Spotlight
A selection of stories from across the Federation

France, Germany, Poland, United Kingdom, United States, Colombia, India, Tunisia
Abortion Rights: Latest Decisions and Developments around the World
The global landscape of abortion rights continues to evolve in 2024, with new legislation and feminist movements fighting for better access. Let's take a trip around the world to see the latest developments.
Most Popular This Week
France, Germany, Poland, United Kingdom, United States, Colombia, India, Tunisia

Abortion Rights: Latest Decisions and Developments around the World
Over the past 30 years, more than

Palestine

In their own words: The people providing sexual and reproductive health care under bombardment in Gaza
Week after week, heavy Israeli bombardment from air, land, and sea, has continued across most of the Gaza Strip.
Vanuatu

When getting to the hospital is difficult, Vanuatu mobile outreach can save lives
In the mountains of Kumera on Tanna Island, Vanuatu, the village women of Kamahaul normally spend over 10,000 Vatu ($83 USD) to travel to the nearest hospital.
Vanuatu

Sex: changing minds and winning hearts in Tanna, Vanuatu
“Very traditional.” These two words are often used to describe the people of Tanna in Vanuatu, one of the most populated islands in the small country in the Pacific.
Vanuatu

Vanuatu cyclone response: The mental health toll on humanitarian providers
Girls and women from nearby villages flock to mobile health clinics set up by the Vanuatu Family Health Association (VFHA).
Cook Islands

Trans & Proud: Being Transgender in the Cook Islands
It’s a scene like many others around the world: a loving family pour over childhood photos, giggling and reminiscing about the memories.
Cook Islands

In Pictures: The activists who helped win LGBTI+ rights in the Cook Islands
The Cook Islands has removed a law that criminalizes homosexuality, in a huge victory for the local LGBTI+ community.
Filter our stories by:
- Association Burundaise pour le Bien-Etre Familial
- Association Malienne pour la Protection et la Promotion de la Famille
- Association Togolaise pour le Bien-Etre Familial
- Cameroon National Association for Family Welfare
- Family Guidance Association of Ethiopia
- Family Planning Association of Malawi
- Family Planning Association of Nepal
- Family Planning Association of Sri Lanka
- Foundation for the Promotion of Responsible Parenthood - Aruba
- Indonesian Planned Parenthood Association
- Kiribati Family Health Association
- Palestinian Family Planning and Protection Association (PFPPA)
- Planned Parenthood Association of Ghana
- Reproductive & Family Health Association of Fiji
- Reproductive Health Association of Cambodia (RHAC)
- Reproductive Health Uganda
- Somaliland Family Health Association
- Tonga Family Health Association
- Vanuatu Family Health Association


| 08 January 2021
"Girls have to know their rights"
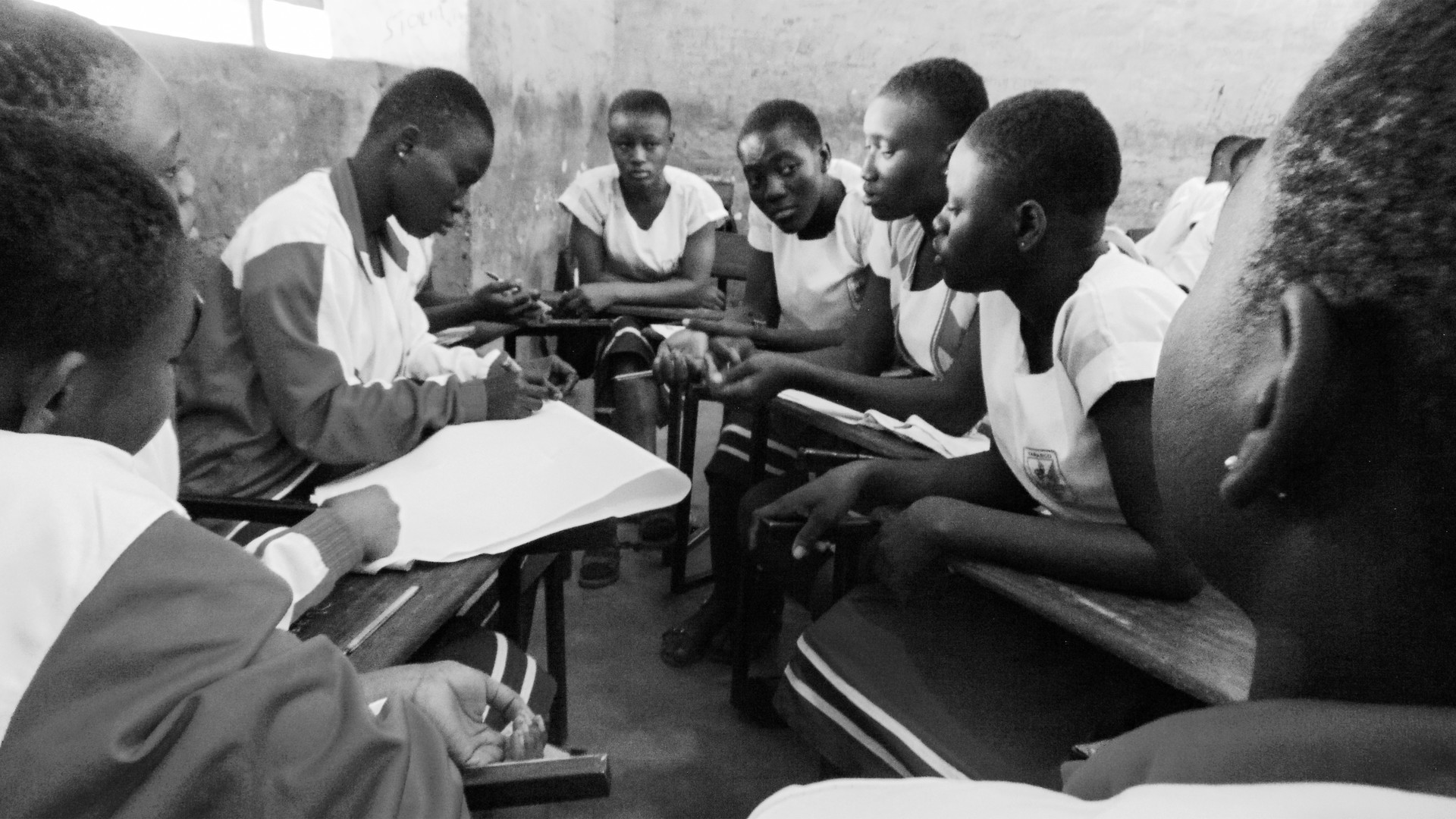
Aminata Sonogo listened intently to the group of young volunteers as they explained different types of contraception, and raised her hand with questions. Sitting at a wooden school desk at 22, Aminata is older than most of her classmates, but she shrugs off the looks and comments. She has fought hard to be here. Aminata is studying in Bamako, the capital of Mali. Just a quarter of Malian girls complete secondary school, according to UNICEF. But even if she will graduate later than most, Aminata is conscious of how far she has come. “I wanted to go to high school but I needed to pass some exams to get here. In the end, it took me three years,” she said. At the start of her final year of collège, or middle school, Aminata got pregnant. She is far from alone: 38% of Malian girls will be pregnant or a mother by the age of 18. Abortion is illegal in Mali except in cases of rape, incest or danger to the mother’s life, and even then it is difficult to obtain, according to medical professionals. Determined to take control of her life “I felt a lot of stigma from my classmates and even my teachers. I tried to ignore them and carry on going to school and studying. But I gave birth to my daughter just before my exams, so I couldn’t take them.” Aminata went through her pregnancy with little support, as the father of her daughter, Fatoumata, distanced himself from her after arguments about their situation. “I have had some problems with the father of the baby. We fought a lot and I didn’t see him for most of the pregnancy, right until the birth,” she recalled. The first year of her daughter’s life was a blur of doctors’ appointments, as Fatoumata was often ill. It seemed Aminata’s chances of finishing school were slipping away. But gradually her family began to take a more active role in caring for her daughter, and she began demanding more help from Fatoumata’s father too. She went back to school in the autumn, 18 months after Fatoumata’s birth and with more determination than ever. She no longer had time to hang out with friends after school, but attended classes, took care of her daughter and then studied more. At the end of the academic year, it paid off. “I did it. I passed my exams and now I am in high school,” Aminata said, smiling and relaxing her shoulders. "Family planning protects girls" Aminata’s next goal is her high school diploma, and obtaining it while trying to navigate the difficult world of relationships and sex. “It’s something you can talk about with your close friends. I would be too ashamed to talk about this with my parents,” she said. She is guided by visits from the young volunteers of the Association Malienne pour la Protection et Promotion de la Famille (AMPPF), and shares her own story with classmates who she sees at risk. “The guys come up to you and tell you that you are beautiful, but if you don’t want to sleep with them they will rape you. That’s the choice. You can accept or you can refuse and they will rape you anyway,” she said. “Girls have to know their rights”. After listening to the volunteers talk about all the different options for contraception, she is reviewing her own choices. “Family planning protects girls,” Aminata said. “It means we can protect ourselves from pregnancies that we don’t want”.

