Spotlight
A selection of stories from across the Federation

France, Germany, Poland, United Kingdom, United States, Colombia, India, Tunisia
Abortion Rights: Latest Decisions and Developments around the World
The global landscape of abortion rights continues to evolve in 2024, with new legislation and feminist movements fighting for better access. Let's take a trip around the world to see the latest developments.
Most Popular This Week
France, Germany, Poland, United Kingdom, United States, Colombia, India, Tunisia

Abortion Rights: Latest Decisions and Developments around the World
Over the past 30 years, more than

Palestine

In their own words: The people providing sexual and reproductive health care under bombardment in Gaza
Week after week, heavy Israeli bombardment from air, land, and sea, has continued across most of the Gaza Strip.
Vanuatu

When getting to the hospital is difficult, Vanuatu mobile outreach can save lives
In the mountains of Kumera on Tanna Island, Vanuatu, the village women of Kamahaul normally spend over 10,000 Vatu ($83 USD) to travel to the nearest hospital.
Vanuatu

Sex: changing minds and winning hearts in Tanna, Vanuatu
“Very traditional.” These two words are often used to describe the people of Tanna in Vanuatu, one of the most populated islands in the small country in the Pacific.
Vanuatu

Vanuatu cyclone response: The mental health toll on humanitarian providers
Girls and women from nearby villages flock to mobile health clinics set up by the Vanuatu Family Health Association (VFHA).
Cook Islands

Trans & Proud: Being Transgender in the Cook Islands
It’s a scene like many others around the world: a loving family pour over childhood photos, giggling and reminiscing about the memories.
Cook Islands

In Pictures: The activists who helped win LGBTI+ rights in the Cook Islands
The Cook Islands has removed a law that criminalizes homosexuality, in a huge victory for the local LGBTI+ community.
Filter our stories by:
- Afghanistan
- Albania
- Aruba
- Bangladesh
- Benin
- Botswana
- Burundi
- Cambodia
- Cameroon
- Colombia
- Congo, Dem. Rep.
- Cook Islands
- El Salvador
- Ethiopia
- Fiji
- France
- Germany
- Ghana
- Guinea-Conakry
- India
- Ireland
- Jamaica
- Kenya
- Kiribati
- Lesotho
- Malawi
- Mali
- Mozambique
- Nepal
- Nigeria
- Pakistan
- Palestine
- Poland
- Senegal
- Somaliland
- Sri Lanka
- Sudan
- Thailand
- Togo
- Tonga
- Trinidad and Tobago
- Tunisia
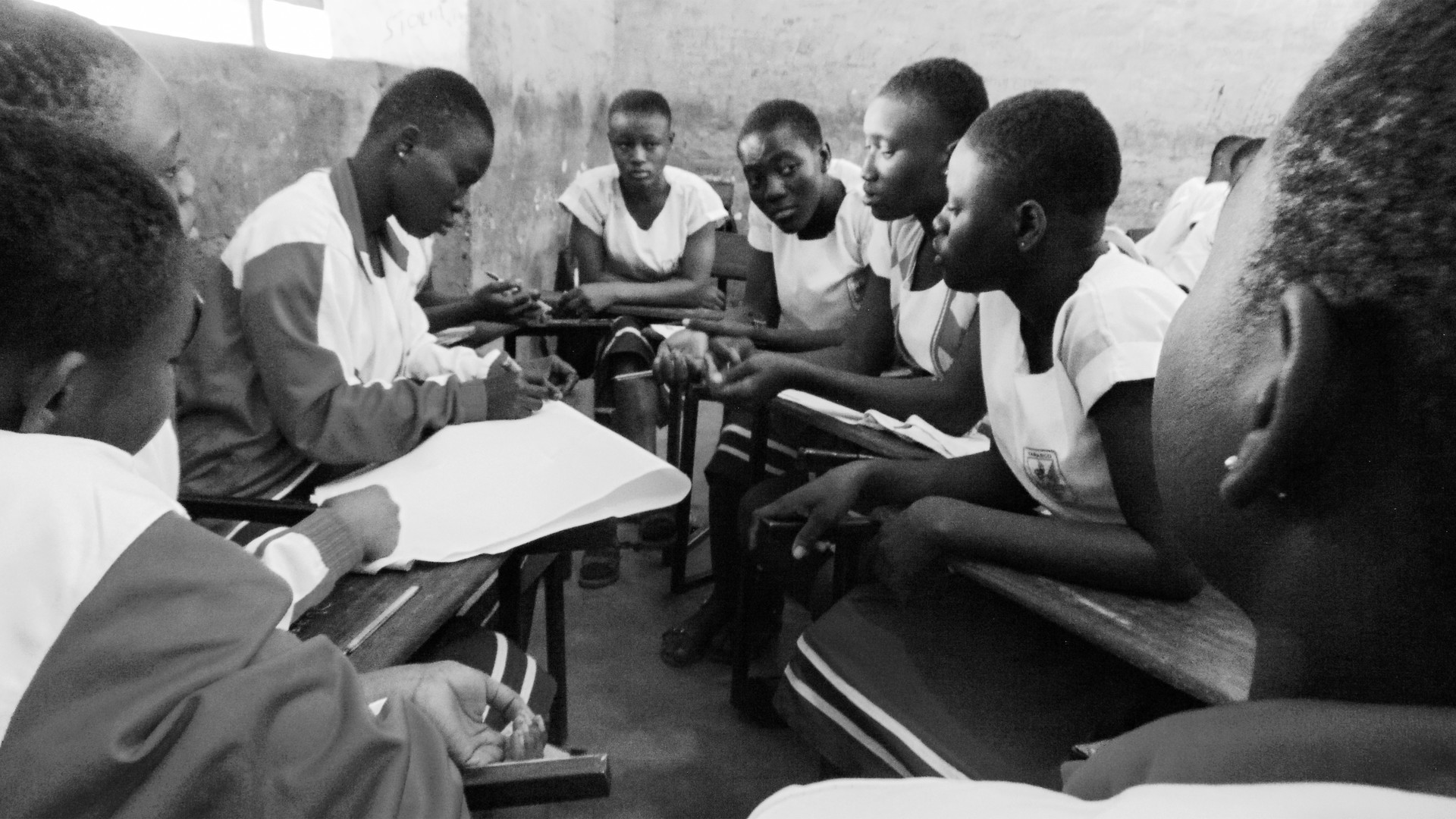
- Uganda
- United Kingdom
- United States
- Vanuatu
- Zambia
- Afghan Family Guidance Association
- Albanian Center for Population and Development
- Asociación Pro-Bienestar de la Familia Colombiana
- Associação Moçambicana para Desenvolvimento da Família
- Association Béninoise pour la Promotion de la Famille
- Association Burundaise pour le Bien-Etre Familial
- Association Malienne pour la Protection et la Promotion de la Famille
- Association pour le Bien-Etre Familial/Naissances Désirables
- Association Sénégalaise pour le Bien-Étre Familial
- Association Togolaise pour le Bien-Etre Familial
- Association Tunisienne de la Santé de la Reproduction
- Botswana Family Welfare Association
- Cameroon National Association for Family Welfare
- Cook Islands Family Welfare Association
- Family Guidance Association of Ethiopia
- Family Planning Association of India
- Family Planning Association of Malawi
- Family Planning Association of Nepal
- Family Planning Association of Sri Lanka
- Family Planning Association of Trinidad and Tobago
- Foundation for the Promotion of Responsible Parenthood - Aruba
- Indonesian Planned Parenthood Association
- Jamaica Family Planning Association
- Kiribati Family Health Association
- Lesotho Planned Parenthood Association
- Mouvement Français pour le Planning Familial
- Palestinian Family Planning and Protection Association (PFPPA)
- Planned Parenthood Association of Ghana
- Planned Parenthood Association of Thailand
- Planned Parenthood Association of Zambia
- Planned Parenthood Federation of America
- Planned Parenthood Federation of Nigeria
- Pro Familia - Germany
- Rahnuma-Family Planning Association of Pakistan
- Reproductive & Family Health Association of Fiji
- Reproductive Health Association of Cambodia (RHAC)
- Reproductive Health Uganda
- Somaliland Family Health Association
- Sudan Family Planning Association
- Tonga Family Health Association
- Vanuatu Family Health Association


