This page was originally published in 2012 and has since been updated.
Myth: Abortion
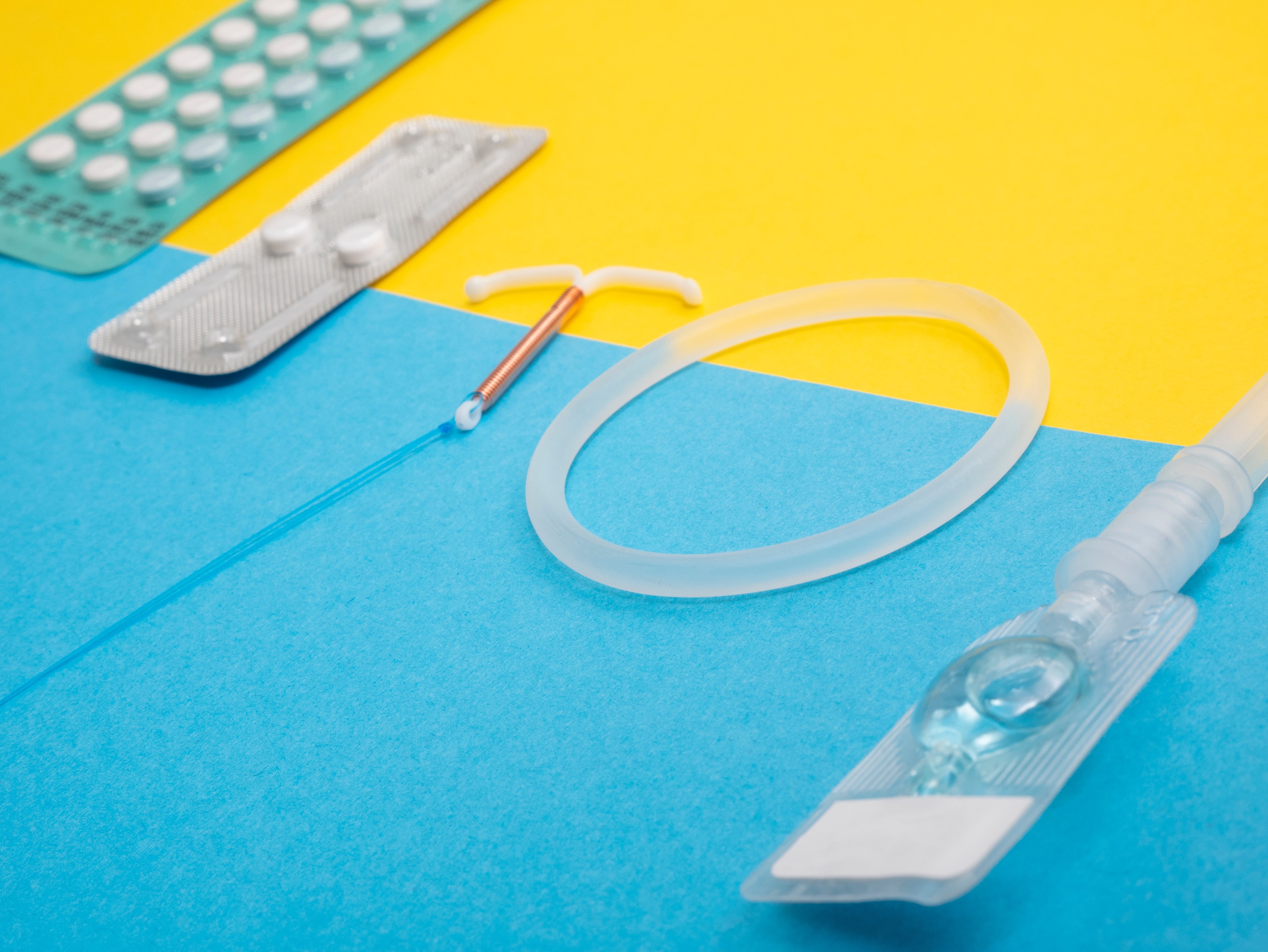
Some couples do not want to use the IUD because they incorrectly believe that the IUD prevents pregnancy by causing abortions.