| 18 April 2024
"Girls have to know their rights"
Aminata Sonogo listened intently to the group of young volunteers as they explained different types of contraception, and raised her hand with questions. Sitting at a wooden school desk at 22, Aminata is older than most of her classmates, but she shrugs off the looks and comments. She has fought hard to be here. Aminata is studying in Bamako, the capital of Mali. Just a quarter of Malian girls complete secondary school, according to UNICEF. But even if she will graduate later than most, Aminata is conscious of how far she has come. “I wanted to go to high school but I needed to pass some exams to get here. In the end, it took me three years,” she said. At the start of her final year of collège, or middle school, Aminata got pregnant. She is far from alone: 38% of Malian girls will be pregnant or a mother by the age of 18. Abortion is illegal in Mali except in cases of rape, incest or danger to the mother’s life, and even then it is difficult to obtain, according to medical professionals. Determined to take control of her life “I felt a lot of stigma from my classmates and even my teachers. I tried to ignore them and carry on going to school and studying. But I gave birth to my daughter just before my exams, so I couldn’t take them.” Aminata went through her pregnancy with little support, as the father of her daughter, Fatoumata, distanced himself from her after arguments about their situation. “I have had some problems with the father of the baby. We fought a lot and I didn’t see him for most of the pregnancy, right until the birth,” she recalled. The first year of her daughter’s life was a blur of doctors’ appointments, as Fatoumata was often ill. It seemed Aminata’s chances of finishing school were slipping away. But gradually her family began to take a more active role in caring for her daughter, and she began demanding more help from Fatoumata’s father too. She went back to school in the autumn, 18 months after Fatoumata’s birth and with more determination than ever. She no longer had time to hang out with friends after school, but attended classes, took care of her daughter and then studied more. At the end of the academic year, it paid off. “I did it. I passed my exams and now I am in high school,” Aminata said, smiling and relaxing her shoulders. "Family planning protects girls" Aminata’s next goal is her high school diploma, and obtaining it while trying to navigate the difficult world of relationships and sex. “It’s something you can talk about with your close friends. I would be too ashamed to talk about this with my parents,” she said. She is guided by visits from the young volunteers of the Association Malienne pour la Protection et Promotion de la Famille (AMPPF), and shares her own story with classmates who she sees at risk. “The guys come up to you and tell you that you are beautiful, but if you don’t want to sleep with them they will rape you. That’s the choice. You can accept or you can refuse and they will rape you anyway,” she said. “Girls have to know their rights”. After listening to the volunteers talk about all the different options for contraception, she is reviewing her own choices. “Family planning protects girls,” Aminata said. “It means we can protect ourselves from pregnancies that we don’t want”.

| 08 January 2021
"The movement helps girls to know their rights and their bodies"
My name is Fatoumata Yehiya Maiga. I’m 23-years-old, and I’m an IT specialist. I joined the Youth Action Movement at the end of 2018. The head of the movement in Mali is a friend of mine, and I met her before I knew she was the president. She invited me to their events and over time persuaded me to join. I watched them raising awareness about sexual and reproductive health, using sketches and speeches. I learnt a lot. Overcoming taboos I went home and talked about what I had seen and learnt with my family. In Africa, and even more so in the village where I come from in Gao, northern Mali, people don’t talk about these things. I wanted to take my sisters to the events, but every time I spoke about them my relatives would just say it was to teach girls to have sex, and that it’s taboo. That’s not what I believe. I think the movement helps girls, most of all, to know their sexual rights, their bodies, what to do and what not to do to stay healthy and safe. They don’t understand this concept. My family would say it was just a smokescreen to convince girls to get involved in something dirty. I have had to tell my younger cousins about their periods, for example, when they came from the village to live in the city. One of my cousins was so scared, and told me she was bleeding from her vagina and didn’t know why. We talk about managing periods in the Youth Action Movement, as well as how to manage cramps and feel better. The devastating impact of FGM But there was a much more important reason for me to join the movement. My parents are educated, so me and my sisters were never cut. I learned about female genital mutilation at a conference I attended in 2016. I didn’t know that there were different types of severity and ways that girls could be cut. I hadn’t understood quite how dangerous this practice is. Then, two years ago, I lost my friend Aïssata. She got married young, at 17. She struggled to conceive until she was 23. The day she gave birth, there were complications and she died. The doctors said that the excision was botched and that’s what killed her. From that day on, I decided I needed to teach all the girls in my community about how harmful this practice is for their health. I was so horrified by the way she died. Normally, girls in Mali are cut when they are three or four years old, though for some it’s done at birth. When they are older and get pregnant, I know they face the same challenges as every woman does giving birth, but they also live with the dangerous consequences of this unhealthy practice. The importance of talking openly The problem lies with the families. I want us, as a movement, to talk with the parents and explain to them how they can contribute to their children’s sexual health. I wish it were no longer a taboo between parents and their girls. But if we talk in such direct terms, they only see disobedience, and say that we are encouraging promiscuity. We need to talk to teenagers because they are already parents in many cases. They are the ones who decide to go through with cutting their daughters, or not. A lot of Mali is hard to reach though. We need travelling groups to go to those isolated rural areas and talk to people about sexual health. Pregnancy is the girl’s decision, and girls have a right to be healthy, and to choose their future.

| 18 April 2024
"The movement helps girls to know their rights and their bodies"
My name is Fatoumata Yehiya Maiga. I’m 23-years-old, and I’m an IT specialist. I joined the Youth Action Movement at the end of 2018. The head of the movement in Mali is a friend of mine, and I met her before I knew she was the president. She invited me to their events and over time persuaded me to join. I watched them raising awareness about sexual and reproductive health, using sketches and speeches. I learnt a lot. Overcoming taboos I went home and talked about what I had seen and learnt with my family. In Africa, and even more so in the village where I come from in Gao, northern Mali, people don’t talk about these things. I wanted to take my sisters to the events, but every time I spoke about them my relatives would just say it was to teach girls to have sex, and that it’s taboo. That’s not what I believe. I think the movement helps girls, most of all, to know their sexual rights, their bodies, what to do and what not to do to stay healthy and safe. They don’t understand this concept. My family would say it was just a smokescreen to convince girls to get involved in something dirty. I have had to tell my younger cousins about their periods, for example, when they came from the village to live in the city. One of my cousins was so scared, and told me she was bleeding from her vagina and didn’t know why. We talk about managing periods in the Youth Action Movement, as well as how to manage cramps and feel better. The devastating impact of FGM But there was a much more important reason for me to join the movement. My parents are educated, so me and my sisters were never cut. I learned about female genital mutilation at a conference I attended in 2016. I didn’t know that there were different types of severity and ways that girls could be cut. I hadn’t understood quite how dangerous this practice is. Then, two years ago, I lost my friend Aïssata. She got married young, at 17. She struggled to conceive until she was 23. The day she gave birth, there were complications and she died. The doctors said that the excision was botched and that’s what killed her. From that day on, I decided I needed to teach all the girls in my community about how harmful this practice is for their health. I was so horrified by the way she died. Normally, girls in Mali are cut when they are three or four years old, though for some it’s done at birth. When they are older and get pregnant, I know they face the same challenges as every woman does giving birth, but they also live with the dangerous consequences of this unhealthy practice. The importance of talking openly The problem lies with the families. I want us, as a movement, to talk with the parents and explain to them how they can contribute to their children’s sexual health. I wish it were no longer a taboo between parents and their girls. But if we talk in such direct terms, they only see disobedience, and say that we are encouraging promiscuity. We need to talk to teenagers because they are already parents in many cases. They are the ones who decide to go through with cutting their daughters, or not. A lot of Mali is hard to reach though. We need travelling groups to go to those isolated rural areas and talk to people about sexual health. Pregnancy is the girl’s decision, and girls have a right to be healthy, and to choose their future.