| 04 May 2017
In the eye of the storm
Cyclone Winston, which devastated Fiji, was the strongest to ever hit the South Pacific. IPPF’s humanitarian response there was carried out with our Member Association, the Reproductive & Family Health Association of Fiji, and is part of our SPRINT Initiative, funded by the Australian Government. My name is Verenaisi Katerina. I have five children and we live in a remote village in the Ba Highlands. At the time the cyclone hit we were all living in a timber house and I was pregnant. I’ve lived in a bure (traditional timber house with a thatched grass roof) all my life, I’m so used to living in a bure, I’m not used to living in a tin-roofed house. We tried to be prepared when the cyclone came. But we had to all rush to the evacuation centre when the roof blew off our house. My whole family was scared, our house was flooded and our crops were all damaged. My daughter was covering her eyes and ears and crying for help. While I started preparing to move to the local school to take shelter, my husband went to get us some food. I was really, really afraid. I was so worried about my kids. I told my husband not to be late and to help me out with the kids going down to the school. In the end, I managed to get my children to the school on my own, and my husband joined us later. While my family took shelter, lots of other homes in Navala were destroyed. We were lucky: most of their possessions were blown away, but some managed to survive, and our home was damaged, but remained standing. When we came back the next day, my husband tried to start repairing the kitchen so that we could move back. We had a small stove that we were using, and we made a small kitchen so at least we could cook. My husband could only get us what was left over from the farm and that’s basically what we were living on. We had to eat a lot of flour products, a lot of rice, because our farm was badly damaged. I received a dignity kit from IPPF and found it extremely helpful, particularly in clothing my children and the baby. Some of it was worn on the very same day we received it. I later took part in a family planning session conducted by IPPF. I learned a lot from the workshop on that day. I told myself, this is it. I’m only going to have five kids. Having to go through that experience of Cyclone Winston, if I had more children, then it might have been more difficult, too late, for me to run up to that school for shelter. I have had a talk with my husband and we have decided that this one is my last. My fifth is my last. Stories Read more stories about our work in Fiji after the Cyclone Winston

| 19 April 2024
In the eye of the storm
Cyclone Winston, which devastated Fiji, was the strongest to ever hit the South Pacific. IPPF’s humanitarian response there was carried out with our Member Association, the Reproductive & Family Health Association of Fiji, and is part of our SPRINT Initiative, funded by the Australian Government. My name is Verenaisi Katerina. I have five children and we live in a remote village in the Ba Highlands. At the time the cyclone hit we were all living in a timber house and I was pregnant. I’ve lived in a bure (traditional timber house with a thatched grass roof) all my life, I’m so used to living in a bure, I’m not used to living in a tin-roofed house. We tried to be prepared when the cyclone came. But we had to all rush to the evacuation centre when the roof blew off our house. My whole family was scared, our house was flooded and our crops were all damaged. My daughter was covering her eyes and ears and crying for help. While I started preparing to move to the local school to take shelter, my husband went to get us some food. I was really, really afraid. I was so worried about my kids. I told my husband not to be late and to help me out with the kids going down to the school. In the end, I managed to get my children to the school on my own, and my husband joined us later. While my family took shelter, lots of other homes in Navala were destroyed. We were lucky: most of their possessions were blown away, but some managed to survive, and our home was damaged, but remained standing. When we came back the next day, my husband tried to start repairing the kitchen so that we could move back. We had a small stove that we were using, and we made a small kitchen so at least we could cook. My husband could only get us what was left over from the farm and that’s basically what we were living on. We had to eat a lot of flour products, a lot of rice, because our farm was badly damaged. I received a dignity kit from IPPF and found it extremely helpful, particularly in clothing my children and the baby. Some of it was worn on the very same day we received it. I later took part in a family planning session conducted by IPPF. I learned a lot from the workshop on that day. I told myself, this is it. I’m only going to have five kids. Having to go through that experience of Cyclone Winston, if I had more children, then it might have been more difficult, too late, for me to run up to that school for shelter. I have had a talk with my husband and we have decided that this one is my last. My fifth is my last. Stories Read more stories about our work in Fiji after the Cyclone Winston

