says that the Medical Research Foundation values the great relationship that the two organizations have had for years, even as FPATT works towards becoming its own full-service antiretroviral treatment site for persons living with HIV.

| 24 April 2024
Changing mindsets through medicine and motivation
“You work with people who have HIV? Why?” That was the question Dr. Gregory Boyce was asked by the young intern that stood before him. He had come to the hospital ward to visit a client who was known to be living with HIV. He approached the intern at the desk and gave his name and designation. The intern looked at him, confused and somewhat amused and asked the question that he has neither forgotten, nor understood to this day. However, this young intern’s question comes from a mindset that Dr. Boyce is working fervently to change. As Deputy Director of the Medical Research Foundation of Trinidad and Tobago (MRF), Dr. Boyce provides clinical and administrative support to a team of doctors and nurses providing care to their clients who are living with HIV. Due to MRF’s long-standing work in HIV research and healthcare, the Family Planning Association of Trinidad and Tobago (FPATT), has referred many clients to Dr. Boyce and his team, and especially clients from the LGBTI+ community. Providing specialist care and support “Persons coming to us from key populations, have very layered needs. They are facing unique challenges in addition to living with the virus. There is still that myth that being HIV positive means that you will positively die. Added to that, there’s the discrimination that the community faces in every aspect of their lives on a daily basis. As a staff, we’ve had to seek special training to guide the way we interact with these clients so that we can meet all their needs appropriately and sensitively,” explains Dr. Boyce. “Apart from medical interventions which are needed to ensure that our clients continue to live healthy lives, we focus heavily on their psychosocial needs. It’s easy to think that because a client is physically healthy that they are also emotionally healthy. We have clients that won’t leave abusive relationships because they think no one else would accept them. We have other clients that are dealing with long-term medication fatigue because they have been taking pills for over 10 years. With that sometimes comes depression and other drug addictions, which is why it’s necessary for us to maintain open and honest relationships to address those accompanying issues.” Making HIV a non-issue Dr Boyce has been committed to providing treatment and care to clients living with HIV for over 20 years. He had worked at the Port of Spain General Hospital after graduating, during which time, medicine for persons living with HIV was expensive and out of reach for many. A few years later, through government programmes, medicine became more affordable, and treatment centres were opening up across the island. However, Dr. Boyce realized that the mortality rate had not changed by much. He wondered why people were still dying from a virus when medicine was easily accessible. “That first conversation – giving a client the news that they’ve tested positive – is very important. We get to show them that HIV is not an impediment. Most times, with the wrong information, they start to draw up a list of things that they can no longer do, like go after a promotion or start a family. Then they go through life shrunken and unrecognizable, not the person they once were. So to answer that intern’s question about why I work with persons living with HIV: I want to make HIV a non-issue,” he states. Dr. Boyce hopes to see HIV disclosure become as acceptable as other chronic illnesses such as cancer or diabetes, where an entire family would work towards caring for the affected person, instead of alienating them. He also hopes to see more inclusion and tolerance towards persons living with HIV, especially those within the LGBTI+ community. “Until a gay or transgender person can walk the streets freely and not be jeered at by passers-by, we still have a long way to go. Until they can access treatment at any public facility without fear or judgment, we have a lot of work to do. It would take a lot of education to change the stigma and discrimination but there is absolutely no reason why another person’s life should be miserable because their expression is different to ours.” He commends the work of FPATT in upholding the sexual and reproductive health and rights of the LGBTI+ community, through ensuring that they have a safe and non-judgmental environment for treatment and care. He says that the Medical Research Foundation values the great relationship that the two organizations have had for years, even as FPATT works towards becoming its own full-service antiretroviral treatment site for persons living with HIV.

| 24 June 2021
Ensuring care for Trinidad and Tobago's LGBTI+ community
Public perceptions, a lack of education, and government policies contribute to the barriers and challenges to achieving equality for all. In a country as diverse as Trinidad and Tobago, this is especially acute for certain key populations, including the LGBTI+ community. For Brandy Rodriguez, Healthcare Navigator at the Family Planning Association of Trinidad and Tobago (FPATT), the struggle is both real and personal. In 1999, Brandy began her transition to womanhood and since 2006 has been working with FPATT in their HIV programme for the LGBTI+ community. “Back in 2004, very little was said about HIV infection, transmission and prevention. In fact, if there was any information, it was misconstrued and meant to stigmatize the LGBTI+ community. I was fairly new to the transgender community, so I made it a mission to research and find out the truths behind HIV and how I could protect myself. I then felt like I had to share what I found with others who were searching as well,” she said. Overcoming prejudice and stigma That’s when FPATT asked Brandy to join their team in educating the LGBTI+ community on the types of healthcare available. Stigma surrounding the community forced many to stay hidden and avoid seeking care. Even if a member of the LGBTI+ community wanted to test for their HIV status, they would never dare to go into a public health centre, because of the fear of being judged by the healthcare professionals. “It’s a simple case of this. When a transgender or non-binary person walks into a health centre or hospital, and the triage nurse has to fill in a form that asks for gender, the only two options there are male and female. So usually, the non-binary person knows that if they want to access that healthcare, free of judgement, they would have to dress as the gender that would bring less attention. At the end of the day, the healthcare provider does not receive accurate information about the client, and the client doesn’t receive the scope of assessment and treatment that may be necessary. So part of what I do, is to simply accompany the client to the appointment so that it’s a less stressful experience and they don’t feel like they are alone,” says Brandy. The importance of access to HIV treatment and care Apart from a great lack of healthcare professionals that are willing to treat the LGBTI+ community non-judgementally, the community also lacks social support. Most of the members of the community face barriers to housing and employment, which often means earning a livelihood through sex work. Over 95% of skilled and employable persons within the LGBTI+ community have turned to sex work because they are constantly denied employment within other industries. “When I began my transition, I was fortunate to have the support of my family; they understood my heart and my need to be my authentic self. Not everyone has that support and so some either migrate or are left homeless because of the fact. Having to work within the sex industry means that they are now at greater risk for HIV or other STIs. My job as an Educator and Navigator is to promote condom use and ensure that they make use of FPATT’s regular HIV testing. If they do test positive, we then have that conversation about U=U, which means that if they [their HIV viral load] are undetectable, they will be untransferable, and then get them to that place of undetectability.” Brandy explains that being undetectable means that the client’s viral load is suppressed, and they are living healthy lives. The team works hard to ensure clients living with HIV enrol in the FPATT Programme, which supports the importance of adhering to consistent treatment, healthy eating, and rest. As well as testing, the Programme offers sexual and reproductive health education on prevention against STIs and both group and one-to-one sessions to anyone who needs it. Advocating for support FPATT has, for many years, advocated for the sexual and reproductive rights of the LGBTI+ community, ensuring that it remains a safe place for HIV testing and counselling. It holds a vision of a world where gender or sexuality are no longer a source of inequality or stigma. FPATT is poised to become a full-service HIV treatment site, offering antiretroviral treatment as well as psychosocial services for persons affected by HIV. FPATT’s goal is to stop discrimination and stigma against persons living with HIV and ultimately end the spread of HIV within Trinidad and Tobago by 2030.