| 13 August 2020
In pictures: Delivering healthcare to remote communities in Fiji
In early April 2020, the all too familiar destruction of a Tropical Cyclone (TC) – Harold – hit the Solomon Islands, Vanuatu, Fiji and Tonga. One of the worst affected areas was the Eastern part of Fiji. Through support by Department of Foreign Affairs and Trade (DFAT), our Member Association, Reproductive and Family Health Association of Fiji (RFHAF), was quick to respond ensuring access to essential sexual and reproductive healthcare for Kadavu’s women, girls, and vulnerable groups. Fiji's vulnerable coastline Fiji’s worst affected area was the Eastern part, with TC Harold bringing destructive storm force winds and storm surge. RFHAF focused its humanitarian response on the local Kadavu population. This remote area proves a challenge to reach for the team with supplies. Share on Twitter Share on Facebook Share via WhatsApp Share via Email RFHAF's humanitarian response team tackle rough terrain National travel restrictions - due to the current COVID-19 pandemic - on all inter island transfers has slowed the response in some areas, including Kadavu. The island of Kadavu is one of the least developed areas of Fiji, the main source of income is substance living (Yaqona). Transport around the island is difficult, with very few roads, no public water system or electricity. The humanitarian team from RFHAF travels by boat and then on foot. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Asenaca, client Kadavu, the biggest island in the Eastern division has the greatest population (10,897). 197 evacuation centres were activated in total, initially hosting over 6,240 people. Many are women of reproductive age, with an estimated 150 currently pregnant. Asenaca learns about breast cancer self-checks from RFHAF’s healthcare provider, Karo. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nasi, RFHAF healthcare provider The medical mobile team deliver a broad range of healthcare including contraception, information and counselling on sexual health, pregnancy, HIV and STI care and testing. RFHAF Team in Kadavu performing general health checks after TC Harold. Nasi administers a HPV shot to a client. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Kate, client Young women and girls are at the heart of RFHAF’s healthcare provision. Kate walks home with her dignity kit after a health check at the mobile clinic. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Karo, RFHAF healthcare worker RFHAF offers sexual and reproductive healthcare as well as counselling, and referrals for follow up care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Alidi, RFHAF healthcare worker The team ensures young people in the community are not forgotten and provide information and education on relationships and sexual health and rights. Alidi conducting a session with a local group of young people at Gasele, Kadavu.Photos ©IPPF/Rob Rickman/Fiji Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 18 April 2024
In pictures: Delivering healthcare to remote communities in Fiji
In early April 2020, the all too familiar destruction of a Tropical Cyclone (TC) – Harold – hit the Solomon Islands, Vanuatu, Fiji and Tonga. One of the worst affected areas was the Eastern part of Fiji. Through support by Department of Foreign Affairs and Trade (DFAT), our Member Association, Reproductive and Family Health Association of Fiji (RFHAF), was quick to respond ensuring access to essential sexual and reproductive healthcare for Kadavu’s women, girls, and vulnerable groups. Fiji's vulnerable coastline Fiji’s worst affected area was the Eastern part, with TC Harold bringing destructive storm force winds and storm surge. RFHAF focused its humanitarian response on the local Kadavu population. This remote area proves a challenge to reach for the team with supplies. Share on Twitter Share on Facebook Share via WhatsApp Share via Email RFHAF's humanitarian response team tackle rough terrain National travel restrictions - due to the current COVID-19 pandemic - on all inter island transfers has slowed the response in some areas, including Kadavu. The island of Kadavu is one of the least developed areas of Fiji, the main source of income is substance living (Yaqona). Transport around the island is difficult, with very few roads, no public water system or electricity. The humanitarian team from RFHAF travels by boat and then on foot. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Asenaca, client Kadavu, the biggest island in the Eastern division has the greatest population (10,897). 197 evacuation centres were activated in total, initially hosting over 6,240 people. Many are women of reproductive age, with an estimated 150 currently pregnant. Asenaca learns about breast cancer self-checks from RFHAF’s healthcare provider, Karo. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nasi, RFHAF healthcare provider The medical mobile team deliver a broad range of healthcare including contraception, information and counselling on sexual health, pregnancy, HIV and STI care and testing. RFHAF Team in Kadavu performing general health checks after TC Harold. Nasi administers a HPV shot to a client. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Kate, client Young women and girls are at the heart of RFHAF’s healthcare provision. Kate walks home with her dignity kit after a health check at the mobile clinic. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Karo, RFHAF healthcare worker RFHAF offers sexual and reproductive healthcare as well as counselling, and referrals for follow up care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Alidi, RFHAF healthcare worker The team ensures young people in the community are not forgotten and provide information and education on relationships and sexual health and rights. Alidi conducting a session with a local group of young people at Gasele, Kadavu.Photos ©IPPF/Rob Rickman/Fiji Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 28 July 2020
"I wanted to protect girls from violence – like early marriage – and I wanted to change people’s wrong perceptions about sex and sexuality"
Seventeen-year-old student Jumeya Mohammed Amin started educating other people about sexual and reproductive health when she was 14 years old. She trained as a ‘change agent’ for her community through the Family Guidance Association of Ethiopia’s south west office in Jimma, the capital of Oromia region. Amin comes from a small, conservative town about 20km outside the city. "I wanted to protect girls from violence – like early marriage – and I wanted to change people’s wrong perceptions about sex and sexuality, because they [men in her community] start having sex with girls at a young age, even with girls as young as nine years old, because of a lack of education." "They suddenly had to act like grown-up women" "Before I started this training I saw the majority of students having sex early and getting pregnant because of a lack of information, and they would have to leave home and school. Boys would be disciplined and if they were seen doing things on campus, expelled. Girls younger than me at the time were married. The youngest was only nine. They would have to go back home and could not play anymore or go to school. They suddenly had to act like grown-up women, like old ladies. They never go back to school after marriage. My teacher chose me for this training and told me about the programme. I like the truth so I was not afraid. I heard about a lot of problems out there during my training and I told myself I had to be strong and go and fight this." "I have a brother and four sisters and I practiced my training on my family first. They were so shocked by what I was saying they were silent. Even on the second day, they said nothing. On the third day, I told them I was going to teach people in schools this, so I asked them why they had stayed silent. They told me that because of cultural and religious issues, people would not accept these ideas and stories, but they gave me permission to go and do it. Because of my efforts, people in my school have not started having sex early and the girls get free sanitary pads through the clubs so they no longer need to stay home during periods." Training hundreds of her peers "I know people in my community who have unplanned pregnancies consult traditional healers [for abortions] and take drugs and they suffer. I know one girl from 10th grade who was 15 years old and died from this in 2017. The healers sometimes use tree leaves in their concoctions. We tell them where they can go and get different [safe abortion] services. The first round of trainings I did was with 400 students over four months and eight sessions in 2017. Last year, I trained 600 people and this year in the first trimester of school I trained 400. When students finish the course, they want to do it again, and when we forget we have a session, they come and remind me. At school, they call me a teacher. I’d like to be a doctor and this training has really made me want to do that more."

| 18 April 2024
"I wanted to protect girls from violence – like early marriage – and I wanted to change people’s wrong perceptions about sex and sexuality"
Seventeen-year-old student Jumeya Mohammed Amin started educating other people about sexual and reproductive health when she was 14 years old. She trained as a ‘change agent’ for her community through the Family Guidance Association of Ethiopia’s south west office in Jimma, the capital of Oromia region. Amin comes from a small, conservative town about 20km outside the city. "I wanted to protect girls from violence – like early marriage – and I wanted to change people’s wrong perceptions about sex and sexuality, because they [men in her community] start having sex with girls at a young age, even with girls as young as nine years old, because of a lack of education." "They suddenly had to act like grown-up women" "Before I started this training I saw the majority of students having sex early and getting pregnant because of a lack of information, and they would have to leave home and school. Boys would be disciplined and if they were seen doing things on campus, expelled. Girls younger than me at the time were married. The youngest was only nine. They would have to go back home and could not play anymore or go to school. They suddenly had to act like grown-up women, like old ladies. They never go back to school after marriage. My teacher chose me for this training and told me about the programme. I like the truth so I was not afraid. I heard about a lot of problems out there during my training and I told myself I had to be strong and go and fight this." "I have a brother and four sisters and I practiced my training on my family first. They were so shocked by what I was saying they were silent. Even on the second day, they said nothing. On the third day, I told them I was going to teach people in schools this, so I asked them why they had stayed silent. They told me that because of cultural and religious issues, people would not accept these ideas and stories, but they gave me permission to go and do it. Because of my efforts, people in my school have not started having sex early and the girls get free sanitary pads through the clubs so they no longer need to stay home during periods." Training hundreds of her peers "I know people in my community who have unplanned pregnancies consult traditional healers [for abortions] and take drugs and they suffer. I know one girl from 10th grade who was 15 years old and died from this in 2017. The healers sometimes use tree leaves in their concoctions. We tell them where they can go and get different [safe abortion] services. The first round of trainings I did was with 400 students over four months and eight sessions in 2017. Last year, I trained 600 people and this year in the first trimester of school I trained 400. When students finish the course, they want to do it again, and when we forget we have a session, they come and remind me. At school, they call me a teacher. I’d like to be a doctor and this training has really made me want to do that more."

| 16 July 2020
"Before, there was no safe abortion"
Rewda Kedir works as a midwife in a rural area of the Oromia region in southwest Ethiopia. Only 14% of married women are using any method of contraception here. The government hospital Rewda works in is supported to provide a full range of sexual and reproductive healthcare, which includes providing free contraceptives and comprehensive abortion care. In January 2017, the maternal healthcare clinic faced shortages of contraceptives after the US administration reactivated and expanded the Global Gag Rule, which does not allow any funding to go to organizations associated with providing abortion care. Fortunately in this case, the shortages only lasted a month due to the government of the Netherlands stepping in and matching lost funding. “Before, we had a shortage of contraceptive pills and emergency contraceptives. We would have to give people prescriptions and they would go to private clinics and where they had to pay," Rewda tells us. "When I first came to this clinic, there was a real shortage of people trained in family planning. I was the only one. Now there are many people trained on family planning, and when I’m not here, people can help." "There used to be a shortage of choice and alternatives, and now there are many. And the implant procedures are better because there are newer products that are much smaller so putting them in is less invasive.” Opening a dialogue on contraception The hospital has been providing medical abortions for six years. “Before, there was no safe abortion," says Rewda. She explains how people would go to 'traditional' healers and then come to the clinic with complications like sepsis, bleeding, anaemia and toxic shock. If they had complications or infections above nine weeks, Rewda and her colleagues would send them to Jimma, the regional capital. "Before, it was very difficult to persuade them to use family planning, and we had to have a lot of conversations. Now, they come 45 days after delivery to speak to us about this and get their babies immunised," she explains. "They want contraceptives to space out their children. Sometimes their husbands don’t like them coming to get family planning so we have to lock their appointment cards away. Their husbands want more children and they think that women who do not keep having their children will go with other men." "More kids, more wealth" Rewda tells us that they've used family counselling to try and persuade men to reconsider their ideas about contraception, by explaining to them that continuously giving birth under unsafe circumstances can affect a woman's health and might lead to maternal death, damage the uterus and lead to long-term complications. "Here, people believe that more kids means more wealth, and religion restricts family planning services. Before, they did not have good training on family planning and abortion. Now, women that have abortions get proper care and the counseling and education has improved. There are still unsafe abortions but they have really reduced. We used to see about 40 a year and now it’s one or two." However, problems still exist. "There are some complications, like irregular bleeding from some contraceptives," Rewda says, and that "women still face conflict with their husbands over family planning and sometimes have to go to court to fight this or divorce them.”