Fact: IUDs do not work by causing abortions
In the vast majority of cases, IUDs work by preventing fertilization. The copper-bearing IUD acts as a spermicide, killing or impairing sperm so they cannot reach the egg. IUDs that contain progestin cause the cervical mucus to thicken, which stops sperm from entering the uterus. Thus, the current evidence suggests that the main mechanisms of action of IUDs occur prior to fertilization. In very rare case, IUDs prevent implantation which is considered a contraceptive not an abortifacient effect.
Myth: Effectiveness
Some women do not want to use the IUD because they incorrectly believe that the IUD is not effective in preventing pregnancy or that the IUD loses its contraceptive effect after only a few years from the time of insertion.
Fact: IUDs are the more than 99% effective!
Both the hormonal and copper-bearing IUDs are highly effective contraceptive methods. In fact, they are among the most effective reversible methods, with pregnancy rates similar to those for female sterilization.
Hormonal levonorgestrel-releasing IUD (LNG-IUD): Less than 1 pregnancy per 100 women using the LNG-IUD over the first year (2 per 1,000 women). That means the LNG-IUD will prevent pregnancy in 998 of 1,000 women. A small risk of pregnancy remains beyond the first year of use and continues as long as the woman is using the LNG-IUD. Over 5 years of LNG-IUD use, about 1 per 100 women (5 to 8 per 1,000 women) will become pregnant. The LNG-IUD is approved for up to 5 years of use.
Copper-bearing IUDs: Less than 1 pregnancy per 100 women using an IUD over the first year (6 to 8 per 1,000 women). That means the IUD will prevent pregnancy for 992 to 994 of 1,000 women using IUDs will not become pregnant. A small risk of pregnancy remains beyond the first year of use and continues as long as the woman is using the IUD. Over 10 years of IUD use, about 2 per 100 women will become pregnant. The IUD is effective for up to 12 years.
Myth: Health risks and side effects
Some women do not want to use the IUD because they incorrectly believe that IUD causes side effects or health risks such as cancer, sexually transmitted infections, or birth defects.
Fact: IUDs are safe!
Infection related to IUD insertion probably occurs because the instruments or IUD carry with them organisms from the lower genital tract. If the organisms are bacteria normally present in the genital tract, then it seems that some mechanism automatically eliminates this contamination from the uterus soon after the insertion process without infection occurring. Risk of infection can be further reduced by following routine infection-prevention procedures including the “no-touch” insertion technique (not letting the loaded IUD or uterine sounds touch any unsterile surfaces such as hands, speculum, vaginal wall, or table top).
The IUD never travels to the heart, brain, or any other part of the body outside the abdomen. The IUD normally stays within the uterus like a seed within a shell. Rarely, the IUD may come through (perforate) the wall of the uterus into the abdominal cavity. This is most often due to a mistake during insertion. Proper insertion technique can help prevent many problems, such as infection, expulsion, and perforation. If uterine perforation is suspected within 6 weeks after insertion or if it is suspected later and is causing symptoms, refer the client for evaluation to a clinician experienced at removing such IUDs. Usually, however, the out-of-place IUD causes no problems and should be left where it is. The woman will need another contraceptive method.
IUDs do not cause cancer in otherwise healthy women, but confirmed or suspected cancer of the genital tract is a contraindication to IUD use, because the increased risk of infection, perforation, and bleeding at insertion may make the condition worse. For the levonorgestrel-releasing IUD, breast cancer is also a contraindication.
IUDs do not increase the risk of contracting STIs, including HIV. However, usually women who have a very high risk of exposure to gonorrhea or chlamydia should not have an IUD inserted. In special circumstances, when other, more appropriate methods are not available or acceptable to her, a qualified provider who can carefully assess a specific woman’s risk may decide that she can use an IUD.
IUD use neither causes multiple pregnancies after removal nor increases the risk of birth defects, whether the pregnancy occurs with the IUD in place, or after removal.
In the rare event that a client becomes pregnant with an IUD in situ, it is important to explain the risks of leaving the IUD in the uterus during pregnancy. There is a higher risk of preterm delivery or miscarriage, including infected (septic) miscarriage during the first or second trimester, which can be life-threatening. Early removal of the IUD reduces these risks, although the removal procedure itself involves a small risk of miscarriage. There is no evidence of increased risk of fetal malformations, however.