| 24 April 2024
Ensuring care for Trinidad and Tobago's LGBTI+ community
Public perceptions, a lack of education, and government policies contribute to the barriers and challenges to achieving equality for all. In a country as diverse as Trinidad and Tobago, this is especially acute for certain key populations, including the LGBTI+ community. For Brandy Rodriguez, Healthcare Navigator at the Family Planning Association of Trinidad and Tobago (FPATT), the struggle is both real and personal. In 1999, Brandy began her transition to womanhood and since 2006 has been working with FPATT in their HIV programme for the LGBTI+ community. “Back in 2004, very little was said about HIV infection, transmission and prevention. In fact, if there was any information, it was misconstrued and meant to stigmatize the LGBTI+ community. I was fairly new to the transgender community, so I made it a mission to research and find out the truths behind HIV and how I could protect myself. I then felt like I had to share what I found with others who were searching as well,” she said. Overcoming prejudice and stigma That’s when FPATT asked Brandy to join their team in educating the LGBTI+ community on the types of healthcare available. Stigma surrounding the community forced many to stay hidden and avoid seeking care. Even if a member of the LGBTI+ community wanted to test for their HIV status, they would never dare to go into a public health centre, because of the fear of being judged by the healthcare professionals. “It’s a simple case of this. When a transgender or non-binary person walks into a health centre or hospital, and the triage nurse has to fill in a form that asks for gender, the only two options there are male and female. So usually, the non-binary person knows that if they want to access that healthcare, free of judgement, they would have to dress as the gender that would bring less attention. At the end of the day, the healthcare provider does not receive accurate information about the client, and the client doesn’t receive the scope of assessment and treatment that may be necessary. So part of what I do, is to simply accompany the client to the appointment so that it’s a less stressful experience and they don’t feel like they are alone,” says Brandy. The importance of access to HIV treatment and care Apart from a great lack of healthcare professionals that are willing to treat the LGBTI+ community non-judgementally, the community also lacks social support. Most of the members of the community face barriers to housing and employment, which often means earning a livelihood through sex work. Over 95% of skilled and employable persons within the LGBTI+ community have turned to sex work because they are constantly denied employment within other industries. “When I began my transition, I was fortunate to have the support of my family; they understood my heart and my need to be my authentic self. Not everyone has that support and so some either migrate or are left homeless because of the fact. Having to work within the sex industry means that they are now at greater risk for HIV or other STIs. My job as an Educator and Navigator is to promote condom use and ensure that they make use of FPATT’s regular HIV testing. If they do test positive, we then have that conversation about U=U, which means that if they [their HIV viral load] are undetectable, they will be untransferable, and then get them to that place of undetectability.” Brandy explains that being undetectable means that the client’s viral load is suppressed, and they are living healthy lives. The team works hard to ensure clients living with HIV enrol in the FPATT Programme, which supports the importance of adhering to consistent treatment, healthy eating, and rest. As well as testing, the Programme offers sexual and reproductive health education on prevention against STIs and both group and one-to-one sessions to anyone who needs it. Advocating for support FPATT has, for many years, advocated for the sexual and reproductive rights of the LGBTI+ community, ensuring that it remains a safe place for HIV testing and counselling. It holds a vision of a world where gender or sexuality are no longer a source of inequality or stigma. FPATT is poised to become a full-service HIV treatment site, offering antiretroviral treatment as well as psychosocial services for persons affected by HIV. FPATT’s goal is to stop discrimination and stigma against persons living with HIV and ultimately end the spread of HIV within Trinidad and Tobago by 2030.

| 26 May 2021
COVID-19 inspires new approach to reaching young people during lockdown
Provision of sexual and reproductive healthcare for all, regardless of age, is at the core of Famia Planea Aruba’s (FPA) work. Over the years FPA has developed different information packages specifically aimed at reaching and supporting young people, families, and educators. The inspiration for delivering comprehensive sexuality education digitally to young people was propelled by the COVID-19 lockdown. Like other frontline healthcare providers, FPA was faced with unforeseen challenges about how to continue reaching their communities. Undeterred, the team embraced the challenge to create, develop, and launch FPA’s first Online Puberty Educational News Program (OPEN). Responding to clients' needs digitally “In the last few years, FPA’s in-school Comprehensive Sexuality Education (CSE) program was growing rapidly, and then all of a sudden we hit a wall; our Island was in complete lockdown and all schools were closed. At first, we were very sad, since we were fully booked for the upcoming few months, and would lose the opportunity to reach thousands of young people”, says Evelyn Yarzagaray, FPA’s Executive Director. Typically, during April and May FPA usually focuses on students between the ages of 11 and 13 and supporting with the transition from elementary school to secondary school. At this age young people are starting to experience changes to their bodies and hormones. “We were all of a sudden bombarded with parents who started requesting one-on-one counselling sessions for their kids, but due to safety regulations this was not an easy option. That was when we started looking for a way to reach both parent and child in the safety of their own homes. By converting materials used during our in-person CSE program, we developed an educational video that can be viewed by both parent and child”, says Evelyn. The OPEN platform has been designed with a colourful background, emojis, and animation to appeal to its target audience. Users can access valuable information through the FAQ section, international news, and video content such as an interview with a Family Physician. “The filming and editing were the longest and most difficult part of the entire process, but once it was launched, we immediately saw that is was completely worth it, reaching over 42,000 people on social media”, Evelyn says. “I know it's all part of the growing up process” Jeanira, 37, is a doctor’s assistant and has two young children aged two and 12. She has been a member of FPA for many years, but only recently learned that FPA provides healthcare for all ages and stages of life – particularly young people. “About a year ago I had begun researching the best way and time to start talking to my daughter about her upcoming body changes, sexuality, and puberty in general”, explains Jeanira. It was a family member who suggested the FPA video on social media about puberty that was in Jeanira’s native language. “The video is fun, educational, featured local professionals and related to my daughter’s age. I love the fact that I could introduce the video to her and let her watch it in her own comfort zone. At the end, it did stimulate conversations and questions for a few days after and it truly made it easier for us to talk about some of the topics that can sometimes be a little hard to approach”, says Jeanira. 11-year-old Xiqiën really enjoyed the video: “My favourite part was to be able to recognize some changes that I am going through right now. There are some changes that I would like to skip but I know it’s all part of the growing up process. I’m so thankful that FPA had the idea to make such a fun video for us to learn from. There was some stuff that I already knew, but I also learned some new things. I did ask my mom a lot of questions after the video, mostly because they said that everyone is different, and I really wanted to know how my mom is different from me. I don’t feel quite as worried to talk to my mom about these things anymore, I know that she will try to help.”

| 24 April 2024
COVID-19 inspires new approach to reaching young people during lockdown
Provision of sexual and reproductive healthcare for all, regardless of age, is at the core of Famia Planea Aruba’s (FPA) work. Over the years FPA has developed different information packages specifically aimed at reaching and supporting young people, families, and educators. The inspiration for delivering comprehensive sexuality education digitally to young people was propelled by the COVID-19 lockdown. Like other frontline healthcare providers, FPA was faced with unforeseen challenges about how to continue reaching their communities. Undeterred, the team embraced the challenge to create, develop, and launch FPA’s first Online Puberty Educational News Program (OPEN). Responding to clients' needs digitally “In the last few years, FPA’s in-school Comprehensive Sexuality Education (CSE) program was growing rapidly, and then all of a sudden we hit a wall; our Island was in complete lockdown and all schools were closed. At first, we were very sad, since we were fully booked for the upcoming few months, and would lose the opportunity to reach thousands of young people”, says Evelyn Yarzagaray, FPA’s Executive Director. Typically, during April and May FPA usually focuses on students between the ages of 11 and 13 and supporting with the transition from elementary school to secondary school. At this age young people are starting to experience changes to their bodies and hormones. “We were all of a sudden bombarded with parents who started requesting one-on-one counselling sessions for their kids, but due to safety regulations this was not an easy option. That was when we started looking for a way to reach both parent and child in the safety of their own homes. By converting materials used during our in-person CSE program, we developed an educational video that can be viewed by both parent and child”, says Evelyn. The OPEN platform has been designed with a colourful background, emojis, and animation to appeal to its target audience. Users can access valuable information through the FAQ section, international news, and video content such as an interview with a Family Physician. “The filming and editing were the longest and most difficult part of the entire process, but once it was launched, we immediately saw that is was completely worth it, reaching over 42,000 people on social media”, Evelyn says. “I know it's all part of the growing up process” Jeanira, 37, is a doctor’s assistant and has two young children aged two and 12. She has been a member of FPA for many years, but only recently learned that FPA provides healthcare for all ages and stages of life – particularly young people. “About a year ago I had begun researching the best way and time to start talking to my daughter about her upcoming body changes, sexuality, and puberty in general”, explains Jeanira. It was a family member who suggested the FPA video on social media about puberty that was in Jeanira’s native language. “The video is fun, educational, featured local professionals and related to my daughter’s age. I love the fact that I could introduce the video to her and let her watch it in her own comfort zone. At the end, it did stimulate conversations and questions for a few days after and it truly made it easier for us to talk about some of the topics that can sometimes be a little hard to approach”, says Jeanira. 11-year-old Xiqiën really enjoyed the video: “My favourite part was to be able to recognize some changes that I am going through right now. There are some changes that I would like to skip but I know it’s all part of the growing up process. I’m so thankful that FPA had the idea to make such a fun video for us to learn from. There was some stuff that I already knew, but I also learned some new things. I did ask my mom a lot of questions after the video, mostly because they said that everyone is different, and I really wanted to know how my mom is different from me. I don’t feel quite as worried to talk to my mom about these things anymore, I know that she will try to help.”