| 18 April 2024
"Before, there was no safe abortion"
Rewda Kedir works as a midwife in a rural area of the Oromia region in southwest Ethiopia. Only 14% of married women are using any method of contraception here. The government hospital Rewda works in is supported to provide a full range of sexual and reproductive healthcare, which includes providing free contraceptives and comprehensive abortion care. In January 2017, the maternal healthcare clinic faced shortages of contraceptives after the US administration reactivated and expanded the Global Gag Rule, which does not allow any funding to go to organizations associated with providing abortion care. Fortunately in this case, the shortages only lasted a month due to the government of the Netherlands stepping in and matching lost funding. “Before, we had a shortage of contraceptive pills and emergency contraceptives. We would have to give people prescriptions and they would go to private clinics and where they had to pay," Rewda tells us. "When I first came to this clinic, there was a real shortage of people trained in family planning. I was the only one. Now there are many people trained on family planning, and when I’m not here, people can help." "There used to be a shortage of choice and alternatives, and now there are many. And the implant procedures are better because there are newer products that are much smaller so putting them in is less invasive.” Opening a dialogue on contraception The hospital has been providing medical abortions for six years. “Before, there was no safe abortion," says Rewda. She explains how people would go to 'traditional' healers and then come to the clinic with complications like sepsis, bleeding, anaemia and toxic shock. If they had complications or infections above nine weeks, Rewda and her colleagues would send them to Jimma, the regional capital. "Before, it was very difficult to persuade them to use family planning, and we had to have a lot of conversations. Now, they come 45 days after delivery to speak to us about this and get their babies immunised," she explains. "They want contraceptives to space out their children. Sometimes their husbands don’t like them coming to get family planning so we have to lock their appointment cards away. Their husbands want more children and they think that women who do not keep having their children will go with other men." "More kids, more wealth" Rewda tells us that they've used family counselling to try and persuade men to reconsider their ideas about contraception, by explaining to them that continuously giving birth under unsafe circumstances can affect a woman's health and might lead to maternal death, damage the uterus and lead to long-term complications. "Here, people believe that more kids means more wealth, and religion restricts family planning services. Before, they did not have good training on family planning and abortion. Now, women that have abortions get proper care and the counseling and education has improved. There are still unsafe abortions but they have really reduced. We used to see about 40 a year and now it’s one or two." However, problems still exist. "There are some complications, like irregular bleeding from some contraceptives," Rewda says, and that "women still face conflict with their husbands over family planning and sometimes have to go to court to fight this or divorce them.”