| 04 May 2017
Starting again in Fiji
Cyclone Winston, which devastated Fiji, was the strongest to ever hit the South Pacific. IPPF’s humanitarian response there was carried out with our Member Association, the Reproductive & Family Health Association of Fiji, and is part of our SPRINT Initiative, funded by the Australian Government. 22-year-old Sulueti arrived in the village one week after the cyclone was over. She was shocked - there was nothing left apart from the foundation of the house apart from that everything was gone. She hadn't expected it to be so bad. Her 59-year-old mother, had been sick and alone during the cyclone and she was traumatised as had never experienced a storm like that before. They tried slowly to start rebuilding a small house for them to move back into and out of the community hall. It was a difficult time because Sulueti was four-months pregnant. She managed to see a doctor three times while staying in the community hall, but there were no proper examinations or ultrasounds during this time. The delivery was fine in a maternity hospital. She received a dignity kit from IPPF and received baby supplies for post-delivery, everything that was required for a new mother to care for a baby was in the kit. IPPF went to visit her in her home and gave advice on family planning - she is taking injectables now because she doesn’t want any more children. Stories Read more stories about our work in Fiji after the Cyclone Winston

| 19 April 2024
Starting again in Fiji
Cyclone Winston, which devastated Fiji, was the strongest to ever hit the South Pacific. IPPF’s humanitarian response there was carried out with our Member Association, the Reproductive & Family Health Association of Fiji, and is part of our SPRINT Initiative, funded by the Australian Government. 22-year-old Sulueti arrived in the village one week after the cyclone was over. She was shocked - there was nothing left apart from the foundation of the house apart from that everything was gone. She hadn't expected it to be so bad. Her 59-year-old mother, had been sick and alone during the cyclone and she was traumatised as had never experienced a storm like that before. They tried slowly to start rebuilding a small house for them to move back into and out of the community hall. It was a difficult time because Sulueti was four-months pregnant. She managed to see a doctor three times while staying in the community hall, but there were no proper examinations or ultrasounds during this time. The delivery was fine in a maternity hospital. She received a dignity kit from IPPF and received baby supplies for post-delivery, everything that was required for a new mother to care for a baby was in the kit. IPPF went to visit her in her home and gave advice on family planning - she is taking injectables now because she doesn’t want any more children. Stories Read more stories about our work in Fiji after the Cyclone Winston
| 20 April 2017
Sex workers in Uganda find hope
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Lady Mermaid's Bureau. Joanne is a sex-worker who has been involved in the project run by Lady Mermaid's Bureau, funded by SAAF. "My name is Joanne, I have been a sex-worker for two years." Joanne was abused as a child and became pregnant at a very young age. She was forced to leave school with only a primary education and could not speak English very well. When she moved to Kampala from her village she was told she could get a good job but she had nowhere to stay and ended up becoming a sex-worker in order to support herself and her two children. While sex-work offers some financial support, the fact that it is illegal and that gender inequality is high in Uganda make sex workers very vulnerable to rape and violence. "The problems are very many. Men don’t want to pay. Someone uses you but he does not want to pay. We are being beaten, and there's a lot of stress and competition." "There is a lot of competition between sex workers. Sometimes you go on the streets and no man is going to buy you and you end up not earning a single coin. Other times, when that man buys you, he tells you the money, you negotiate when you go to the lodge the man does not pay you. That is the most hard thing because you need to feed your children, but someone does not pay you. The men beat us when we are in the lodges. They are rough, they don’t want to use condoms, you tell him to use a condom, and he does not want to use a condom. So they end up infecting you sometimes. My other sex workers most of them got infected through that. We are even being raped by policemen sometimes. They come on the streets to chase us away and if we stay on the streets to work, the policemen force you. When a policeman arrests you, he takes you to a police station because you don’t have money. He asks what you can offer if you want to leave jail. You will say, "I have nothing I don’t have money." So the only thing you can do is to have sex with him. Then he will release you. Women cells are not the same as the ones for men - sometimes you are there alone at night. So police cells are being used to rape women. He has not paid you so that is rape - he has just forced you. There are many women who got pregnant because of this rape. Even me. I have had two abortions." Joanne used local herbs to terminate her pregnancy which led to complications. Then her friend told her about Lady Mermaid's Bureau and they referred her to IPPF's Reproductive Health Uganda (RHU) who were able to help her. Since being involved with Lady Mermaid's Bureau Joanne has been taught English and computer skills and has also got access to contraception and legal support. She thinks that both sex-work and abortion should be legalised in Uganda to reduce the stigma that leads to violence and abuse. "At times men don't respect us as sex-workers. Because it is illegal they abuse you. If they legalise it, it will be good." Stories Read more stories about the amazing success of SAAF in Uganda
| 19 April 2024
Sex workers in Uganda find hope
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Lady Mermaid's Bureau. Joanne is a sex-worker who has been involved in the project run by Lady Mermaid's Bureau, funded by SAAF. "My name is Joanne, I have been a sex-worker for two years." Joanne was abused as a child and became pregnant at a very young age. She was forced to leave school with only a primary education and could not speak English very well. When she moved to Kampala from her village she was told she could get a good job but she had nowhere to stay and ended up becoming a sex-worker in order to support herself and her two children. While sex-work offers some financial support, the fact that it is illegal and that gender inequality is high in Uganda make sex workers very vulnerable to rape and violence. "The problems are very many. Men don’t want to pay. Someone uses you but he does not want to pay. We are being beaten, and there's a lot of stress and competition." "There is a lot of competition between sex workers. Sometimes you go on the streets and no man is going to buy you and you end up not earning a single coin. Other times, when that man buys you, he tells you the money, you negotiate when you go to the lodge the man does not pay you. That is the most hard thing because you need to feed your children, but someone does not pay you. The men beat us when we are in the lodges. They are rough, they don’t want to use condoms, you tell him to use a condom, and he does not want to use a condom. So they end up infecting you sometimes. My other sex workers most of them got infected through that. We are even being raped by policemen sometimes. They come on the streets to chase us away and if we stay on the streets to work, the policemen force you. When a policeman arrests you, he takes you to a police station because you don’t have money. He asks what you can offer if you want to leave jail. You will say, "I have nothing I don’t have money." So the only thing you can do is to have sex with him. Then he will release you. Women cells are not the same as the ones for men - sometimes you are there alone at night. So police cells are being used to rape women. He has not paid you so that is rape - he has just forced you. There are many women who got pregnant because of this rape. Even me. I have had two abortions." Joanne used local herbs to terminate her pregnancy which led to complications. Then her friend told her about Lady Mermaid's Bureau and they referred her to IPPF's Reproductive Health Uganda (RHU) who were able to help her. Since being involved with Lady Mermaid's Bureau Joanne has been taught English and computer skills and has also got access to contraception and legal support. She thinks that both sex-work and abortion should be legalised in Uganda to reduce the stigma that leads to violence and abuse. "At times men don't respect us as sex-workers. Because it is illegal they abuse you. If they legalise it, it will be good." Stories Read more stories about the amazing success of SAAF in Uganda