| 26 May 2021
Providing information and contraceptive care to young people in school
Accessibility to information and contraceptives has always been a priority for Famia Planea Aruba (FPA) – whether through the office, delivery service, or in schools. For over 15 years FPA has worked in partnership with one of the largest secondary schools on the island. The FPA team visits the school every month to provide guidance, counselling, and contraceptive care to students, and to help ensure they stay in school to complete their education. “One of my first experiences providing comprehensive sex education with FPA was at the EPB School, during my education as a social worker. Many years later I still very much enjoy this”, says Richenella, FPA’s Finance and Information, Education and Communication (IEC) support staff. Building trust FPA’s client is at the heart of its healthcare provision. The FPA team works with students to build trust and ensure they feel safe to talk openly. This helps to provide a sense of consistency for the student, as well as efficiency for the team being familiar with specific students and cases. They are better able to notice if something changes, and if a student needs a referral to a medical doctor or other organization for additional treatment. “The consultations are always fun; you get a change of scenery by stepping out of the office. Over the years you see so many faces and still somehow you manage to remember most of them. After just a few visits you can start to build a profile of most students; you can start to tell who the class clown is, the Mister Popular, the shy one, the loud one, and the one who just wants to take his time to avoid going back to class”, Richenella laughs. Working in partnership with the school social worker FPA places great value on the 14-year relationship they have with Adriana, the social worker at EPB San Nicolas School. Adriana is the person who has the most contact with the students, and the one most student’s turn to when they need help. “Most of the time you get to have fun with the students, however every now and then you will come across a heartbreaking case. Since Aruba has so many different migrants, very often you will come across one person who is not insured at the moment, who needs products and can’t afford it – and you figure out a way to help”, Adriana says. For registered youth under 21 years of age, the costs of the healthcare provision are covered by the national health insurance, however, some students fall outside of the system. “For our second, third and fourth-year students, FPA has been collaborating with us to provide a monthly session where the students receive contraceptives and guidance on school grounds. Since around this age, most of our students are already sexually active, we try to help them stay safe in and out of school.” “The love, patience, and dedication that FPA has shown our students over the years are outstanding. At the beginning of the COVID-19 crisis we had to stop the consultation hours, but thankfully we are now back at it, bigger and better. Due to the collaboration with FPA we were able to finish out our 2018-2019 school year with no new pregnancies, which was a first for our school. We hope to accomplish this again, now that we can continue our consultations, and keep our kids educated and in school for as long as we can so they can achieve the best possible future”, Adriana says.

| 24 April 2024
Providing information and contraceptive care to young people in school
Accessibility to information and contraceptives has always been a priority for Famia Planea Aruba (FPA) – whether through the office, delivery service, or in schools. For over 15 years FPA has worked in partnership with one of the largest secondary schools on the island. The FPA team visits the school every month to provide guidance, counselling, and contraceptive care to students, and to help ensure they stay in school to complete their education. “One of my first experiences providing comprehensive sex education with FPA was at the EPB School, during my education as a social worker. Many years later I still very much enjoy this”, says Richenella, FPA’s Finance and Information, Education and Communication (IEC) support staff. Building trust FPA’s client is at the heart of its healthcare provision. The FPA team works with students to build trust and ensure they feel safe to talk openly. This helps to provide a sense of consistency for the student, as well as efficiency for the team being familiar with specific students and cases. They are better able to notice if something changes, and if a student needs a referral to a medical doctor or other organization for additional treatment. “The consultations are always fun; you get a change of scenery by stepping out of the office. Over the years you see so many faces and still somehow you manage to remember most of them. After just a few visits you can start to build a profile of most students; you can start to tell who the class clown is, the Mister Popular, the shy one, the loud one, and the one who just wants to take his time to avoid going back to class”, Richenella laughs. Working in partnership with the school social worker FPA places great value on the 14-year relationship they have with Adriana, the social worker at EPB San Nicolas School. Adriana is the person who has the most contact with the students, and the one most student’s turn to when they need help. “Most of the time you get to have fun with the students, however every now and then you will come across a heartbreaking case. Since Aruba has so many different migrants, very often you will come across one person who is not insured at the moment, who needs products and can’t afford it – and you figure out a way to help”, Adriana says. For registered youth under 21 years of age, the costs of the healthcare provision are covered by the national health insurance, however, some students fall outside of the system. “For our second, third and fourth-year students, FPA has been collaborating with us to provide a monthly session where the students receive contraceptives and guidance on school grounds. Since around this age, most of our students are already sexually active, we try to help them stay safe in and out of school.” “The love, patience, and dedication that FPA has shown our students over the years are outstanding. At the beginning of the COVID-19 crisis we had to stop the consultation hours, but thankfully we are now back at it, bigger and better. Due to the collaboration with FPA we were able to finish out our 2018-2019 school year with no new pregnancies, which was a first for our school. We hope to accomplish this again, now that we can continue our consultations, and keep our kids educated and in school for as long as we can so they can achieve the best possible future”, Adriana says.