| 18 June 2020
In pictures: Healthcare in the face of the climate crisis in Kiribati
Humanitarian crises Largely brought on by sudden onset and slow-onset natural disasters, humanitarian crises are increasingly prevalent in the Pacific. During responses to humanitarian crises in the Pacific, sexual and reproductive healthcare is often under-prioritised and under-resourced. As a result, women and girls of reproductive age and vulnerable and marginalized groups are disproportionately affected and facing increased health and psychosocial risks. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Fragile environments Low topography, rising sea levels and insufficient fresh water supply leaves Kiribati’s population vulnerable to the effects of the climate crisis. The fragility of the outer islands of Kiribati during natural disasters is compounded by their geographic isolation, which makes transportation and communication during post-disaster relief and response both expensive and difficult. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Coastal exposure The majority of the population of 115,000 people live a subsistence lifestyle. Communities are geographically dispersed across 33 atolls covering 3.5 million square kilometres in the central Pacific Ocean. The population and infrastructure within Kiribati are largely concentrated on the coast, where communities face increased exposure to climate threats and natural hazards such as tsunamis, earthquakes, king tides, flooding, droughts, and occasionally cyclones. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Takaria, leader and youth organizer in the Tebikenikua community Takaria will be running to be a Member of Parliament in Kiribati in 2020. “I assist the youth with family problems and family planning and disasters. In our community there are unforeseen pregnancies, domestic violence, and disasters such as high tide waters and strong winds, which can also affect this community. The Kiribati Family Health Association (KFHA) is the key point for us with outreach and training so people in this community know how to prevent and treat STIs, etc. They all know where the KFHA clinic is and that they can get counselling or services there. The problem now is you can’t survive with the sea rise levels. I want all members of my community to live better and have better health and peace.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Susan*, sex worker Susan receives care at the Kiribati Family Health Association (KFHA) including a pap smear. Susan*, 28, is a sex worker from the town of Betio on the main island of Kiribati. Originally from an outlying island, she moved into Tarawa to seek work. Unable to find employment that would fulfill her dream of sending money back to her two children, she was introduced to sex work. With other sex workers, she regularly travels out to the large cargo ships from China, Philippines and Korea anchored off the coast of Kiribati. Despite her new income, she still can’t speak with her children or see them due to the restrictive costs involved of travel between islands.*pseudonym Share on Twitter Share on Facebook Share via WhatsApp Share via Email Theta, 25-year-old mother and youth volunteer Theta is part of the Humanitarian Youth Club set up by the Kiribati Family Health Association in her village. “We face a lot of situations here, one of them is disasters and the second is unemployment and school drop out with our youth. I have helped the Humanitarian Youth Club to apply for financial grants from the Australian High Commission [for $1,000] I am recognized as the smartest member who can write in English. We have learned how to design a disaster plan for the community and share our ideas on sexual and reproductive issues such as STIs. We discuss what we can do for the next strong tide, where we can gather as a community and what we can do if even the maneabe (town hall) floods? If the tide and wind is too strong, we need to go to another safer place, such as another community’s town hall. For now, I want to enjoy the chance to be in our own beloved country. I won’t move until the majority have already left. I want my daughter to grow up in the same place I grew up in.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Beitau, youth volunteer Beitau is the Chairperson of the Humanitarian Youth Club. “I was lucky to be selected as Chairperson as the Humanitarian Youth Club. I feel like I get more respect from the community now I am in this position. I would love advanced training on leadership now, to further assist the club. As I am the Chairperson of the HYC, my main target is to help people during a disaster. I have attended training through KFHA. What I took from this is that when a disaster strikes, we have to do our best for pregnant women, small children and people with disabilities. They more vulnerable and less able to survive a disaster.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Abe, youth officer Abe was involved with KFHA since 2012. “I was inspired by what they KFHA was doing and the issues they were addressing that affects youth. I was surprised to see how many young people come to the clinic as they are affected by STIs, HIV and teenage pregnancy. The lack of education here is a big problem, most people here have a lot of children and yet can’t afford to send them to school. Sexual and reproductive health is our responsibility and we must talk about it with young people. Climate change affects many countries, but Kiribati is small and low lying. I used to go visit a very nice beach with a lot of nice trees and plants. Now, the trees are gone, and the waves have taken over, and the houses have disappeared so no one can build there. In my role as a youth worker and activist, I tell people to fight climate change: to grow more mangroves, to clean up the beach, because we love our Kiribati.”©IPPF/Hannah Maule-Ffinch/Kiribati Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 18 April 2024
In pictures: Healthcare in the face of the climate crisis in Kiribati
Humanitarian crises Largely brought on by sudden onset and slow-onset natural disasters, humanitarian crises are increasingly prevalent in the Pacific. During responses to humanitarian crises in the Pacific, sexual and reproductive healthcare is often under-prioritised and under-resourced. As a result, women and girls of reproductive age and vulnerable and marginalized groups are disproportionately affected and facing increased health and psychosocial risks. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Fragile environments Low topography, rising sea levels and insufficient fresh water supply leaves Kiribati’s population vulnerable to the effects of the climate crisis. The fragility of the outer islands of Kiribati during natural disasters is compounded by their geographic isolation, which makes transportation and communication during post-disaster relief and response both expensive and difficult. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Coastal exposure The majority of the population of 115,000 people live a subsistence lifestyle. Communities are geographically dispersed across 33 atolls covering 3.5 million square kilometres in the central Pacific Ocean. The population and infrastructure within Kiribati are largely concentrated on the coast, where communities face increased exposure to climate threats and natural hazards such as tsunamis, earthquakes, king tides, flooding, droughts, and occasionally cyclones. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Takaria, leader and youth organizer in the Tebikenikua community Takaria will be running to be a Member of Parliament in Kiribati in 2020. “I assist the youth with family problems and family planning and disasters. In our community there are unforeseen pregnancies, domestic violence, and disasters such as high tide waters and strong winds, which can also affect this community. The Kiribati Family Health Association (KFHA) is the key point for us with outreach and training so people in this community know how to prevent and treat STIs, etc. They all know where the KFHA clinic is and that they can get counselling or services there. The problem now is you can’t survive with the sea rise levels. I want all members of my community to live better and have better health and peace.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Susan*, sex worker Susan receives care at the Kiribati Family Health Association (KFHA) including a pap smear. Susan*, 28, is a sex worker from the town of Betio on the main island of Kiribati. Originally from an outlying island, she moved into Tarawa to seek work. Unable to find employment that would fulfill her dream of sending money back to her two children, she was introduced to sex work. With other sex workers, she regularly travels out to the large cargo ships from China, Philippines and Korea anchored off the coast of Kiribati. Despite her new income, she still can’t speak with her children or see them due to the restrictive costs involved of travel between islands.*pseudonym Share on Twitter Share on Facebook Share via WhatsApp Share via Email Theta, 25-year-old mother and youth volunteer Theta is part of the Humanitarian Youth Club set up by the Kiribati Family Health Association in her village. “We face a lot of situations here, one of them is disasters and the second is unemployment and school drop out with our youth. I have helped the Humanitarian Youth Club to apply for financial grants from the Australian High Commission [for $1,000] I am recognized as the smartest member who can write in English. We have learned how to design a disaster plan for the community and share our ideas on sexual and reproductive issues such as STIs. We discuss what we can do for the next strong tide, where we can gather as a community and what we can do if even the maneabe (town hall) floods? If the tide and wind is too strong, we need to go to another safer place, such as another community’s town hall. For now, I want to enjoy the chance to be in our own beloved country. I won’t move until the majority have already left. I want my daughter to grow up in the same place I grew up in.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Beitau, youth volunteer Beitau is the Chairperson of the Humanitarian Youth Club. “I was lucky to be selected as Chairperson as the Humanitarian Youth Club. I feel like I get more respect from the community now I am in this position. I would love advanced training on leadership now, to further assist the club. As I am the Chairperson of the HYC, my main target is to help people during a disaster. I have attended training through KFHA. What I took from this is that when a disaster strikes, we have to do our best for pregnant women, small children and people with disabilities. They more vulnerable and less able to survive a disaster.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Abe, youth officer Abe was involved with KFHA since 2012. “I was inspired by what they KFHA was doing and the issues they were addressing that affects youth. I was surprised to see how many young people come to the clinic as they are affected by STIs, HIV and teenage pregnancy. The lack of education here is a big problem, most people here have a lot of children and yet can’t afford to send them to school. Sexual and reproductive health is our responsibility and we must talk about it with young people. Climate change affects many countries, but Kiribati is small and low lying. I used to go visit a very nice beach with a lot of nice trees and plants. Now, the trees are gone, and the waves have taken over, and the houses have disappeared so no one can build there. In my role as a youth worker and activist, I tell people to fight climate change: to grow more mangroves, to clean up the beach, because we love our Kiribati.”©IPPF/Hannah Maule-Ffinch/Kiribati Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 08 January 2021
"Girls have to know their rights"
Aminata Sonogo listened intently to the group of young volunteers as they explained different types of contraception, and raised her hand with questions. Sitting at a wooden school desk at 22, Aminata is older than most of her classmates, but she shrugs off the looks and comments. She has fought hard to be here. Aminata is studying in Bamako, the capital of Mali. Just a quarter of Malian girls complete secondary school, according to UNICEF. But even if she will graduate later than most, Aminata is conscious of how far she has come. “I wanted to go to high school but I needed to pass some exams to get here. In the end, it took me three years,” she said. At the start of her final year of collège, or middle school, Aminata got pregnant. She is far from alone: 38% of Malian girls will be pregnant or a mother by the age of 18. Abortion is illegal in Mali except in cases of rape, incest or danger to the mother’s life, and even then it is difficult to obtain, according to medical professionals. Determined to take control of her life “I felt a lot of stigma from my classmates and even my teachers. I tried to ignore them and carry on going to school and studying. But I gave birth to my daughter just before my exams, so I couldn’t take them.” Aminata went through her pregnancy with little support, as the father of her daughter, Fatoumata, distanced himself from her after arguments about their situation. “I have had some problems with the father of the baby. We fought a lot and I didn’t see him for most of the pregnancy, right until the birth,” she recalled. The first year of her daughter’s life was a blur of doctors’ appointments, as Fatoumata was often ill. It seemed Aminata’s chances of finishing school were slipping away. But gradually her family began to take a more active role in caring for her daughter, and she began demanding more help from Fatoumata’s father too. She went back to school in the autumn, 18 months after Fatoumata’s birth and with more determination than ever. She no longer had time to hang out with friends after school, but attended classes, took care of her daughter and then studied more. At the end of the academic year, it paid off. “I did it. I passed my exams and now I am in high school,” Aminata said, smiling and relaxing her shoulders. "Family planning protects girls" Aminata’s next goal is her high school diploma, and obtaining it while trying to navigate the difficult world of relationships and sex. “It’s something you can talk about with your close friends. I would be too ashamed to talk about this with my parents,” she said. She is guided by visits from the young volunteers of the Association Malienne pour la Protection et Promotion de la Famille (AMPPF), and shares her own story with classmates who she sees at risk. “The guys come up to you and tell you that you are beautiful, but if you don’t want to sleep with them they will rape you. That’s the choice. You can accept or you can refuse and they will rape you anyway,” she said. “Girls have to know their rights”. After listening to the volunteers talk about all the different options for contraception, she is reviewing her own choices. “Family planning protects girls,” Aminata said. “It means we can protect ourselves from pregnancies that we don’t want”.

| 18 April 2024
"Girls have to know their rights"
Aminata Sonogo listened intently to the group of young volunteers as they explained different types of contraception, and raised her hand with questions. Sitting at a wooden school desk at 22, Aminata is older than most of her classmates, but she shrugs off the looks and comments. She has fought hard to be here. Aminata is studying in Bamako, the capital of Mali. Just a quarter of Malian girls complete secondary school, according to UNICEF. But even if she will graduate later than most, Aminata is conscious of how far she has come. “I wanted to go to high school but I needed to pass some exams to get here. In the end, it took me three years,” she said. At the start of her final year of collège, or middle school, Aminata got pregnant. She is far from alone: 38% of Malian girls will be pregnant or a mother by the age of 18. Abortion is illegal in Mali except in cases of rape, incest or danger to the mother’s life, and even then it is difficult to obtain, according to medical professionals. Determined to take control of her life “I felt a lot of stigma from my classmates and even my teachers. I tried to ignore them and carry on going to school and studying. But I gave birth to my daughter just before my exams, so I couldn’t take them.” Aminata went through her pregnancy with little support, as the father of her daughter, Fatoumata, distanced himself from her after arguments about their situation. “I have had some problems with the father of the baby. We fought a lot and I didn’t see him for most of the pregnancy, right until the birth,” she recalled. The first year of her daughter’s life was a blur of doctors’ appointments, as Fatoumata was often ill. It seemed Aminata’s chances of finishing school were slipping away. But gradually her family began to take a more active role in caring for her daughter, and she began demanding more help from Fatoumata’s father too. She went back to school in the autumn, 18 months after Fatoumata’s birth and with more determination than ever. She no longer had time to hang out with friends after school, but attended classes, took care of her daughter and then studied more. At the end of the academic year, it paid off. “I did it. I passed my exams and now I am in high school,” Aminata said, smiling and relaxing her shoulders. "Family planning protects girls" Aminata’s next goal is her high school diploma, and obtaining it while trying to navigate the difficult world of relationships and sex. “It’s something you can talk about with your close friends. I would be too ashamed to talk about this with my parents,” she said. She is guided by visits from the young volunteers of the Association Malienne pour la Protection et Promotion de la Famille (AMPPF), and shares her own story with classmates who she sees at risk. “The guys come up to you and tell you that you are beautiful, but if you don’t want to sleep with them they will rape you. That’s the choice. You can accept or you can refuse and they will rape you anyway,” she said. “Girls have to know their rights”. After listening to the volunteers talk about all the different options for contraception, she is reviewing her own choices. “Family planning protects girls,” Aminata said. “It means we can protect ourselves from pregnancies that we don’t want”.