| 04 April 2017
Help across the generations
Cyclone Winston, which devastated Fiji, was the strongest to ever hit the South Pacific. IPPF’s humanitarian response there was carried out with our Member Association, the Reproductive Family Health Association of Fiji, and is part of our SPRINT Initiative, funded by the Australian Government. My name is Atunaisa Rayasi. I am 65-years-old and I live in the village of Natalecake, with my son, daughter-in-law and their three children. During the storm the branch of the mango tree broke off and it hit the roof which was damaged. The roof stayed intact but was damaged so everything got drenched. The children were really scared. In my room the roofing iron came out and blew away. We can still see the watermark over there on the wall, where a dark patch marks out the spot where the rains hit. Even though the house was badly damaged, I actually found it far more difficult later, when I wanted to get to the hospital to see a doctor. After the cyclone, the road to the hospital was destroyed completely. We only got to the hospital after three weeks. I had to ask my son to get a car. There were so many other people there. I had to sit in a queue and wait for my number to be called up. You get there in the morning and the number gets called at 2pm. I am not able to leave home often, so I wasn't amongst those in the village hall when the NGOs (non-governmental organisations) came around. My daughter-in-law, who was pregnant at the time, received assistance from IPPF. She got some help with the buckets which helped the whole family. We were able to store fresh drinking water inside. Stories Read more stories about our work in Fiji after the Cyclone Winston

| 19 April 2024
Help across the generations
Cyclone Winston, which devastated Fiji, was the strongest to ever hit the South Pacific. IPPF’s humanitarian response there was carried out with our Member Association, the Reproductive Family Health Association of Fiji, and is part of our SPRINT Initiative, funded by the Australian Government. My name is Atunaisa Rayasi. I am 65-years-old and I live in the village of Natalecake, with my son, daughter-in-law and their three children. During the storm the branch of the mango tree broke off and it hit the roof which was damaged. The roof stayed intact but was damaged so everything got drenched. The children were really scared. In my room the roofing iron came out and blew away. We can still see the watermark over there on the wall, where a dark patch marks out the spot where the rains hit. Even though the house was badly damaged, I actually found it far more difficult later, when I wanted to get to the hospital to see a doctor. After the cyclone, the road to the hospital was destroyed completely. We only got to the hospital after three weeks. I had to ask my son to get a car. There were so many other people there. I had to sit in a queue and wait for my number to be called up. You get there in the morning and the number gets called at 2pm. I am not able to leave home often, so I wasn't amongst those in the village hall when the NGOs (non-governmental organisations) came around. My daughter-in-law, who was pregnant at the time, received assistance from IPPF. She got some help with the buckets which helped the whole family. We were able to store fresh drinking water inside. Stories Read more stories about our work in Fiji after the Cyclone Winston

| 05 March 2017
Forced into marriage at 16
High up in the mountains of Rasuwa in northern Nepal, close to the Tibetan border, is the village of Gatlang. This tight-knit village of traditional stone houses and Buddhist stupas is home to the Tamang people: a Buddhist indigenous group for whom family life is strictly patriarchal. Marriage traditions here can be oppressive: when a man chooses a wife, the girls – many are as young as 14 – have little choice but to marry. Most then go on to have large families, meaning food, money and education are spread sparsely. Jomini Tamang was just 16 years old when her parents forced her to marry. “I don’t want to get married,” she told them, but the wedding went ahead anyway. Jomini lives in Gatlang, a remote village of traditional stone and carved wooden houses, high up in the mountains of northern Nepal, close to the Tibetan border. The people here are Tamang, a Buddhist ethnic group, and family life is strictly patriarchal. Many Tamang marry young – from around 14 years old – and girls tend to be pushed into marriage by both their parents and the young men who choose them. “It’s not easy being married, it’s difficult,” says Jomini, whose husband is eight years older than her. “When I got married, I didn’t know anything about what happens after marriage, about the physical side.” After a year of marriage, Jomini had her first child, a boy called Gauran, who is now two. Women like Jomini are expected to combine childcare with household chores and long shifts farming vegetables in the village fields. “After the birth, I had many difficulties. Bringing up a child in this remote village was frightening and challenging, and Gauran was ill a lot". Giving birth at a young age can lead to severe physical complications or death, and maternal mortality is one of the leading causes of death for women in Nepal. Only 60% of women receive skilled antenatal support. Luckily for Jomini, shortly after Gauran’s birth, the Family Planning Association of Nepal (FPAN), Nepal’s leading family planning NGO, stepped in to help. Jomini met Pasang Tamang, a local woman who works as a reproductive health female volunteer for FPAN. Through Pasang, Jomini learned about different contraceptive methods and, with careful advice and support, was able to think through which might be best for her. She opted for the contraceptive injection, and says she is much happier now: contraception has given her more freedom, and the space to think clearly about when to have another child. Jomini’s experiences have convinced her to do everything possible to enable her children to live happier lives, less constrained by patriarchy and marriage. If she has a daughter, “I will tell her not to get married at an early age like her mum, and that if she does, she will suffer,” she says. “I will advise her to study more so she can work.” “And I will advise my son the same! Study more and wait til you are more mature to get married.” Stories Read more stories from Nepal