| 17 August 2021
In pictures: World Humanitarian Day 2021
This World Humanitarian Day we reflect on the incredible work undertaken by our humanitarian response teams over the last 12 months. Last year, IPPF reached approximately 5.5 million people in humanitarian crises through our local Member Associations. This achievement would not have been possible without the dedicated and heroic healthcare teams providing vital sexual and reproductive healthcare in the most fragile humanitarian settings. COVID-19 response in Papua New Guinea Papua New Guinea Family Health Association (PNGFHA) PNGFHA responded to the COVID-19 outbreak in PNG, supported by the Australian government. With access to emergency healthcare facilities now extremely limited, PNGFHA health workers travel to hard-to-reach areas providing sexual and reproductive healthcare to the most marginalized communities.Clients like Vavine Kila receive a consultation at the PNGFHA mobile clinic. Share on Twitter Share on Facebook Share via WhatsApp Share via Email The humanitarian response teams taking healthcare into people's homes in Gaza Palestinian Family Planning and Protection Association (PFPPA) On 10 May 2021, Israel launched airstrikes on the Gaza Strip, killing over 220 people (including women and children) and leaving over 75,000 displaced. At the time, an estimated 87,000 women in the Gaza Strip and nearby areas were pregnant. The PFPPA humanitarian response team visited families in their homes, with each household expected to have four to five women of reproductive age needing healthcare. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Offering holistic care to families in Gaza Palestinian Family Planning and Protection Association (PFPPA) Children account for close to 50% of the population in Gaza. As part of the response, PFPPA youth volunteers entertained the children while their family members received life-saving sexual and reproductive healthcare and psychosocial support by the humanitarian response teams in privacy. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Ensuring ante- and post-natal care in the aftermath of an earthquake in West Sulawesi Indonesia Planned Parenthood Association (IPPA) On 15 January 2021, a 6.2 magnitude earthquake struck the West Sulawesi province in Indonesia leaving over 15,000 displaced, including many pregnant people and nursing mothers.As part of its response efforts, the IPPA set up mobile clinics near the shelters to provide vital ante- and post-natal care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email A super cyclone and a pandemic Family Planning Association of India (FPAI) On 20 May 2020, severe Cyclone Amphan hit the Indian state of West Bengal, affecting millions of people in and around the state capital Kolkata. Emergency crises during the COVID-19 pandemic intensifies the impact of the disaster and puts a strain on health systems and access to sexual and reproductive healthcare.FPAI responded by providing emergency sexual and reproductive healthcare to affected communities, particularly focusing on the most marginalized and vulnerable people including the LGBTI community, sex workers, pregnant women, and survivors of sexual and gender-based violence (SGBV). Share on Twitter Share on Facebook Share via WhatsApp Share via Email Providing healthcare to hardest hit communities after Cyclone Yasa The Reproductive and Family Health Association of Fiji (RFHAF) In mid-December 2020, a category 5 severe Tropical Cyclone Yasa hit the island of Fiji and neighbouring Lau group of Islands. IPPF’s Member Association, RFHAF, was supported by the Australian government to provide life-saving sexual and reproductive healthcare in the hardest hit communities, including counselling on STI risk reduction, first-line support for survivors of SGBV, and contraceptive and ante-natal care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 24 April 2024
In pictures: World Humanitarian Day 2021
This World Humanitarian Day we reflect on the incredible work undertaken by our humanitarian response teams over the last 12 months. Last year, IPPF reached approximately 5.5 million people in humanitarian crises through our local Member Associations. This achievement would not have been possible without the dedicated and heroic healthcare teams providing vital sexual and reproductive healthcare in the most fragile humanitarian settings. COVID-19 response in Papua New Guinea Papua New Guinea Family Health Association (PNGFHA) PNGFHA responded to the COVID-19 outbreak in PNG, supported by the Australian government. With access to emergency healthcare facilities now extremely limited, PNGFHA health workers travel to hard-to-reach areas providing sexual and reproductive healthcare to the most marginalized communities.Clients like Vavine Kila receive a consultation at the PNGFHA mobile clinic. Share on Twitter Share on Facebook Share via WhatsApp Share via Email The humanitarian response teams taking healthcare into people's homes in Gaza Palestinian Family Planning and Protection Association (PFPPA) On 10 May 2021, Israel launched airstrikes on the Gaza Strip, killing over 220 people (including women and children) and leaving over 75,000 displaced. At the time, an estimated 87,000 women in the Gaza Strip and nearby areas were pregnant. The PFPPA humanitarian response team visited families in their homes, with each household expected to have four to five women of reproductive age needing healthcare. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Offering holistic care to families in Gaza Palestinian Family Planning and Protection Association (PFPPA) Children account for close to 50% of the population in Gaza. As part of the response, PFPPA youth volunteers entertained the children while their family members received life-saving sexual and reproductive healthcare and psychosocial support by the humanitarian response teams in privacy. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Ensuring ante- and post-natal care in the aftermath of an earthquake in West Sulawesi Indonesia Planned Parenthood Association (IPPA) On 15 January 2021, a 6.2 magnitude earthquake struck the West Sulawesi province in Indonesia leaving over 15,000 displaced, including many pregnant people and nursing mothers.As part of its response efforts, the IPPA set up mobile clinics near the shelters to provide vital ante- and post-natal care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email A super cyclone and a pandemic Family Planning Association of India (FPAI) On 20 May 2020, severe Cyclone Amphan hit the Indian state of West Bengal, affecting millions of people in and around the state capital Kolkata. Emergency crises during the COVID-19 pandemic intensifies the impact of the disaster and puts a strain on health systems and access to sexual and reproductive healthcare.FPAI responded by providing emergency sexual and reproductive healthcare to affected communities, particularly focusing on the most marginalized and vulnerable people including the LGBTI community, sex workers, pregnant women, and survivors of sexual and gender-based violence (SGBV). Share on Twitter Share on Facebook Share via WhatsApp Share via Email Providing healthcare to hardest hit communities after Cyclone Yasa The Reproductive and Family Health Association of Fiji (RFHAF) In mid-December 2020, a category 5 severe Tropical Cyclone Yasa hit the island of Fiji and neighbouring Lau group of Islands. IPPF’s Member Association, RFHAF, was supported by the Australian government to provide life-saving sexual and reproductive healthcare in the hardest hit communities, including counselling on STI risk reduction, first-line support for survivors of SGBV, and contraceptive and ante-natal care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 10 August 2021
In Pictures: International Youth Day 2021
Last year, IPPF and our global Member Associations delivered a staggering 98.2 million sexual and reproductive health services to young people aged 25 and under – that’s approximately 45% of all services delivered. When young people are able to access and manage their sexual and reproductive health and rights (SRHR) with dignity and care, their chances of thriving in life increase, and as such we work with and for youth populations around the world in many ways. Take a look at some of the ways we have been involved with this and, more importantly, how young people themselves have been the driving force behind the fight for SRHR for all. Malawi Young volunteers connect their peers to information and contraceptive care Kondwani, a 22-year-old Youth Action Movement (YAM) volunteer, not only distributes condoms locally, she also challenges her peers to show her on a wooden model how to use them, because she knows that this can pose a problem for some people.Activities like this in hard-to-reach areas are one of many that the YAM delivers across Malawi. Trained and hosted by Youth Life Centres, which provide sexual and reproductive healthcare aimed at youth, volunteers like Kondwani meet up regularly and reach out to their peers in schools, universities, and on social media.Learn more about Kondwani Share on Twitter Share on Facebook Share via WhatsApp Share via Email Poland Defending human rights in the face of unrelenting attacks Nadia believes activism can change the world. Over the last few years in Poland, women’s reproductive choices have been stripped back at an alarming rate. The young activist wants to reverse this erosion of women’s rights by campaigning for better reproductive, labour and social rights across the country. Nadia is painfully aware that in Poland, where public discourse is dominated by men, the belief that “children and young women have no voice” still reigns.As a result of her activism, Nadia has become the target of visceral personal attacks online, unrelenting violent behaviour, sexism & discrimination – but she hasn't given up.Learn more about Nadia Share on Twitter Share on Facebook Share via WhatsApp Share via Email Mali Using street dance to teach about consent, contraception and more Abdoulaye Camara is the best dancer in the neighbourhood, and he’s not afraid to show it. But Abdoulaye’s moves aren't just for fun – he's head of the dance troupe of the Youth Action Movement, belonging to the Association Malienne pour la Protection et la Promotion de la Famille, which uses dance and comedy sketches to talk about sex.“We distract them with dance and humour and then we transmit those important messages about sex without offending them,” explains Abdoulaye. Sexuality, STIs, consent, early/unintended pregnancy, contraception, and more – no topic is off the table for Abdoulaye and his troupe. Learn more about Abdoulaye Share on Twitter Share on Facebook Share via WhatsApp Share via Email Aruba Providing information and contraceptive care to young people in school Access to information and contraceptives has always been a priority for Famia Planea Aruba (FPA) – whether through their office, a delivery service, or in schools. For over 15 years FPA has worked in partnership with one of the largest secondary schools on the island. The FPA team visits the school every month to provide guidance, counselling, and contraceptive care to students, and to help ensure they stay in school to complete their education.The FPA team works with students to build trust and ensure they feel safe to talk openly. This helps to provide a sense of consistency for the student and the team, who are better able to notice if something changes, and if a student needs a referral to a medical doctor or other organization for additional treatment.Learn more about FPA Share on Twitter Share on Facebook Share via WhatsApp Share via Email Indonesia Surviving an earthquake as a young mother during COVID-19 Shortly after becoming a mother at 18, Herlina’s home was struck by a powerful earthquake in January, forcing her and her baby Nur to flee. She had to deal with this terrifying situation alone, all during the COVID-19 pandemic as well.The Indonesia Planned Parenthood Association (IPPA) health volunteer team were able to support Herlina by providing sexual and reproductive healthcare services, specifically advising Herlina on postpartum care. The team also gave Herlina dignity kits, which included sanitary pads, underclothes, and soap to maintain proper hygiene, which is a common challenge in displaced communities.Learn more about Herlina Share on Twitter Share on Facebook Share via WhatsApp Share via Email Kiribati Abe the ‘Youth Warrior’ “It’s time to be talking about sexual and reproductive health and rights (SRHR) early on, let’s not wait until young people get in trouble.” Abe's voice reveals the energy and passion of someone who is doing what they were destined to do.He is a proud member of the LGBTI community, as well as of his local church – two worlds he tries to bring together in order to spread important healthcare messages among other young people.Along with SRHR, Abe also cares deeply about tackling climate change: "In my role as a youth worker and activist, I tell people to fight climate change: to grow more mangroves and to clean up the beach. Because we love our Kiribati."Learn more about Abe Share on Twitter Share on Facebook Share via WhatsApp Share via Email Tanzania Creating safe spaces for young people to get healthcare services without judgement 20-year-old Zahra Amri has been working with Chama cha Uzazi na Malezi Bora Tanzania (UMATI) since she was 13. Starting out as a Youth Action Movement member, she then became a peer educator for young people and now works at UMATI’s Youth Center.“There are several issues that as youth we must talk about, no matter what,” says Zahra. “The community and parents have myths and misconceptions that youth should not be able to speak about sexual reproductive health. But this situation affects most adolescents who face many challenges in life.For Zahra, it’s imperative that young people are educated about how to identify and report gender-based violence (GBV), as well as learning all about menstruation (particularly for girls living in poverty), gender equality and more.Learn more about Zahra Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 24 April 2024
In Pictures: International Youth Day 2021
Last year, IPPF and our global Member Associations delivered a staggering 98.2 million sexual and reproductive health services to young people aged 25 and under – that’s approximately 45% of all services delivered. When young people are able to access and manage their sexual and reproductive health and rights (SRHR) with dignity and care, their chances of thriving in life increase, and as such we work with and for youth populations around the world in many ways. Take a look at some of the ways we have been involved with this and, more importantly, how young people themselves have been the driving force behind the fight for SRHR for all. Malawi Young volunteers connect their peers to information and contraceptive care Kondwani, a 22-year-old Youth Action Movement (YAM) volunteer, not only distributes condoms locally, she also challenges her peers to show her on a wooden model how to use them, because she knows that this can pose a problem for some people.Activities like this in hard-to-reach areas are one of many that the YAM delivers across Malawi. Trained and hosted by Youth Life Centres, which provide sexual and reproductive healthcare aimed at youth, volunteers like Kondwani meet up regularly and reach out to their peers in schools, universities, and on social media.Learn more about Kondwani Share on Twitter Share on Facebook Share via WhatsApp Share via Email Poland Defending human rights in the face of unrelenting attacks Nadia believes activism can change the world. Over the last few years in Poland, women’s reproductive choices have been stripped back at an alarming rate. The young activist wants to reverse this erosion of women’s rights by campaigning for better reproductive, labour and social rights across the country. Nadia is painfully aware that in Poland, where public discourse is dominated by men, the belief that “children and young women have no voice” still reigns.As a result of her activism, Nadia has become the target of visceral personal attacks online, unrelenting violent behaviour, sexism & discrimination – but she hasn't given up.Learn more about Nadia Share on Twitter Share on Facebook Share via WhatsApp Share via Email Mali Using street dance to teach about consent, contraception and more Abdoulaye Camara is the best dancer in the neighbourhood, and he’s not afraid to show it. But Abdoulaye’s moves aren't just for fun – he's head of the dance troupe of the Youth Action Movement, belonging to the Association Malienne pour la Protection et la Promotion de la Famille, which uses dance and comedy sketches to talk about sex.“We distract them with dance and humour and then we transmit those important messages about sex without offending them,” explains Abdoulaye. Sexuality, STIs, consent, early/unintended pregnancy, contraception, and more – no topic is off the table for Abdoulaye and his troupe. Learn more about Abdoulaye Share on Twitter Share on Facebook Share via WhatsApp Share via Email Aruba Providing information and contraceptive care to young people in school Access to information and contraceptives has always been a priority for Famia Planea Aruba (FPA) – whether through their office, a delivery service, or in schools. For over 15 years FPA has worked in partnership with one of the largest secondary schools on the island. The FPA team visits the school every month to provide guidance, counselling, and contraceptive care to students, and to help ensure they stay in school to complete their education.The FPA team works with students to build trust and ensure they feel safe to talk openly. This helps to provide a sense of consistency for the student and the team, who are better able to notice if something changes, and if a student needs a referral to a medical doctor or other organization for additional treatment.Learn more about FPA Share on Twitter Share on Facebook Share via WhatsApp Share via Email Indonesia Surviving an earthquake as a young mother during COVID-19 Shortly after becoming a mother at 18, Herlina’s home was struck by a powerful earthquake in January, forcing her and her baby Nur to flee. She had to deal with this terrifying situation alone, all during the COVID-19 pandemic as well.The Indonesia Planned Parenthood Association (IPPA) health volunteer team were able to support Herlina by providing sexual and reproductive healthcare services, specifically advising Herlina on postpartum care. The team also gave Herlina dignity kits, which included sanitary pads, underclothes, and soap to maintain proper hygiene, which is a common challenge in displaced communities.Learn more about Herlina Share on Twitter Share on Facebook Share via WhatsApp Share via Email Kiribati Abe the ‘Youth Warrior’ “It’s time to be talking about sexual and reproductive health and rights (SRHR) early on, let’s not wait until young people get in trouble.” Abe's voice reveals the energy and passion of someone who is doing what they were destined to do.He is a proud member of the LGBTI community, as well as of his local church – two worlds he tries to bring together in order to spread important healthcare messages among other young people.Along with SRHR, Abe also cares deeply about tackling climate change: "In my role as a youth worker and activist, I tell people to fight climate change: to grow more mangroves and to clean up the beach. Because we love our Kiribati."Learn more about Abe Share on Twitter Share on Facebook Share via WhatsApp Share via Email Tanzania Creating safe spaces for young people to get healthcare services without judgement 20-year-old Zahra Amri has been working with Chama cha Uzazi na Malezi Bora Tanzania (UMATI) since she was 13. Starting out as a Youth Action Movement member, she then became a peer educator for young people and now works at UMATI’s Youth Center.“There are several issues that as youth we must talk about, no matter what,” says Zahra. “The community and parents have myths and misconceptions that youth should not be able to speak about sexual reproductive health. But this situation affects most adolescents who face many challenges in life.For Zahra, it’s imperative that young people are educated about how to identify and report gender-based violence (GBV), as well as learning all about menstruation (particularly for girls living in poverty), gender equality and more.Learn more about Zahra Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 24 June 2021
Changing mindsets through medicine and motivation
“You work with people who have HIV? Why?” That was the question Dr. Gregory Boyce was asked by the young intern that stood before him. He had come to the hospital ward to visit a client who was known to be living with HIV. He approached the intern at the desk and gave his name and designation. The intern looked at him, confused and somewhat amused and asked the question that he has neither forgotten, nor understood to this day. However, this young intern’s question comes from a mindset that Dr. Boyce is working fervently to change. As Deputy Director of the Medical Research Foundation of Trinidad and Tobago (MRF), Dr. Boyce provides clinical and administrative support to a team of doctors and nurses providing care to their clients who are living with HIV. Due to MRF’s long-standing work in HIV research and healthcare, the Family Planning Association of Trinidad and Tobago (FPATT), has referred many clients to Dr. Boyce and his team, and especially clients from the LGBTI+ community. Providing specialist care and support “Persons coming to us from key populations, have very layered needs. They are facing unique challenges in addition to living with the virus. There is still that myth that being HIV positive means that you will positively die. Added to that, there’s the discrimination that the community faces in every aspect of their lives on a daily basis. As a staff, we’ve had to seek special training to guide the way we interact with these clients so that we can meet all their needs appropriately and sensitively,” explains Dr. Boyce. “Apart from medical interventions which are needed to ensure that our clients continue to live healthy lives, we focus heavily on their psychosocial needs. It’s easy to think that because a client is physically healthy that they are also emotionally healthy. We have clients that won’t leave abusive relationships because they think no one else would accept them. We have other clients that are dealing with long-term medication fatigue because they have been taking pills for over 10 years. With that sometimes comes depression and other drug addictions, which is why it’s necessary for us to maintain open and honest relationships to address those accompanying issues.” Making HIV a non-issue Dr Boyce has been committed to providing treatment and care to clients living with HIV for over 20 years. He had worked at the Port of Spain General Hospital after graduating, during which time, medicine for persons living with HIV was expensive and out of reach for many. A few years later, through government programmes, medicine became more affordable, and treatment centres were opening up across the island. However, Dr. Boyce realized that the mortality rate had not changed by much. He wondered why people were still dying from a virus when medicine was easily accessible. “That first conversation – giving a client the news that they’ve tested positive – is very important. We get to show them that HIV is not an impediment. Most times, with the wrong information, they start to draw up a list of things that they can no longer do, like go after a promotion or start a family. Then they go through life shrunken and unrecognizable, not the person they once were. So to answer that intern’s question about why I work with persons living with HIV: I want to make HIV a non-issue,” he states. Dr. Boyce hopes to see HIV disclosure become as acceptable as other chronic illnesses such as cancer or diabetes, where an entire family would work towards caring for the affected person, instead of alienating them. He also hopes to see more inclusion and tolerance towards persons living with HIV, especially those within the LGBTI+ community. “Until a gay or transgender person can walk the streets freely and not be jeered at by passers-by, we still have a long way to go. Until they can access treatment at any public facility without fear or judgment, we have a lot of work to do. It would take a lot of education to change the stigma and discrimination but there is absolutely no reason why another person’s life should be miserable because their expression is different to ours.” He commends the work of FPATT in upholding the sexual and reproductive health and rights of the LGBTI+ community, through ensuring that they have a safe and non-judgmental environment for treatment and care. He says that the Medical Research Foundation values the great relationship that the two organizations have had for years, even as FPATT works towards becoming its own full-service antiretroviral treatment site for persons living with HIV.