| 08 January 2021
"The movement helps girls to know their rights and their bodies"
My name is Fatoumata Yehiya Maiga. I’m 23-years-old, and I’m an IT specialist. I joined the Youth Action Movement at the end of 2018. The head of the movement in Mali is a friend of mine, and I met her before I knew she was the president. She invited me to their events and over time persuaded me to join. I watched them raising awareness about sexual and reproductive health, using sketches and speeches. I learnt a lot. Overcoming taboos I went home and talked about what I had seen and learnt with my family. In Africa, and even more so in the village where I come from in Gao, northern Mali, people don’t talk about these things. I wanted to take my sisters to the events, but every time I spoke about them my relatives would just say it was to teach girls to have sex, and that it’s taboo. That’s not what I believe. I think the movement helps girls, most of all, to know their sexual rights, their bodies, what to do and what not to do to stay healthy and safe. They don’t understand this concept. My family would say it was just a smokescreen to convince girls to get involved in something dirty. I have had to tell my younger cousins about their periods, for example, when they came from the village to live in the city. One of my cousins was so scared, and told me she was bleeding from her vagina and didn’t know why. We talk about managing periods in the Youth Action Movement, as well as how to manage cramps and feel better. The devastating impact of FGM But there was a much more important reason for me to join the movement. My parents are educated, so me and my sisters were never cut. I learned about female genital mutilation at a conference I attended in 2016. I didn’t know that there were different types of severity and ways that girls could be cut. I hadn’t understood quite how dangerous this practice is. Then, two years ago, I lost my friend Aïssata. She got married young, at 17. She struggled to conceive until she was 23. The day she gave birth, there were complications and she died. The doctors said that the excision was botched and that’s what killed her. From that day on, I decided I needed to teach all the girls in my community about how harmful this practice is for their health. I was so horrified by the way she died. Normally, girls in Mali are cut when they are three or four years old, though for some it’s done at birth. When they are older and get pregnant, I know they face the same challenges as every woman does giving birth, but they also live with the dangerous consequences of this unhealthy practice. The importance of talking openly The problem lies with the families. I want us, as a movement, to talk with the parents and explain to them how they can contribute to their children’s sexual health. I wish it were no longer a taboo between parents and their girls. But if we talk in such direct terms, they only see disobedience, and say that we are encouraging promiscuity. We need to talk to teenagers because they are already parents in many cases. They are the ones who decide to go through with cutting their daughters, or not. A lot of Mali is hard to reach though. We need travelling groups to go to those isolated rural areas and talk to people about sexual health. Pregnancy is the girl’s decision, and girls have a right to be healthy, and to choose their future.

| 18 April 2024
"The movement helps girls to know their rights and their bodies"
My name is Fatoumata Yehiya Maiga. I’m 23-years-old, and I’m an IT specialist. I joined the Youth Action Movement at the end of 2018. The head of the movement in Mali is a friend of mine, and I met her before I knew she was the president. She invited me to their events and over time persuaded me to join. I watched them raising awareness about sexual and reproductive health, using sketches and speeches. I learnt a lot. Overcoming taboos I went home and talked about what I had seen and learnt with my family. In Africa, and even more so in the village where I come from in Gao, northern Mali, people don’t talk about these things. I wanted to take my sisters to the events, but every time I spoke about them my relatives would just say it was to teach girls to have sex, and that it’s taboo. That’s not what I believe. I think the movement helps girls, most of all, to know their sexual rights, their bodies, what to do and what not to do to stay healthy and safe. They don’t understand this concept. My family would say it was just a smokescreen to convince girls to get involved in something dirty. I have had to tell my younger cousins about their periods, for example, when they came from the village to live in the city. One of my cousins was so scared, and told me she was bleeding from her vagina and didn’t know why. We talk about managing periods in the Youth Action Movement, as well as how to manage cramps and feel better. The devastating impact of FGM But there was a much more important reason for me to join the movement. My parents are educated, so me and my sisters were never cut. I learned about female genital mutilation at a conference I attended in 2016. I didn’t know that there were different types of severity and ways that girls could be cut. I hadn’t understood quite how dangerous this practice is. Then, two years ago, I lost my friend Aïssata. She got married young, at 17. She struggled to conceive until she was 23. The day she gave birth, there were complications and she died. The doctors said that the excision was botched and that’s what killed her. From that day on, I decided I needed to teach all the girls in my community about how harmful this practice is for their health. I was so horrified by the way she died. Normally, girls in Mali are cut when they are three or four years old, though for some it’s done at birth. When they are older and get pregnant, I know they face the same challenges as every woman does giving birth, but they also live with the dangerous consequences of this unhealthy practice. The importance of talking openly The problem lies with the families. I want us, as a movement, to talk with the parents and explain to them how they can contribute to their children’s sexual health. I wish it were no longer a taboo between parents and their girls. But if we talk in such direct terms, they only see disobedience, and say that we are encouraging promiscuity. We need to talk to teenagers because they are already parents in many cases. They are the ones who decide to go through with cutting their daughters, or not. A lot of Mali is hard to reach though. We need travelling groups to go to those isolated rural areas and talk to people about sexual health. Pregnancy is the girl’s decision, and girls have a right to be healthy, and to choose their future.

| 13 August 2020
In pictures: Delivering healthcare to remote communities in Fiji
In early April 2020, the all too familiar destruction of a Tropical Cyclone (TC) – Harold – hit the Solomon Islands, Vanuatu, Fiji and Tonga. One of the worst affected areas was the Eastern part of Fiji. Through support by Department of Foreign Affairs and Trade (DFAT), our Member Association, Reproductive and Family Health Association of Fiji (RFHAF), was quick to respond ensuring access to essential sexual and reproductive healthcare for Kadavu’s women, girls, and vulnerable groups. Fiji's vulnerable coastline Fiji’s worst affected area was the Eastern part, with TC Harold bringing destructive storm force winds and storm surge. RFHAF focused its humanitarian response on the local Kadavu population. This remote area proves a challenge to reach for the team with supplies. Share on Twitter Share on Facebook Share via WhatsApp Share via Email RFHAF's humanitarian response team tackle rough terrain National travel restrictions - due to the current COVID-19 pandemic - on all inter island transfers has slowed the response in some areas, including Kadavu. The island of Kadavu is one of the least developed areas of Fiji, the main source of income is substance living (Yaqona). Transport around the island is difficult, with very few roads, no public water system or electricity. The humanitarian team from RFHAF travels by boat and then on foot. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Asenaca, client Kadavu, the biggest island in the Eastern division has the greatest population (10,897). 197 evacuation centres were activated in total, initially hosting over 6,240 people. Many are women of reproductive age, with an estimated 150 currently pregnant. Asenaca learns about breast cancer self-checks from RFHAF’s healthcare provider, Karo. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nasi, RFHAF healthcare provider The medical mobile team deliver a broad range of healthcare including contraception, information and counselling on sexual health, pregnancy, HIV and STI care and testing. RFHAF Team in Kadavu performing general health checks after TC Harold. Nasi administers a HPV shot to a client. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Kate, client Young women and girls are at the heart of RFHAF’s healthcare provision. Kate walks home with her dignity kit after a health check at the mobile clinic. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Karo, RFHAF healthcare worker RFHAF offers sexual and reproductive healthcare as well as counselling, and referrals for follow up care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Alidi, RFHAF healthcare worker The team ensures young people in the community are not forgotten and provide information and education on relationships and sexual health and rights. Alidi conducting a session with a local group of young people at Gasele, Kadavu.Photos ©IPPF/Rob Rickman/Fiji Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 18 April 2024
In pictures: Delivering healthcare to remote communities in Fiji
In early April 2020, the all too familiar destruction of a Tropical Cyclone (TC) – Harold – hit the Solomon Islands, Vanuatu, Fiji and Tonga. One of the worst affected areas was the Eastern part of Fiji. Through support by Department of Foreign Affairs and Trade (DFAT), our Member Association, Reproductive and Family Health Association of Fiji (RFHAF), was quick to respond ensuring access to essential sexual and reproductive healthcare for Kadavu’s women, girls, and vulnerable groups. Fiji's vulnerable coastline Fiji’s worst affected area was the Eastern part, with TC Harold bringing destructive storm force winds and storm surge. RFHAF focused its humanitarian response on the local Kadavu population. This remote area proves a challenge to reach for the team with supplies. Share on Twitter Share on Facebook Share via WhatsApp Share via Email RFHAF's humanitarian response team tackle rough terrain National travel restrictions - due to the current COVID-19 pandemic - on all inter island transfers has slowed the response in some areas, including Kadavu. The island of Kadavu is one of the least developed areas of Fiji, the main source of income is substance living (Yaqona). Transport around the island is difficult, with very few roads, no public water system or electricity. The humanitarian team from RFHAF travels by boat and then on foot. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Asenaca, client Kadavu, the biggest island in the Eastern division has the greatest population (10,897). 197 evacuation centres were activated in total, initially hosting over 6,240 people. Many are women of reproductive age, with an estimated 150 currently pregnant. Asenaca learns about breast cancer self-checks from RFHAF’s healthcare provider, Karo. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nasi, RFHAF healthcare provider The medical mobile team deliver a broad range of healthcare including contraception, information and counselling on sexual health, pregnancy, HIV and STI care and testing. RFHAF Team in Kadavu performing general health checks after TC Harold. Nasi administers a HPV shot to a client. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Kate, client Young women and girls are at the heart of RFHAF’s healthcare provision. Kate walks home with her dignity kit after a health check at the mobile clinic. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Karo, RFHAF healthcare worker RFHAF offers sexual and reproductive healthcare as well as counselling, and referrals for follow up care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Alidi, RFHAF healthcare worker The team ensures young people in the community are not forgotten and provide information and education on relationships and sexual health and rights. Alidi conducting a session with a local group of young people at Gasele, Kadavu.Photos ©IPPF/Rob Rickman/Fiji Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 28 July 2020
"I wanted to protect girls from violence – like early marriage – and I wanted to change people’s wrong perceptions about sex and sexuality"
Seventeen-year-old student Jumeya Mohammed Amin started educating other people about sexual and reproductive health when she was 14 years old. She trained as a ‘change agent’ for her community through the Family Guidance Association of Ethiopia’s south west office in Jimma, the capital of Oromia region. Amin comes from a small, conservative town about 20km outside the city. "I wanted to protect girls from violence – like early marriage – and I wanted to change people’s wrong perceptions about sex and sexuality, because they [men in her community] start having sex with girls at a young age, even with girls as young as nine years old, because of a lack of education." "They suddenly had to act like grown-up women" "Before I started this training I saw the majority of students having sex early and getting pregnant because of a lack of information, and they would have to leave home and school. Boys would be disciplined and if they were seen doing things on campus, expelled. Girls younger than me at the time were married. The youngest was only nine. They would have to go back home and could not play anymore or go to school. They suddenly had to act like grown-up women, like old ladies. They never go back to school after marriage. My teacher chose me for this training and told me about the programme. I like the truth so I was not afraid. I heard about a lot of problems out there during my training and I told myself I had to be strong and go and fight this." "I have a brother and four sisters and I practiced my training on my family first. They were so shocked by what I was saying they were silent. Even on the second day, they said nothing. On the third day, I told them I was going to teach people in schools this, so I asked them why they had stayed silent. They told me that because of cultural and religious issues, people would not accept these ideas and stories, but they gave me permission to go and do it. Because of my efforts, people in my school have not started having sex early and the girls get free sanitary pads through the clubs so they no longer need to stay home during periods." Training hundreds of her peers "I know people in my community who have unplanned pregnancies consult traditional healers [for abortions] and take drugs and they suffer. I know one girl from 10th grade who was 15 years old and died from this in 2017. The healers sometimes use tree leaves in their concoctions. We tell them where they can go and get different [safe abortion] services. The first round of trainings I did was with 400 students over four months and eight sessions in 2017. Last year, I trained 600 people and this year in the first trimester of school I trained 400. When students finish the course, they want to do it again, and when we forget we have a session, they come and remind me. At school, they call me a teacher. I’d like to be a doctor and this training has really made me want to do that more."