| 19 April 2024
Forced into marriage at 16
High up in the mountains of Rasuwa in northern Nepal, close to the Tibetan border, is the village of Gatlang. This tight-knit village of traditional stone houses and Buddhist stupas is home to the Tamang people: a Buddhist indigenous group for whom family life is strictly patriarchal. Marriage traditions here can be oppressive: when a man chooses a wife, the girls – many are as young as 14 – have little choice but to marry. Most then go on to have large families, meaning food, money and education are spread sparsely. Jomini Tamang was just 16 years old when her parents forced her to marry. “I don’t want to get married,” she told them, but the wedding went ahead anyway. Jomini lives in Gatlang, a remote village of traditional stone and carved wooden houses, high up in the mountains of northern Nepal, close to the Tibetan border. The people here are Tamang, a Buddhist ethnic group, and family life is strictly patriarchal. Many Tamang marry young – from around 14 years old – and girls tend to be pushed into marriage by both their parents and the young men who choose them. “It’s not easy being married, it’s difficult,” says Jomini, whose husband is eight years older than her. “When I got married, I didn’t know anything about what happens after marriage, about the physical side.” After a year of marriage, Jomini had her first child, a boy called Gauran, who is now two. Women like Jomini are expected to combine childcare with household chores and long shifts farming vegetables in the village fields. “After the birth, I had many difficulties. Bringing up a child in this remote village was frightening and challenging, and Gauran was ill a lot". Giving birth at a young age can lead to severe physical complications or death, and maternal mortality is one of the leading causes of death for women in Nepal. Only 60% of women receive skilled antenatal support. Luckily for Jomini, shortly after Gauran’s birth, the Family Planning Association of Nepal (FPAN), Nepal’s leading family planning NGO, stepped in to help. Jomini met Pasang Tamang, a local woman who works as a reproductive health female volunteer for FPAN. Through Pasang, Jomini learned about different contraceptive methods and, with careful advice and support, was able to think through which might be best for her. She opted for the contraceptive injection, and says she is much happier now: contraception has given her more freedom, and the space to think clearly about when to have another child. Jomini’s experiences have convinced her to do everything possible to enable her children to live happier lives, less constrained by patriarchy and marriage. If she has a daughter, “I will tell her not to get married at an early age like her mum, and that if she does, she will suffer,” she says. “I will advise her to study more so she can work.” “And I will advise my son the same! Study more and wait til you are more mature to get married.” Stories Read more stories from Nepal
| 15 October 2016
Living with HIV and HPV - a grandmother's tale
Christine is a 45-year-old grandmother who has HIV. She has been on antiretroviral treatment since 2005 and was widowed in 2006. She thinks her husband died of an HIV-related infection. “I heard on the radio that for people living positively it was a serious risk for us to get cervical cancer. During the announcements they mentioned some of the signs of cervical cancer like bad smell and so many signs. “I was having signs of discharge and very bad smell,” she said. She needed a smear to check for cervical cancer but getting one in rural Uganda wasn’t easy because money was tight and there were few gynaecologists available. “I tried in TASO Uganda, I failed. I went to Lachor Hospital, I never got satisfied. “Early in 2013, I heard over the radio about the services being offered by Reproductive Health Uganda. I went to their service centre and I was examined for cervical cancer and I tested positive. I got services from that centre. Last August, when I went for my control, they found that I’m free of cervical cancer,” said Christine. When she went for the smear for cervical cancer at Gulu Clinic she was also tested for human papilloma virus (HPV). Today Christine is visited by two people at her thatched hut home four kilometres away from Gulu Clinic. It is part of the routine follow-up for patients. From first appearance, it is hard to believe that this grandmother of one is living with HIV until she tells you that she is living positively. In her hut, the portrait of her late husband is displayed on the wall. Smartly dressed in a white and black coloured long dress, Christine said she had seen many friends that had died of cervical cancer. “Gulu Clinic has changed my life completely because of the way they handle their clients. And we got the service at a lower cost than at other health centres." Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE
| 19 April 2024
Living with HIV and HPV - a grandmother's tale
Christine is a 45-year-old grandmother who has HIV. She has been on antiretroviral treatment since 2005 and was widowed in 2006. She thinks her husband died of an HIV-related infection. “I heard on the radio that for people living positively it was a serious risk for us to get cervical cancer. During the announcements they mentioned some of the signs of cervical cancer like bad smell and so many signs. “I was having signs of discharge and very bad smell,” she said. She needed a smear to check for cervical cancer but getting one in rural Uganda wasn’t easy because money was tight and there were few gynaecologists available. “I tried in TASO Uganda, I failed. I went to Lachor Hospital, I never got satisfied. “Early in 2013, I heard over the radio about the services being offered by Reproductive Health Uganda. I went to their service centre and I was examined for cervical cancer and I tested positive. I got services from that centre. Last August, when I went for my control, they found that I’m free of cervical cancer,” said Christine. When she went for the smear for cervical cancer at Gulu Clinic she was also tested for human papilloma virus (HPV). Today Christine is visited by two people at her thatched hut home four kilometres away from Gulu Clinic. It is part of the routine follow-up for patients. From first appearance, it is hard to believe that this grandmother of one is living with HIV until she tells you that she is living positively. In her hut, the portrait of her late husband is displayed on the wall. Smartly dressed in a white and black coloured long dress, Christine said she had seen many friends that had died of cervical cancer. “Gulu Clinic has changed my life completely because of the way they handle their clients. And we got the service at a lower cost than at other health centres." Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE

| 04 May 2017
In the eye of the storm
Cyclone Winston, which devastated Fiji, was the strongest to ever hit the South Pacific. IPPF’s humanitarian response there was carried out with our Member Association, the Reproductive & Family Health Association of Fiji, and is part of our SPRINT Initiative, funded by the Australian Government. My name is Verenaisi Katerina. I have five children and we live in a remote village in the Ba Highlands. At the time the cyclone hit we were all living in a timber house and I was pregnant. I’ve lived in a bure (traditional timber house with a thatched grass roof) all my life, I’m so used to living in a bure, I’m not used to living in a tin-roofed house. We tried to be prepared when the cyclone came. But we had to all rush to the evacuation centre when the roof blew off our house. My whole family was scared, our house was flooded and our crops were all damaged. My daughter was covering her eyes and ears and crying for help. While I started preparing to move to the local school to take shelter, my husband went to get us some food. I was really, really afraid. I was so worried about my kids. I told my husband not to be late and to help me out with the kids going down to the school. In the end, I managed to get my children to the school on my own, and my husband joined us later. While my family took shelter, lots of other homes in Navala were destroyed. We were lucky: most of their possessions were blown away, but some managed to survive, and our home was damaged, but remained standing. When we came back the next day, my husband tried to start repairing the kitchen so that we could move back. We had a small stove that we were using, and we made a small kitchen so at least we could cook. My husband could only get us what was left over from the farm and that’s basically what we were living on. We had to eat a lot of flour products, a lot of rice, because our farm was badly damaged. I received a dignity kit from IPPF and found it extremely helpful, particularly in clothing my children and the baby. Some of it was worn on the very same day we received it. I later took part in a family planning session conducted by IPPF. I learned a lot from the workshop on that day. I told myself, this is it. I’m only going to have five kids. Having to go through that experience of Cyclone Winston, if I had more children, then it might have been more difficult, too late, for me to run up to that school for shelter. I have had a talk with my husband and we have decided that this one is my last. My fifth is my last. Stories Read more stories about our work in Fiji after the Cyclone Winston