| 24 April 2024
Changing mindsets through medicine and motivation
“You work with people who have HIV? Why?” That was the question Dr. Gregory Boyce was asked by the young intern that stood before him. He had come to the hospital ward to visit a client who was known to be living with HIV. He approached the intern at the desk and gave his name and designation. The intern looked at him, confused and somewhat amused and asked the question that he has neither forgotten, nor understood to this day. However, this young intern’s question comes from a mindset that Dr. Boyce is working fervently to change. As Deputy Director of the Medical Research Foundation of Trinidad and Tobago (MRF), Dr. Boyce provides clinical and administrative support to a team of doctors and nurses providing care to their clients who are living with HIV. Due to MRF’s long-standing work in HIV research and healthcare, the Family Planning Association of Trinidad and Tobago (FPATT), has referred many clients to Dr. Boyce and his team, and especially clients from the LGBTI+ community. Providing specialist care and support “Persons coming to us from key populations, have very layered needs. They are facing unique challenges in addition to living with the virus. There is still that myth that being HIV positive means that you will positively die. Added to that, there’s the discrimination that the community faces in every aspect of their lives on a daily basis. As a staff, we’ve had to seek special training to guide the way we interact with these clients so that we can meet all their needs appropriately and sensitively,” explains Dr. Boyce. “Apart from medical interventions which are needed to ensure that our clients continue to live healthy lives, we focus heavily on their psychosocial needs. It’s easy to think that because a client is physically healthy that they are also emotionally healthy. We have clients that won’t leave abusive relationships because they think no one else would accept them. We have other clients that are dealing with long-term medication fatigue because they have been taking pills for over 10 years. With that sometimes comes depression and other drug addictions, which is why it’s necessary for us to maintain open and honest relationships to address those accompanying issues.” Making HIV a non-issue Dr Boyce has been committed to providing treatment and care to clients living with HIV for over 20 years. He had worked at the Port of Spain General Hospital after graduating, during which time, medicine for persons living with HIV was expensive and out of reach for many. A few years later, through government programmes, medicine became more affordable, and treatment centres were opening up across the island. However, Dr. Boyce realized that the mortality rate had not changed by much. He wondered why people were still dying from a virus when medicine was easily accessible. “That first conversation – giving a client the news that they’ve tested positive – is very important. We get to show them that HIV is not an impediment. Most times, with the wrong information, they start to draw up a list of things that they can no longer do, like go after a promotion or start a family. Then they go through life shrunken and unrecognizable, not the person they once were. So to answer that intern’s question about why I work with persons living with HIV: I want to make HIV a non-issue,” he states. Dr. Boyce hopes to see HIV disclosure become as acceptable as other chronic illnesses such as cancer or diabetes, where an entire family would work towards caring for the affected person, instead of alienating them. He also hopes to see more inclusion and tolerance towards persons living with HIV, especially those within the LGBTI+ community. “Until a gay or transgender person can walk the streets freely and not be jeered at by passers-by, we still have a long way to go. Until they can access treatment at any public facility without fear or judgment, we have a lot of work to do. It would take a lot of education to change the stigma and discrimination but there is absolutely no reason why another person’s life should be miserable because their expression is different to ours.” He commends the work of FPATT in upholding the sexual and reproductive health and rights of the LGBTI+ community, through ensuring that they have a safe and non-judgmental environment for treatment and care. He says that the Medical Research Foundation values the great relationship that the two organizations have had for years, even as FPATT works towards becoming its own full-service antiretroviral treatment site for persons living with HIV.