Overall levels of Pelvic Inflammatory Disease (PID) in IUD users are low. A woman with chlamydia or gonorrhea at the time of IUD insertion, however, is at higher risk of PID in the first few weeks after insertion than she is later. After the first few weeks, an STI may be no more likely to progress to PID in an IUD user than for other women with STIs. To reduce the risk of infection during IUD insertion, providers can ensure appropriate insertion conditions, screening, and counseling, as well as regularly monitor and treat infection.
Antibiotics are usually not routinely given before IUD insertion. Most recent research done where STIs are not common suggests that PID risk is low with or without antibiotics. When appropriate questions to screen for STI risk are asked and IUD insertion is done with proper infection-prevention procedures (including the no-touch insertion technique), there is little risk of infection. Antibiotics may be considered, however, in areas where STIs are common and STI screening is limited.
If PID occurs or is suspected with an IUD in place, treatment should be started as soon as possible. There is no need to remove the IUD if a woman wants to continue using it. The PID should be treated and the IUD left in situ. If a woman wants it removed, it can be taken out after starting antibiotic treatment. An IUD should not be inserted in women who currently have a PID. It may be inserted as soon as she finishes treatment, if she is not at risk for reinfection before insertion.
The copper in copper-bearing IUDs is not released into the blood. Levels of serum copper in long-term users of copper IUDs are similar to that of the normal population.
Myth: Problems after removal
Some couples do not want to use the IUD because they incorrectly believe that the IUD will cause infertility, ectopic pregnancy, or miscarriage.
Fact: no increased risk of infertility
Good studies find no increased risk of infertility among women who have used IUDs, including young women and women with no children. Whether or not a woman has an IUD, however, if she develops pelvic inflammatory disease (PID) and it is not treated, there is some chance that she will become infertile. PID can permanently damage the lining of the fallopian tubes and may partially or totally block one or both tubes enough to cause infertility.
Fact: no increased risk of ectopic pregnancy or miscarriage after removal
Because any pregnancy among IUD users is rare, ectopic pregnancy among IUD users is even rarer. An IUD does not increase a woman’s overall risk of ectopic pregnancy. In fact, an IUD user’s risk of an ectopic pregnancy is much lower than the risk to a woman who is not using any method of contraception. In the unlikely event of pregnancy in an IUD user, 6 to 8 in every 100 of these pregnancies is ectopic. Thus, the great majority of pregnancies after IUD failure are not ectopic. Still, ectopic pregnancy can be life-threatening, so a provider should be aware that ectopic pregnancy is possible if an IUD fails.
IUDs do not cause miscarriages after they have been removed. If correct insertion technique is used, the use of an IUD will not cause any difficulty in future pregnancies.
In the rare event that a client becomes pregnant with an IUD in situ, it is important to explain the risks of leaving the IUD in the uterus during pregnancy. There is a higher risk of preterm delivery or first- and second- trimester miscarriage, including infected (septic) miscarriage which can be life-threatening. Early removal of the IUD reduces these risks, although the removal procedure itself involves a small risk of miscarriage.
If the client does not want to continue the pregnancy and if therapeutic termination of pregnancy is legally available, inform her accordingly. If she wishes to continue the pregnancy and the IUD strings are visible or can be retrieved safely from the cervical canal, gently remove the IUD or refer for removal. The client should return at once if she develops any signs of miscarriage or septic miscarriage (vaginal bleeding, cramping, pain, abnormal vaginal discharge, or fever).
However, if the IUD strings cannot be found in the cervical canal and the IUD cannot be safely retrieved, refer for ultrasound, if possible, to determine whether the IUD is still in the uterus. If the IUD is still in the uterus, if ultrasound is not available, or if the client chooses to keep the IUD, her pregnancy should be followed closely by a nurse or doctor. She should see a nurse or doctor at once if she develops any signs of septic miscarriage.
Myth: change of menstrual pattern
Many couples do not want to use the IUD because they incorrectly believe that using the IUD will cause either no monthly bleeding (amenorrhea) or heavier, painful, and more frequent menstrual bleeding, and this is harmful for your system.
Fact: change in bleeding patterns are not harmful
Women can experience changes in bleeding patterns depending on the type of IUD.
Women using copper-bearing IUDs may experience:
- Heavy and prolonged monthly bleeding
- Irregular bleeding
- More cramps and pain during monthly bleeding
These bleeding changes are normal and usually are not signs of illness. They are most common in the first 3 to 6 months after insertion and usually lessen with time. A provider should evaluate for an underlying condition unrelated to method use if:
- Cramping continues and occurs between monthly bleeding;
- Heavy or prolonged bleeding continues, or if bleeding starts suddenly after several months of normal bleeding or long after the IUD was inserted, or;
- Irregular bleeding persists after 6 months, or starts suddenly after several months of normal bleeding.
Severe anaemia requires careful consideration because if heavier menstrual periods are experienced, the additional monthly blood loss could worsen existing anaemia. The anaemia should be treated before an IUD is inserted. The LNG-IUD may actually help to reduce anaemia by reducing blood loss.
Women using the LNG-IUD may experience heavy, prolonged, or irregular bleeding in the first few months, but then experience:
- Lighter, regular, and predictable bleeding
- Infrequent, light, or no monthly bleeding
These bleeding changes also are normal and usually are not signs of illness.
Copper-bearing IUDs rarely cause monthly bleeding to stop completely. However, women using an LNG-IUD may not experience monthly bleeding due to strong uniform suppression of the endometrium. If monthly bleeding does not occur while a woman is using a copper-bearing IUD, pregnancy should be excluded. If the woman is not pregnant, other causes of no monthly bleeding should be investigated.
Pain associated with menstruation may increase in some women, but usually this is only for the first month or two. The LNG-IUD may reduce the pain associated with menstruation. Non-steroidal anti-inflammatory drugs may also reduce discomfort.
Myth: Sexual desire and sexual pleasure
Some couples do not want to use the IUD because they incorrectly believe that the IUD will cause inconvenience during sex, pain for the male partner because the strings will hurt the penis, or that using the IUD causes discomfort and pain for the woman during sex.
Fact: It might make you more relaxed about unintended pregnancies and enjoy sex even more!
There is no reason why an IUD should negatively affect sexual pleasure. On the contrary, being free from fear of pregnancy may allow both partners, especially the woman, to enjoy their sexual life.
There is no reason why an IUD should cause discomfort or pain during sexual intercourse unless the woman is already having cramps, which sometimes occur during the first few weeks after insertion. Sexual intercourse cannot displace an IUD.
Sometimes a man can feel the strings if they are too long. If this bothers him, cutting the strings shorter should solve the problem. Sometimes a man can also feel discomfort if the strings are cut too short. To remedy the problem, the provider can cut them even shorter so they are not coming out of the cervical canal. The woman should be told beforehand, however, that this will mean she may not be able to feel the strings to check her IUD, and removing her IUD may be more difficult. Alternatively, she can have the IUD replaced with a new one and the strings cut to the correct length. The strings should be cut so that 3 centimeters hang out of the cervix. A man may feel discomfort during sex if the IUD has started to come out through the cervix. If a woman suspects this, she should see a doctor or nurse immediately. Proper counselling of the male partner may be appropriate.
Myth: Who can use the method
Many women do not want to use the IUD because they incorrectly believe that the IUD should not be used by women who are young or who have not had children.
Fact: IUDs are safe for a wide range of women
There is no minimum or maximum age requirement for using the IUD. An IUD should be removed after menopause has occurred — at least 12 months after her last monthly bleeding. There is also no requirement that a woman must have children to use the IUD. A history of pelvic infection or multiple sex partners (one indication that a woman is at high risk for STIs) make the choice of an IUD inappropriate for such women.
The myth that young women and women without children cannot use IUDs stems from fears about a higher risk of expulsion in these women and fears about a higher risk of infection in these women.
Expulsion is more likely in certain circumstances, such as young age at insertion (under 20 or 25 years old). Some studies also have found a higher rate of expulsion among women who have no children. The additional risk of expulsion, however, is not sufficient to deny IUDs to women in these circumstances, because the advantages of the IUD outweigh the risks of expulsion.
Women with current gonorrheal or chlamydial infection should not have an IUD inserted. Since laboratory STI tests usually are not available, World Health Organization guidance considers STI risk assessment and physical examination essential to safe use of IUDs, but not laboratory tests. Providers should not determine a woman’s STI risk based on her age or whether she has had children. Rather, the provider can discuss risky behaviors or situations in their communities that they think are most likely to expose women to STIs, for example having more than one sexual partner in the last three months without always using condoms. The client can think about whether such situations occurred recently (in the past 3 months or so).
when
Blog Series
Adolescent Health
Subject
Contraception, Comprehensive Sex Education