| 19 April 2024
In the eye of the storm
Cyclone Winston, which devastated Fiji, was the strongest to ever hit the South Pacific. IPPF’s humanitarian response there was carried out with our Member Association, the Reproductive & Family Health Association of Fiji, and is part of our SPRINT Initiative, funded by the Australian Government. My name is Verenaisi Katerina. I have five children and we live in a remote village in the Ba Highlands. At the time the cyclone hit we were all living in a timber house and I was pregnant. I’ve lived in a bure (traditional timber house with a thatched grass roof) all my life, I’m so used to living in a bure, I’m not used to living in a tin-roofed house. We tried to be prepared when the cyclone came. But we had to all rush to the evacuation centre when the roof blew off our house. My whole family was scared, our house was flooded and our crops were all damaged. My daughter was covering her eyes and ears and crying for help. While I started preparing to move to the local school to take shelter, my husband went to get us some food. I was really, really afraid. I was so worried about my kids. I told my husband not to be late and to help me out with the kids going down to the school. In the end, I managed to get my children to the school on my own, and my husband joined us later. While my family took shelter, lots of other homes in Navala were destroyed. We were lucky: most of their possessions were blown away, but some managed to survive, and our home was damaged, but remained standing. When we came back the next day, my husband tried to start repairing the kitchen so that we could move back. We had a small stove that we were using, and we made a small kitchen so at least we could cook. My husband could only get us what was left over from the farm and that’s basically what we were living on. We had to eat a lot of flour products, a lot of rice, because our farm was badly damaged. I received a dignity kit from IPPF and found it extremely helpful, particularly in clothing my children and the baby. Some of it was worn on the very same day we received it. I later took part in a family planning session conducted by IPPF. I learned a lot from the workshop on that day. I told myself, this is it. I’m only going to have five kids. Having to go through that experience of Cyclone Winston, if I had more children, then it might have been more difficult, too late, for me to run up to that school for shelter. I have had a talk with my husband and we have decided that this one is my last. My fifth is my last. Stories Read more stories about our work in Fiji after the Cyclone Winston

| 04 May 2017
Starting again in Fiji
Cyclone Winston, which devastated Fiji, was the strongest to ever hit the South Pacific. IPPF’s humanitarian response there was carried out with our Member Association, the Reproductive & Family Health Association of Fiji, and is part of our SPRINT Initiative, funded by the Australian Government. 22-year-old Sulueti arrived in the village one week after the cyclone was over. She was shocked - there was nothing left apart from the foundation of the house apart from that everything was gone. She hadn't expected it to be so bad. Her 59-year-old mother, had been sick and alone during the cyclone and she was traumatised as had never experienced a storm like that before. They tried slowly to start rebuilding a small house for them to move back into and out of the community hall. It was a difficult time because Sulueti was four-months pregnant. She managed to see a doctor three times while staying in the community hall, but there were no proper examinations or ultrasounds during this time. The delivery was fine in a maternity hospital. She received a dignity kit from IPPF and received baby supplies for post-delivery, everything that was required for a new mother to care for a baby was in the kit. IPPF went to visit her in her home and gave advice on family planning - she is taking injectables now because she doesn’t want any more children. Stories Read more stories about our work in Fiji after the Cyclone Winston

| 19 April 2024
Starting again in Fiji
Cyclone Winston, which devastated Fiji, was the strongest to ever hit the South Pacific. IPPF’s humanitarian response there was carried out with our Member Association, the Reproductive & Family Health Association of Fiji, and is part of our SPRINT Initiative, funded by the Australian Government. 22-year-old Sulueti arrived in the village one week after the cyclone was over. She was shocked - there was nothing left apart from the foundation of the house apart from that everything was gone. She hadn't expected it to be so bad. Her 59-year-old mother, had been sick and alone during the cyclone and she was traumatised as had never experienced a storm like that before. They tried slowly to start rebuilding a small house for them to move back into and out of the community hall. It was a difficult time because Sulueti was four-months pregnant. She managed to see a doctor three times while staying in the community hall, but there were no proper examinations or ultrasounds during this time. The delivery was fine in a maternity hospital. She received a dignity kit from IPPF and received baby supplies for post-delivery, everything that was required for a new mother to care for a baby was in the kit. IPPF went to visit her in her home and gave advice on family planning - she is taking injectables now because she doesn’t want any more children. Stories Read more stories about our work in Fiji after the Cyclone Winston
| 20 April 2017
Sex workers in Uganda find hope
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Lady Mermaid's Bureau. Joanne is a sex-worker who has been involved in the project run by Lady Mermaid's Bureau, funded by SAAF. "My name is Joanne, I have been a sex-worker for two years." Joanne was abused as a child and became pregnant at a very young age. She was forced to leave school with only a primary education and could not speak English very well. When she moved to Kampala from her village she was told she could get a good job but she had nowhere to stay and ended up becoming a sex-worker in order to support herself and her two children. While sex-work offers some financial support, the fact that it is illegal and that gender inequality is high in Uganda make sex workers very vulnerable to rape and violence. "The problems are very many. Men don’t want to pay. Someone uses you but he does not want to pay. We are being beaten, and there's a lot of stress and competition." "There is a lot of competition between sex workers. Sometimes you go on the streets and no man is going to buy you and you end up not earning a single coin. Other times, when that man buys you, he tells you the money, you negotiate when you go to the lodge the man does not pay you. That is the most hard thing because you need to feed your children, but someone does not pay you. The men beat us when we are in the lodges. They are rough, they don’t want to use condoms, you tell him to use a condom, and he does not want to use a condom. So they end up infecting you sometimes. My other sex workers most of them got infected through that. We are even being raped by policemen sometimes. They come on the streets to chase us away and if we stay on the streets to work, the policemen force you. When a policeman arrests you, he takes you to a police station because you don’t have money. He asks what you can offer if you want to leave jail. You will say, "I have nothing I don’t have money." So the only thing you can do is to have sex with him. Then he will release you. Women cells are not the same as the ones for men - sometimes you are there alone at night. So police cells are being used to rape women. He has not paid you so that is rape - he has just forced you. There are many women who got pregnant because of this rape. Even me. I have had two abortions." Joanne used local herbs to terminate her pregnancy which led to complications. Then her friend told her about Lady Mermaid's Bureau and they referred her to IPPF's Reproductive Health Uganda (RHU) who were able to help her. Since being involved with Lady Mermaid's Bureau Joanne has been taught English and computer skills and has also got access to contraception and legal support. She thinks that both sex-work and abortion should be legalised in Uganda to reduce the stigma that leads to violence and abuse. "At times men don't respect us as sex-workers. Because it is illegal they abuse you. If they legalise it, it will be good." Stories Read more stories about the amazing success of SAAF in Uganda
| 19 April 2024
Sex workers in Uganda find hope
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Lady Mermaid's Bureau. Joanne is a sex-worker who has been involved in the project run by Lady Mermaid's Bureau, funded by SAAF. "My name is Joanne, I have been a sex-worker for two years." Joanne was abused as a child and became pregnant at a very young age. She was forced to leave school with only a primary education and could not speak English very well. When she moved to Kampala from her village she was told she could get a good job but she had nowhere to stay and ended up becoming a sex-worker in order to support herself and her two children. While sex-work offers some financial support, the fact that it is illegal and that gender inequality is high in Uganda make sex workers very vulnerable to rape and violence. "The problems are very many. Men don’t want to pay. Someone uses you but he does not want to pay. We are being beaten, and there's a lot of stress and competition." "There is a lot of competition between sex workers. Sometimes you go on the streets and no man is going to buy you and you end up not earning a single coin. Other times, when that man buys you, he tells you the money, you negotiate when you go to the lodge the man does not pay you. That is the most hard thing because you need to feed your children, but someone does not pay you. The men beat us when we are in the lodges. They are rough, they don’t want to use condoms, you tell him to use a condom, and he does not want to use a condom. So they end up infecting you sometimes. My other sex workers most of them got infected through that. We are even being raped by policemen sometimes. They come on the streets to chase us away and if we stay on the streets to work, the policemen force you. When a policeman arrests you, he takes you to a police station because you don’t have money. He asks what you can offer if you want to leave jail. You will say, "I have nothing I don’t have money." So the only thing you can do is to have sex with him. Then he will release you. Women cells are not the same as the ones for men - sometimes you are there alone at night. So police cells are being used to rape women. He has not paid you so that is rape - he has just forced you. There are many women who got pregnant because of this rape. Even me. I have had two abortions." Joanne used local herbs to terminate her pregnancy which led to complications. Then her friend told her about Lady Mermaid's Bureau and they referred her to IPPF's Reproductive Health Uganda (RHU) who were able to help her. Since being involved with Lady Mermaid's Bureau Joanne has been taught English and computer skills and has also got access to contraception and legal support. She thinks that both sex-work and abortion should be legalised in Uganda to reduce the stigma that leads to violence and abuse. "At times men don't respect us as sex-workers. Because it is illegal they abuse you. If they legalise it, it will be good." Stories Read more stories about the amazing success of SAAF in Uganda