| 24 June 2021
Ensuring care for Trinidad and Tobago's LGBTI+ community
Public perceptions, a lack of education, and government policies contribute to the barriers and challenges to achieving equality for all. In a country as diverse as Trinidad and Tobago, this is especially acute for certain key populations, including the LGBTI+ community. For Brandy Rodriguez, Healthcare Navigator at the Family Planning Association of Trinidad and Tobago (FPATT), the struggle is both real and personal. In 1999, Brandy began her transition to womanhood and since 2006 has been working with FPATT in their HIV programme for the LGBTI+ community. “Back in 2004, very little was said about HIV infection, transmission and prevention. In fact, if there was any information, it was misconstrued and meant to stigmatize the LGBTI+ community. I was fairly new to the transgender community, so I made it a mission to research and find out the truths behind HIV and how I could protect myself. I then felt like I had to share what I found with others who were searching as well,” she said. Overcoming prejudice and stigma That’s when FPATT asked Brandy to join their team in educating the LGBTI+ community on the types of healthcare available. Stigma surrounding the community forced many to stay hidden and avoid seeking care. Even if a member of the LGBTI+ community wanted to test for their HIV status, they would never dare to go into a public health centre, because of the fear of being judged by the healthcare professionals. “It’s a simple case of this. When a transgender or non-binary person walks into a health centre or hospital, and the triage nurse has to fill in a form that asks for gender, the only two options there are male and female. So usually, the non-binary person knows that if they want to access that healthcare, free of judgement, they would have to dress as the gender that would bring less attention. At the end of the day, the healthcare provider does not receive accurate information about the client, and the client doesn’t receive the scope of assessment and treatment that may be necessary. So part of what I do, is to simply accompany the client to the appointment so that it’s a less stressful experience and they don’t feel like they are alone,” says Brandy. The importance of access to HIV treatment and care Apart from a great lack of healthcare professionals that are willing to treat the LGBTI+ community non-judgementally, the community also lacks social support. Most of the members of the community face barriers to housing and employment, which often means earning a livelihood through sex work. Over 95% of skilled and employable persons within the LGBTI+ community have turned to sex work because they are constantly denied employment within other industries. “When I began my transition, I was fortunate to have the support of my family; they understood my heart and my need to be my authentic self. Not everyone has that support and so some either migrate or are left homeless because of the fact. Having to work within the sex industry means that they are now at greater risk for HIV or other STIs. My job as an Educator and Navigator is to promote condom use and ensure that they make use of FPATT’s regular HIV testing. If they do test positive, we then have that conversation about U=U, which means that if they [their HIV viral load] are undetectable, they will be untransferable, and then get them to that place of undetectability.” Brandy explains that being undetectable means that the client’s viral load is suppressed, and they are living healthy lives. The team works hard to ensure clients living with HIV enrol in the FPATT Programme, which supports the importance of adhering to consistent treatment, healthy eating, and rest. As well as testing, the Programme offers sexual and reproductive health education on prevention against STIs and both group and one-to-one sessions to anyone who needs it. Advocating for support FPATT has, for many years, advocated for the sexual and reproductive rights of the LGBTI+ community, ensuring that it remains a safe place for HIV testing and counselling. It holds a vision of a world where gender or sexuality are no longer a source of inequality or stigma. FPATT is poised to become a full-service HIV treatment site, offering antiretroviral treatment as well as psychosocial services for persons affected by HIV. FPATT’s goal is to stop discrimination and stigma against persons living with HIV and ultimately end the spread of HIV within Trinidad and Tobago by 2030.