| 18 April 2024
"I wanted to protect girls from violence – like early marriage – and I wanted to change people’s wrong perceptions about sex and sexuality"
Seventeen-year-old student Jumeya Mohammed Amin started educating other people about sexual and reproductive health when she was 14 years old. She trained as a ‘change agent’ for her community through the Family Guidance Association of Ethiopia’s south west office in Jimma, the capital of Oromia region. Amin comes from a small, conservative town about 20km outside the city. "I wanted to protect girls from violence – like early marriage – and I wanted to change people’s wrong perceptions about sex and sexuality, because they [men in her community] start having sex with girls at a young age, even with girls as young as nine years old, because of a lack of education." "They suddenly had to act like grown-up women" "Before I started this training I saw the majority of students having sex early and getting pregnant because of a lack of information, and they would have to leave home and school. Boys would be disciplined and if they were seen doing things on campus, expelled. Girls younger than me at the time were married. The youngest was only nine. They would have to go back home and could not play anymore or go to school. They suddenly had to act like grown-up women, like old ladies. They never go back to school after marriage. My teacher chose me for this training and told me about the programme. I like the truth so I was not afraid. I heard about a lot of problems out there during my training and I told myself I had to be strong and go and fight this." "I have a brother and four sisters and I practiced my training on my family first. They were so shocked by what I was saying they were silent. Even on the second day, they said nothing. On the third day, I told them I was going to teach people in schools this, so I asked them why they had stayed silent. They told me that because of cultural and religious issues, people would not accept these ideas and stories, but they gave me permission to go and do it. Because of my efforts, people in my school have not started having sex early and the girls get free sanitary pads through the clubs so they no longer need to stay home during periods." Training hundreds of her peers "I know people in my community who have unplanned pregnancies consult traditional healers [for abortions] and take drugs and they suffer. I know one girl from 10th grade who was 15 years old and died from this in 2017. The healers sometimes use tree leaves in their concoctions. We tell them where they can go and get different [safe abortion] services. The first round of trainings I did was with 400 students over four months and eight sessions in 2017. Last year, I trained 600 people and this year in the first trimester of school I trained 400. When students finish the course, they want to do it again, and when we forget we have a session, they come and remind me. At school, they call me a teacher. I’d like to be a doctor and this training has really made me want to do that more."

| 16 July 2020
"Before, there was no safe abortion"
Rewda Kedir works as a midwife in a rural area of the Oromia region in southwest Ethiopia. Only 14% of married women are using any method of contraception here. The government hospital Rewda works in is supported to provide a full range of sexual and reproductive healthcare, which includes providing free contraceptives and comprehensive abortion care. In January 2017, the maternal healthcare clinic faced shortages of contraceptives after the US administration reactivated and expanded the Global Gag Rule, which does not allow any funding to go to organizations associated with providing abortion care. Fortunately in this case, the shortages only lasted a month due to the government of the Netherlands stepping in and matching lost funding. “Before, we had a shortage of contraceptive pills and emergency contraceptives. We would have to give people prescriptions and they would go to private clinics and where they had to pay," Rewda tells us. "When I first came to this clinic, there was a real shortage of people trained in family planning. I was the only one. Now there are many people trained on family planning, and when I’m not here, people can help." "There used to be a shortage of choice and alternatives, and now there are many. And the implant procedures are better because there are newer products that are much smaller so putting them in is less invasive.” Opening a dialogue on contraception The hospital has been providing medical abortions for six years. “Before, there was no safe abortion," says Rewda. She explains how people would go to 'traditional' healers and then come to the clinic with complications like sepsis, bleeding, anaemia and toxic shock. If they had complications or infections above nine weeks, Rewda and her colleagues would send them to Jimma, the regional capital. "Before, it was very difficult to persuade them to use family planning, and we had to have a lot of conversations. Now, they come 45 days after delivery to speak to us about this and get their babies immunised," she explains. "They want contraceptives to space out their children. Sometimes their husbands don’t like them coming to get family planning so we have to lock their appointment cards away. Their husbands want more children and they think that women who do not keep having their children will go with other men." "More kids, more wealth" Rewda tells us that they've used family counselling to try and persuade men to reconsider their ideas about contraception, by explaining to them that continuously giving birth under unsafe circumstances can affect a woman's health and might lead to maternal death, damage the uterus and lead to long-term complications. "Here, people believe that more kids means more wealth, and religion restricts family planning services. Before, they did not have good training on family planning and abortion. Now, women that have abortions get proper care and the counseling and education has improved. There are still unsafe abortions but they have really reduced. We used to see about 40 a year and now it’s one or two." However, problems still exist. "There are some complications, like irregular bleeding from some contraceptives," Rewda says, and that "women still face conflict with their husbands over family planning and sometimes have to go to court to fight this or divorce them.”

| 18 April 2024
"Before, there was no safe abortion"
Rewda Kedir works as a midwife in a rural area of the Oromia region in southwest Ethiopia. Only 14% of married women are using any method of contraception here. The government hospital Rewda works in is supported to provide a full range of sexual and reproductive healthcare, which includes providing free contraceptives and comprehensive abortion care. In January 2017, the maternal healthcare clinic faced shortages of contraceptives after the US administration reactivated and expanded the Global Gag Rule, which does not allow any funding to go to organizations associated with providing abortion care. Fortunately in this case, the shortages only lasted a month due to the government of the Netherlands stepping in and matching lost funding. “Before, we had a shortage of contraceptive pills and emergency contraceptives. We would have to give people prescriptions and they would go to private clinics and where they had to pay," Rewda tells us. "When I first came to this clinic, there was a real shortage of people trained in family planning. I was the only one. Now there are many people trained on family planning, and when I’m not here, people can help." "There used to be a shortage of choice and alternatives, and now there are many. And the implant procedures are better because there are newer products that are much smaller so putting them in is less invasive.” Opening a dialogue on contraception The hospital has been providing medical abortions for six years. “Before, there was no safe abortion," says Rewda. She explains how people would go to 'traditional' healers and then come to the clinic with complications like sepsis, bleeding, anaemia and toxic shock. If they had complications or infections above nine weeks, Rewda and her colleagues would send them to Jimma, the regional capital. "Before, it was very difficult to persuade them to use family planning, and we had to have a lot of conversations. Now, they come 45 days after delivery to speak to us about this and get their babies immunised," she explains. "They want contraceptives to space out their children. Sometimes their husbands don’t like them coming to get family planning so we have to lock their appointment cards away. Their husbands want more children and they think that women who do not keep having their children will go with other men." "More kids, more wealth" Rewda tells us that they've used family counselling to try and persuade men to reconsider their ideas about contraception, by explaining to them that continuously giving birth under unsafe circumstances can affect a woman's health and might lead to maternal death, damage the uterus and lead to long-term complications. "Here, people believe that more kids means more wealth, and religion restricts family planning services. Before, they did not have good training on family planning and abortion. Now, women that have abortions get proper care and the counseling and education has improved. There are still unsafe abortions but they have really reduced. We used to see about 40 a year and now it’s one or two." However, problems still exist. "There are some complications, like irregular bleeding from some contraceptives," Rewda says, and that "women still face conflict with their husbands over family planning and sometimes have to go to court to fight this or divorce them.”