| 04 April 2017
Help across the generations
Cyclone Winston, which devastated Fiji, was the strongest to ever hit the South Pacific. IPPF’s humanitarian response there was carried out with our Member Association, the Reproductive Family Health Association of Fiji, and is part of our SPRINT Initiative, funded by the Australian Government. My name is Atunaisa Rayasi. I am 65-years-old and I live in the village of Natalecake, with my son, daughter-in-law and their three children. During the storm the branch of the mango tree broke off and it hit the roof which was damaged. The roof stayed intact but was damaged so everything got drenched. The children were really scared. In my room the roofing iron came out and blew away. We can still see the watermark over there on the wall, where a dark patch marks out the spot where the rains hit. Even though the house was badly damaged, I actually found it far more difficult later, when I wanted to get to the hospital to see a doctor. After the cyclone, the road to the hospital was destroyed completely. We only got to the hospital after three weeks. I had to ask my son to get a car. There were so many other people there. I had to sit in a queue and wait for my number to be called up. You get there in the morning and the number gets called at 2pm. I am not able to leave home often, so I wasn't amongst those in the village hall when the NGOs (non-governmental organisations) came around. My daughter-in-law, who was pregnant at the time, received assistance from IPPF. She got some help with the buckets which helped the whole family. We were able to store fresh drinking water inside. Stories Read more stories about our work in Fiji after the Cyclone Winston

| 19 April 2024
Help across the generations
Cyclone Winston, which devastated Fiji, was the strongest to ever hit the South Pacific. IPPF’s humanitarian response there was carried out with our Member Association, the Reproductive Family Health Association of Fiji, and is part of our SPRINT Initiative, funded by the Australian Government. My name is Atunaisa Rayasi. I am 65-years-old and I live in the village of Natalecake, with my son, daughter-in-law and their three children. During the storm the branch of the mango tree broke off and it hit the roof which was damaged. The roof stayed intact but was damaged so everything got drenched. The children were really scared. In my room the roofing iron came out and blew away. We can still see the watermark over there on the wall, where a dark patch marks out the spot where the rains hit. Even though the house was badly damaged, I actually found it far more difficult later, when I wanted to get to the hospital to see a doctor. After the cyclone, the road to the hospital was destroyed completely. We only got to the hospital after three weeks. I had to ask my son to get a car. There were so many other people there. I had to sit in a queue and wait for my number to be called up. You get there in the morning and the number gets called at 2pm. I am not able to leave home often, so I wasn't amongst those in the village hall when the NGOs (non-governmental organisations) came around. My daughter-in-law, who was pregnant at the time, received assistance from IPPF. She got some help with the buckets which helped the whole family. We were able to store fresh drinking water inside. Stories Read more stories about our work in Fiji after the Cyclone Winston

| 05 March 2017
Forced into marriage at 16
High up in the mountains of Rasuwa in northern Nepal, close to the Tibetan border, is the village of Gatlang. This tight-knit village of traditional stone houses and Buddhist stupas is home to the Tamang people: a Buddhist indigenous group for whom family life is strictly patriarchal. Marriage traditions here can be oppressive: when a man chooses a wife, the girls – many are as young as 14 – have little choice but to marry. Most then go on to have large families, meaning food, money and education are spread sparsely. Jomini Tamang was just 16 years old when her parents forced her to marry. “I don’t want to get married,” she told them, but the wedding went ahead anyway. Jomini lives in Gatlang, a remote village of traditional stone and carved wooden houses, high up in the mountains of northern Nepal, close to the Tibetan border. The people here are Tamang, a Buddhist ethnic group, and family life is strictly patriarchal. Many Tamang marry young – from around 14 years old – and girls tend to be pushed into marriage by both their parents and the young men who choose them. “It’s not easy being married, it’s difficult,” says Jomini, whose husband is eight years older than her. “When I got married, I didn’t know anything about what happens after marriage, about the physical side.” After a year of marriage, Jomini had her first child, a boy called Gauran, who is now two. Women like Jomini are expected to combine childcare with household chores and long shifts farming vegetables in the village fields. “After the birth, I had many difficulties. Bringing up a child in this remote village was frightening and challenging, and Gauran was ill a lot". Giving birth at a young age can lead to severe physical complications or death, and maternal mortality is one of the leading causes of death for women in Nepal. Only 60% of women receive skilled antenatal support. Luckily for Jomini, shortly after Gauran’s birth, the Family Planning Association of Nepal (FPAN), Nepal’s leading family planning NGO, stepped in to help. Jomini met Pasang Tamang, a local woman who works as a reproductive health female volunteer for FPAN. Through Pasang, Jomini learned about different contraceptive methods and, with careful advice and support, was able to think through which might be best for her. She opted for the contraceptive injection, and says she is much happier now: contraception has given her more freedom, and the space to think clearly about when to have another child. Jomini’s experiences have convinced her to do everything possible to enable her children to live happier lives, less constrained by patriarchy and marriage. If she has a daughter, “I will tell her not to get married at an early age like her mum, and that if she does, she will suffer,” she says. “I will advise her to study more so she can work.” “And I will advise my son the same! Study more and wait til you are more mature to get married.” Stories Read more stories from Nepal