| 24 April 2024
Ensuring care for Trinidad and Tobago's LGBTI+ community
Public perceptions, a lack of education, and government policies contribute to the barriers and challenges to achieving equality for all. In a country as diverse as Trinidad and Tobago, this is especially acute for certain key populations, including the LGBTI+ community. For Brandy Rodriguez, Healthcare Navigator at the Family Planning Association of Trinidad and Tobago (FPATT), the struggle is both real and personal. In 1999, Brandy began her transition to womanhood and since 2006 has been working with FPATT in their HIV programme for the LGBTI+ community. “Back in 2004, very little was said about HIV infection, transmission and prevention. In fact, if there was any information, it was misconstrued and meant to stigmatize the LGBTI+ community. I was fairly new to the transgender community, so I made it a mission to research and find out the truths behind HIV and how I could protect myself. I then felt like I had to share what I found with others who were searching as well,” she said. Overcoming prejudice and stigma That’s when FPATT asked Brandy to join their team in educating the LGBTI+ community on the types of healthcare available. Stigma surrounding the community forced many to stay hidden and avoid seeking care. Even if a member of the LGBTI+ community wanted to test for their HIV status, they would never dare to go into a public health centre, because of the fear of being judged by the healthcare professionals. “It’s a simple case of this. When a transgender or non-binary person walks into a health centre or hospital, and the triage nurse has to fill in a form that asks for gender, the only two options there are male and female. So usually, the non-binary person knows that if they want to access that healthcare, free of judgement, they would have to dress as the gender that would bring less attention. At the end of the day, the healthcare provider does not receive accurate information about the client, and the client doesn’t receive the scope of assessment and treatment that may be necessary. So part of what I do, is to simply accompany the client to the appointment so that it’s a less stressful experience and they don’t feel like they are alone,” says Brandy. The importance of access to HIV treatment and care Apart from a great lack of healthcare professionals that are willing to treat the LGBTI+ community non-judgementally, the community also lacks social support. Most of the members of the community face barriers to housing and employment, which often means earning a livelihood through sex work. Over 95% of skilled and employable persons within the LGBTI+ community have turned to sex work because they are constantly denied employment within other industries. “When I began my transition, I was fortunate to have the support of my family; they understood my heart and my need to be my authentic self. Not everyone has that support and so some either migrate or are left homeless because of the fact. Having to work within the sex industry means that they are now at greater risk for HIV or other STIs. My job as an Educator and Navigator is to promote condom use and ensure that they make use of FPATT’s regular HIV testing. If they do test positive, we then have that conversation about U=U, which means that if they [their HIV viral load] are undetectable, they will be untransferable, and then get them to that place of undetectability.” Brandy explains that being undetectable means that the client’s viral load is suppressed, and they are living healthy lives. The team works hard to ensure clients living with HIV enrol in the FPATT Programme, which supports the importance of adhering to consistent treatment, healthy eating, and rest. As well as testing, the Programme offers sexual and reproductive health education on prevention against STIs and both group and one-to-one sessions to anyone who needs it. Advocating for support FPATT has, for many years, advocated for the sexual and reproductive rights of the LGBTI+ community, ensuring that it remains a safe place for HIV testing and counselling. It holds a vision of a world where gender or sexuality are no longer a source of inequality or stigma. FPATT is poised to become a full-service HIV treatment site, offering antiretroviral treatment as well as psychosocial services for persons affected by HIV. FPATT’s goal is to stop discrimination and stigma against persons living with HIV and ultimately end the spread of HIV within Trinidad and Tobago by 2030.

| 26 May 2021
COVID-19 inspires new approach to reaching young people during lockdown
Provision of sexual and reproductive healthcare for all, regardless of age, is at the core of Famia Planea Aruba’s (FPA) work. Over the years FPA has developed different information packages specifically aimed at reaching and supporting young people, families, and educators. The inspiration for delivering comprehensive sexuality education digitally to young people was propelled by the COVID-19 lockdown. Like other frontline healthcare providers, FPA was faced with unforeseen challenges about how to continue reaching their communities. Undeterred, the team embraced the challenge to create, develop, and launch FPA’s first Online Puberty Educational News Program (OPEN). Responding to clients' needs digitally “In the last few years, FPA’s in-school Comprehensive Sexuality Education (CSE) program was growing rapidly, and then all of a sudden we hit a wall; our Island was in complete lockdown and all schools were closed. At first, we were very sad, since we were fully booked for the upcoming few months, and would lose the opportunity to reach thousands of young people”, says Evelyn Yarzagaray, FPA’s Executive Director. Typically, during April and May FPA usually focuses on students between the ages of 11 and 13 and supporting with the transition from elementary school to secondary school. At this age young people are starting to experience changes to their bodies and hormones. “We were all of a sudden bombarded with parents who started requesting one-on-one counselling sessions for their kids, but due to safety regulations this was not an easy option. That was when we started looking for a way to reach both parent and child in the safety of their own homes. By converting materials used during our in-person CSE program, we developed an educational video that can be viewed by both parent and child”, says Evelyn. The OPEN platform has been designed with a colourful background, emojis, and animation to appeal to its target audience. Users can access valuable information through the FAQ section, international news, and video content such as an interview with a Family Physician. “The filming and editing were the longest and most difficult part of the entire process, but once it was launched, we immediately saw that is was completely worth it, reaching over 42,000 people on social media”, Evelyn says. “I know it's all part of the growing up process” Jeanira, 37, is a doctor’s assistant and has two young children aged two and 12. She has been a member of FPA for many years, but only recently learned that FPA provides healthcare for all ages and stages of life – particularly young people. “About a year ago I had begun researching the best way and time to start talking to my daughter about her upcoming body changes, sexuality, and puberty in general”, explains Jeanira. It was a family member who suggested the FPA video on social media about puberty that was in Jeanira’s native language. “The video is fun, educational, featured local professionals and related to my daughter’s age. I love the fact that I could introduce the video to her and let her watch it in her own comfort zone. At the end, it did stimulate conversations and questions for a few days after and it truly made it easier for us to talk about some of the topics that can sometimes be a little hard to approach”, says Jeanira. 11-year-old Xiqiën really enjoyed the video: “My favourite part was to be able to recognize some changes that I am going through right now. There are some changes that I would like to skip but I know it’s all part of the growing up process. I’m so thankful that FPA had the idea to make such a fun video for us to learn from. There was some stuff that I already knew, but I also learned some new things. I did ask my mom a lot of questions after the video, mostly because they said that everyone is different, and I really wanted to know how my mom is different from me. I don’t feel quite as worried to talk to my mom about these things anymore, I know that she will try to help.”

| 24 April 2024
COVID-19 inspires new approach to reaching young people during lockdown
Provision of sexual and reproductive healthcare for all, regardless of age, is at the core of Famia Planea Aruba’s (FPA) work. Over the years FPA has developed different information packages specifically aimed at reaching and supporting young people, families, and educators. The inspiration for delivering comprehensive sexuality education digitally to young people was propelled by the COVID-19 lockdown. Like other frontline healthcare providers, FPA was faced with unforeseen challenges about how to continue reaching their communities. Undeterred, the team embraced the challenge to create, develop, and launch FPA’s first Online Puberty Educational News Program (OPEN). Responding to clients' needs digitally “In the last few years, FPA’s in-school Comprehensive Sexuality Education (CSE) program was growing rapidly, and then all of a sudden we hit a wall; our Island was in complete lockdown and all schools were closed. At first, we were very sad, since we were fully booked for the upcoming few months, and would lose the opportunity to reach thousands of young people”, says Evelyn Yarzagaray, FPA’s Executive Director. Typically, during April and May FPA usually focuses on students between the ages of 11 and 13 and supporting with the transition from elementary school to secondary school. At this age young people are starting to experience changes to their bodies and hormones. “We were all of a sudden bombarded with parents who started requesting one-on-one counselling sessions for their kids, but due to safety regulations this was not an easy option. That was when we started looking for a way to reach both parent and child in the safety of their own homes. By converting materials used during our in-person CSE program, we developed an educational video that can be viewed by both parent and child”, says Evelyn. The OPEN platform has been designed with a colourful background, emojis, and animation to appeal to its target audience. Users can access valuable information through the FAQ section, international news, and video content such as an interview with a Family Physician. “The filming and editing were the longest and most difficult part of the entire process, but once it was launched, we immediately saw that is was completely worth it, reaching over 42,000 people on social media”, Evelyn says. “I know it's all part of the growing up process” Jeanira, 37, is a doctor’s assistant and has two young children aged two and 12. She has been a member of FPA for many years, but only recently learned that FPA provides healthcare for all ages and stages of life – particularly young people. “About a year ago I had begun researching the best way and time to start talking to my daughter about her upcoming body changes, sexuality, and puberty in general”, explains Jeanira. It was a family member who suggested the FPA video on social media about puberty that was in Jeanira’s native language. “The video is fun, educational, featured local professionals and related to my daughter’s age. I love the fact that I could introduce the video to her and let her watch it in her own comfort zone. At the end, it did stimulate conversations and questions for a few days after and it truly made it easier for us to talk about some of the topics that can sometimes be a little hard to approach”, says Jeanira. 11-year-old Xiqiën really enjoyed the video: “My favourite part was to be able to recognize some changes that I am going through right now. There are some changes that I would like to skip but I know it’s all part of the growing up process. I’m so thankful that FPA had the idea to make such a fun video for us to learn from. There was some stuff that I already knew, but I also learned some new things. I did ask my mom a lot of questions after the video, mostly because they said that everyone is different, and I really wanted to know how my mom is different from me. I don’t feel quite as worried to talk to my mom about these things anymore, I know that she will try to help.”

| 26 May 2021
Providing information and contraceptive care to young people in school
Accessibility to information and contraceptives has always been a priority for Famia Planea Aruba (FPA) – whether through the office, delivery service, or in schools. For over 15 years FPA has worked in partnership with one of the largest secondary schools on the island. The FPA team visits the school every month to provide guidance, counselling, and contraceptive care to students, and to help ensure they stay in school to complete their education. “One of my first experiences providing comprehensive sex education with FPA was at the EPB School, during my education as a social worker. Many years later I still very much enjoy this”, says Richenella, FPA’s Finance and Information, Education and Communication (IEC) support staff. Building trust FPA’s client is at the heart of its healthcare provision. The FPA team works with students to build trust and ensure they feel safe to talk openly. This helps to provide a sense of consistency for the student, as well as efficiency for the team being familiar with specific students and cases. They are better able to notice if something changes, and if a student needs a referral to a medical doctor or other organization for additional treatment. “The consultations are always fun; you get a change of scenery by stepping out of the office. Over the years you see so many faces and still somehow you manage to remember most of them. After just a few visits you can start to build a profile of most students; you can start to tell who the class clown is, the Mister Popular, the shy one, the loud one, and the one who just wants to take his time to avoid going back to class”, Richenella laughs. Working in partnership with the school social worker FPA places great value on the 14-year relationship they have with Adriana, the social worker at EPB San Nicolas School. Adriana is the person who has the most contact with the students, and the one most student’s turn to when they need help. “Most of the time you get to have fun with the students, however every now and then you will come across a heartbreaking case. Since Aruba has so many different migrants, very often you will come across one person who is not insured at the moment, who needs products and can’t afford it – and you figure out a way to help”, Adriana says. For registered youth under 21 years of age, the costs of the healthcare provision are covered by the national health insurance, however, some students fall outside of the system. “For our second, third and fourth-year students, FPA has been collaborating with us to provide a monthly session where the students receive contraceptives and guidance on school grounds. Since around this age, most of our students are already sexually active, we try to help them stay safe in and out of school.” “The love, patience, and dedication that FPA has shown our students over the years are outstanding. At the beginning of the COVID-19 crisis we had to stop the consultation hours, but thankfully we are now back at it, bigger and better. Due to the collaboration with FPA we were able to finish out our 2018-2019 school year with no new pregnancies, which was a first for our school. We hope to accomplish this again, now that we can continue our consultations, and keep our kids educated and in school for as long as we can so they can achieve the best possible future”, Adriana says.

| 24 April 2024
Providing information and contraceptive care to young people in school
Accessibility to information and contraceptives has always been a priority for Famia Planea Aruba (FPA) – whether through the office, delivery service, or in schools. For over 15 years FPA has worked in partnership with one of the largest secondary schools on the island. The FPA team visits the school every month to provide guidance, counselling, and contraceptive care to students, and to help ensure they stay in school to complete their education. “One of my first experiences providing comprehensive sex education with FPA was at the EPB School, during my education as a social worker. Many years later I still very much enjoy this”, says Richenella, FPA’s Finance and Information, Education and Communication (IEC) support staff. Building trust FPA’s client is at the heart of its healthcare provision. The FPA team works with students to build trust and ensure they feel safe to talk openly. This helps to provide a sense of consistency for the student, as well as efficiency for the team being familiar with specific students and cases. They are better able to notice if something changes, and if a student needs a referral to a medical doctor or other organization for additional treatment. “The consultations are always fun; you get a change of scenery by stepping out of the office. Over the years you see so many faces and still somehow you manage to remember most of them. After just a few visits you can start to build a profile of most students; you can start to tell who the class clown is, the Mister Popular, the shy one, the loud one, and the one who just wants to take his time to avoid going back to class”, Richenella laughs. Working in partnership with the school social worker FPA places great value on the 14-year relationship they have with Adriana, the social worker at EPB San Nicolas School. Adriana is the person who has the most contact with the students, and the one most student’s turn to when they need help. “Most of the time you get to have fun with the students, however every now and then you will come across a heartbreaking case. Since Aruba has so many different migrants, very often you will come across one person who is not insured at the moment, who needs products and can’t afford it – and you figure out a way to help”, Adriana says. For registered youth under 21 years of age, the costs of the healthcare provision are covered by the national health insurance, however, some students fall outside of the system. “For our second, third and fourth-year students, FPA has been collaborating with us to provide a monthly session where the students receive contraceptives and guidance on school grounds. Since around this age, most of our students are already sexually active, we try to help them stay safe in and out of school.” “The love, patience, and dedication that FPA has shown our students over the years are outstanding. At the beginning of the COVID-19 crisis we had to stop the consultation hours, but thankfully we are now back at it, bigger and better. Due to the collaboration with FPA we were able to finish out our 2018-2019 school year with no new pregnancies, which was a first for our school. We hope to accomplish this again, now that we can continue our consultations, and keep our kids educated and in school for as long as we can so they can achieve the best possible future”, Adriana says.