| 18 June 2020
In pictures: Healthcare in the face of the climate crisis in Kiribati
Humanitarian crises Largely brought on by sudden onset and slow-onset natural disasters, humanitarian crises are increasingly prevalent in the Pacific. During responses to humanitarian crises in the Pacific, sexual and reproductive healthcare is often under-prioritised and under-resourced. As a result, women and girls of reproductive age and vulnerable and marginalized groups are disproportionately affected and facing increased health and psychosocial risks. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Fragile environments Low topography, rising sea levels and insufficient fresh water supply leaves Kiribati’s population vulnerable to the effects of the climate crisis. The fragility of the outer islands of Kiribati during natural disasters is compounded by their geographic isolation, which makes transportation and communication during post-disaster relief and response both expensive and difficult. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Coastal exposure The majority of the population of 115,000 people live a subsistence lifestyle. Communities are geographically dispersed across 33 atolls covering 3.5 million square kilometres in the central Pacific Ocean. The population and infrastructure within Kiribati are largely concentrated on the coast, where communities face increased exposure to climate threats and natural hazards such as tsunamis, earthquakes, king tides, flooding, droughts, and occasionally cyclones. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Takaria, leader and youth organizer in the Tebikenikua community Takaria will be running to be a Member of Parliament in Kiribati in 2020. “I assist the youth with family problems and family planning and disasters. In our community there are unforeseen pregnancies, domestic violence, and disasters such as high tide waters and strong winds, which can also affect this community. The Kiribati Family Health Association (KFHA) is the key point for us with outreach and training so people in this community know how to prevent and treat STIs, etc. They all know where the KFHA clinic is and that they can get counselling or services there. The problem now is you can’t survive with the sea rise levels. I want all members of my community to live better and have better health and peace.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Susan*, sex worker Susan receives care at the Kiribati Family Health Association (KFHA) including a pap smear. Susan*, 28, is a sex worker from the town of Betio on the main island of Kiribati. Originally from an outlying island, she moved into Tarawa to seek work. Unable to find employment that would fulfill her dream of sending money back to her two children, she was introduced to sex work. With other sex workers, she regularly travels out to the large cargo ships from China, Philippines and Korea anchored off the coast of Kiribati. Despite her new income, she still can’t speak with her children or see them due to the restrictive costs involved of travel between islands.*pseudonym Share on Twitter Share on Facebook Share via WhatsApp Share via Email Theta, 25-year-old mother and youth volunteer Theta is part of the Humanitarian Youth Club set up by the Kiribati Family Health Association in her village. “We face a lot of situations here, one of them is disasters and the second is unemployment and school drop out with our youth. I have helped the Humanitarian Youth Club to apply for financial grants from the Australian High Commission [for $1,000] I am recognized as the smartest member who can write in English. We have learned how to design a disaster plan for the community and share our ideas on sexual and reproductive issues such as STIs. We discuss what we can do for the next strong tide, where we can gather as a community and what we can do if even the maneabe (town hall) floods? If the tide and wind is too strong, we need to go to another safer place, such as another community’s town hall. For now, I want to enjoy the chance to be in our own beloved country. I won’t move until the majority have already left. I want my daughter to grow up in the same place I grew up in.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Beitau, youth volunteer Beitau is the Chairperson of the Humanitarian Youth Club. “I was lucky to be selected as Chairperson as the Humanitarian Youth Club. I feel like I get more respect from the community now I am in this position. I would love advanced training on leadership now, to further assist the club. As I am the Chairperson of the HYC, my main target is to help people during a disaster. I have attended training through KFHA. What I took from this is that when a disaster strikes, we have to do our best for pregnant women, small children and people with disabilities. They more vulnerable and less able to survive a disaster.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Abe, youth officer Abe was involved with KFHA since 2012. “I was inspired by what they KFHA was doing and the issues they were addressing that affects youth. I was surprised to see how many young people come to the clinic as they are affected by STIs, HIV and teenage pregnancy. The lack of education here is a big problem, most people here have a lot of children and yet can’t afford to send them to school. Sexual and reproductive health is our responsibility and we must talk about it with young people. Climate change affects many countries, but Kiribati is small and low lying. I used to go visit a very nice beach with a lot of nice trees and plants. Now, the trees are gone, and the waves have taken over, and the houses have disappeared so no one can build there. In my role as a youth worker and activist, I tell people to fight climate change: to grow more mangroves, to clean up the beach, because we love our Kiribati.”©IPPF/Hannah Maule-Ffinch/Kiribati Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 18 April 2024
In pictures: Healthcare in the face of the climate crisis in Kiribati
Humanitarian crises Largely brought on by sudden onset and slow-onset natural disasters, humanitarian crises are increasingly prevalent in the Pacific. During responses to humanitarian crises in the Pacific, sexual and reproductive healthcare is often under-prioritised and under-resourced. As a result, women and girls of reproductive age and vulnerable and marginalized groups are disproportionately affected and facing increased health and psychosocial risks. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Fragile environments Low topography, rising sea levels and insufficient fresh water supply leaves Kiribati’s population vulnerable to the effects of the climate crisis. The fragility of the outer islands of Kiribati during natural disasters is compounded by their geographic isolation, which makes transportation and communication during post-disaster relief and response both expensive and difficult. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Coastal exposure The majority of the population of 115,000 people live a subsistence lifestyle. Communities are geographically dispersed across 33 atolls covering 3.5 million square kilometres in the central Pacific Ocean. The population and infrastructure within Kiribati are largely concentrated on the coast, where communities face increased exposure to climate threats and natural hazards such as tsunamis, earthquakes, king tides, flooding, droughts, and occasionally cyclones. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Takaria, leader and youth organizer in the Tebikenikua community Takaria will be running to be a Member of Parliament in Kiribati in 2020. “I assist the youth with family problems and family planning and disasters. In our community there are unforeseen pregnancies, domestic violence, and disasters such as high tide waters and strong winds, which can also affect this community. The Kiribati Family Health Association (KFHA) is the key point for us with outreach and training so people in this community know how to prevent and treat STIs, etc. They all know where the KFHA clinic is and that they can get counselling or services there. The problem now is you can’t survive with the sea rise levels. I want all members of my community to live better and have better health and peace.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Susan*, sex worker Susan receives care at the Kiribati Family Health Association (KFHA) including a pap smear. Susan*, 28, is a sex worker from the town of Betio on the main island of Kiribati. Originally from an outlying island, she moved into Tarawa to seek work. Unable to find employment that would fulfill her dream of sending money back to her two children, she was introduced to sex work. With other sex workers, she regularly travels out to the large cargo ships from China, Philippines and Korea anchored off the coast of Kiribati. Despite her new income, she still can’t speak with her children or see them due to the restrictive costs involved of travel between islands.*pseudonym Share on Twitter Share on Facebook Share via WhatsApp Share via Email Theta, 25-year-old mother and youth volunteer Theta is part of the Humanitarian Youth Club set up by the Kiribati Family Health Association in her village. “We face a lot of situations here, one of them is disasters and the second is unemployment and school drop out with our youth. I have helped the Humanitarian Youth Club to apply for financial grants from the Australian High Commission [for $1,000] I am recognized as the smartest member who can write in English. We have learned how to design a disaster plan for the community and share our ideas on sexual and reproductive issues such as STIs. We discuss what we can do for the next strong tide, where we can gather as a community and what we can do if even the maneabe (town hall) floods? If the tide and wind is too strong, we need to go to another safer place, such as another community’s town hall. For now, I want to enjoy the chance to be in our own beloved country. I won’t move until the majority have already left. I want my daughter to grow up in the same place I grew up in.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Beitau, youth volunteer Beitau is the Chairperson of the Humanitarian Youth Club. “I was lucky to be selected as Chairperson as the Humanitarian Youth Club. I feel like I get more respect from the community now I am in this position. I would love advanced training on leadership now, to further assist the club. As I am the Chairperson of the HYC, my main target is to help people during a disaster. I have attended training through KFHA. What I took from this is that when a disaster strikes, we have to do our best for pregnant women, small children and people with disabilities. They more vulnerable and less able to survive a disaster.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Abe, youth officer Abe was involved with KFHA since 2012. “I was inspired by what they KFHA was doing and the issues they were addressing that affects youth. I was surprised to see how many young people come to the clinic as they are affected by STIs, HIV and teenage pregnancy. The lack of education here is a big problem, most people here have a lot of children and yet can’t afford to send them to school. Sexual and reproductive health is our responsibility and we must talk about it with young people. Climate change affects many countries, but Kiribati is small and low lying. I used to go visit a very nice beach with a lot of nice trees and plants. Now, the trees are gone, and the waves have taken over, and the houses have disappeared so no one can build there. In my role as a youth worker and activist, I tell people to fight climate change: to grow more mangroves, to clean up the beach, because we love our Kiribati.”©IPPF/Hannah Maule-Ffinch/Kiribati Share on Twitter Share on Facebook Share via WhatsApp Share via Email