| 19 April 2024
Forced into marriage at 16
High up in the mountains of Rasuwa in northern Nepal, close to the Tibetan border, is the village of Gatlang. This tight-knit village of traditional stone houses and Buddhist stupas is home to the Tamang people: a Buddhist indigenous group for whom family life is strictly patriarchal. Marriage traditions here can be oppressive: when a man chooses a wife, the girls – many are as young as 14 – have little choice but to marry. Most then go on to have large families, meaning food, money and education are spread sparsely. Jomini Tamang was just 16 years old when her parents forced her to marry. “I don’t want to get married,” she told them, but the wedding went ahead anyway. Jomini lives in Gatlang, a remote village of traditional stone and carved wooden houses, high up in the mountains of northern Nepal, close to the Tibetan border. The people here are Tamang, a Buddhist ethnic group, and family life is strictly patriarchal. Many Tamang marry young – from around 14 years old – and girls tend to be pushed into marriage by both their parents and the young men who choose them. “It’s not easy being married, it’s difficult,” says Jomini, whose husband is eight years older than her. “When I got married, I didn’t know anything about what happens after marriage, about the physical side.” After a year of marriage, Jomini had her first child, a boy called Gauran, who is now two. Women like Jomini are expected to combine childcare with household chores and long shifts farming vegetables in the village fields. “After the birth, I had many difficulties. Bringing up a child in this remote village was frightening and challenging, and Gauran was ill a lot". Giving birth at a young age can lead to severe physical complications or death, and maternal mortality is one of the leading causes of death for women in Nepal. Only 60% of women receive skilled antenatal support. Luckily for Jomini, shortly after Gauran’s birth, the Family Planning Association of Nepal (FPAN), Nepal’s leading family planning NGO, stepped in to help. Jomini met Pasang Tamang, a local woman who works as a reproductive health female volunteer for FPAN. Through Pasang, Jomini learned about different contraceptive methods and, with careful advice and support, was able to think through which might be best for her. She opted for the contraceptive injection, and says she is much happier now: contraception has given her more freedom, and the space to think clearly about when to have another child. Jomini’s experiences have convinced her to do everything possible to enable her children to live happier lives, less constrained by patriarchy and marriage. If she has a daughter, “I will tell her not to get married at an early age like her mum, and that if she does, she will suffer,” she says. “I will advise her to study more so she can work.” “And I will advise my son the same! Study more and wait til you are more mature to get married.” Stories Read more stories from Nepal
| 15 October 2016
Living with HIV and HPV - a grandmother's tale
Christine is a 45-year-old grandmother who has HIV. She has been on antiretroviral treatment since 2005 and was widowed in 2006. She thinks her husband died of an HIV-related infection. “I heard on the radio that for people living positively it was a serious risk for us to get cervical cancer. During the announcements they mentioned some of the signs of cervical cancer like bad smell and so many signs. “I was having signs of discharge and very bad smell,” she said. She needed a smear to check for cervical cancer but getting one in rural Uganda wasn’t easy because money was tight and there were few gynaecologists available. “I tried in TASO Uganda, I failed. I went to Lachor Hospital, I never got satisfied. “Early in 2013, I heard over the radio about the services being offered by Reproductive Health Uganda. I went to their service centre and I was examined for cervical cancer and I tested positive. I got services from that centre. Last August, when I went for my control, they found that I’m free of cervical cancer,” said Christine. When she went for the smear for cervical cancer at Gulu Clinic she was also tested for human papilloma virus (HPV). Today Christine is visited by two people at her thatched hut home four kilometres away from Gulu Clinic. It is part of the routine follow-up for patients. From first appearance, it is hard to believe that this grandmother of one is living with HIV until she tells you that she is living positively. In her hut, the portrait of her late husband is displayed on the wall. Smartly dressed in a white and black coloured long dress, Christine said she had seen many friends that had died of cervical cancer. “Gulu Clinic has changed my life completely because of the way they handle their clients. And we got the service at a lower cost than at other health centres." Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE
| 19 April 2024
Living with HIV and HPV - a grandmother's tale
Christine is a 45-year-old grandmother who has HIV. She has been on antiretroviral treatment since 2005 and was widowed in 2006. She thinks her husband died of an HIV-related infection. “I heard on the radio that for people living positively it was a serious risk for us to get cervical cancer. During the announcements they mentioned some of the signs of cervical cancer like bad smell and so many signs. “I was having signs of discharge and very bad smell,” she said. She needed a smear to check for cervical cancer but getting one in rural Uganda wasn’t easy because money was tight and there were few gynaecologists available. “I tried in TASO Uganda, I failed. I went to Lachor Hospital, I never got satisfied. “Early in 2013, I heard over the radio about the services being offered by Reproductive Health Uganda. I went to their service centre and I was examined for cervical cancer and I tested positive. I got services from that centre. Last August, when I went for my control, they found that I’m free of cervical cancer,” said Christine. When she went for the smear for cervical cancer at Gulu Clinic she was also tested for human papilloma virus (HPV). Today Christine is visited by two people at her thatched hut home four kilometres away from Gulu Clinic. It is part of the routine follow-up for patients. From first appearance, it is hard to believe that this grandmother of one is living with HIV until she tells you that she is living positively. In her hut, the portrait of her late husband is displayed on the wall. Smartly dressed in a white and black coloured long dress, Christine said she had seen many friends that had died of cervical cancer. “Gulu Clinic has changed my life completely because of the way they handle their clients. And we got the service at a lower cost than at other health centres." Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE