Australia is on track to be the first country in the world to eliminate cervical cancer by as early as 2028 to 2035. This can be achieved through a combination of HPV vaccination, screening and treatment of pre-cancers and invasive cancers. I have been privileged during these exciting times to represent Family Planning Alliance Australia (FPAA) on key National Cervical Screening Program committees and to act as the FPAA clinical spokesperson on cervical cancer prevention.
As former medical director of one of the FPAA member organisations, Family Planning New South Wales, I have also had the honour of supporting the provision of high-quality, evidence-based and equitable cervical screening services across its clinics as well as providing clinical support to its International Program. The FPNSW International Program has provided cervical screening training and policy support to countries including The Solomon Islands and Tuvalu, and most recently through the collaborative C4 Centre for Research Excellence project Elimination of Cervical Cancer in the Western Pacific (ECCWP) project in Vanuatu and the Western Highlands of Papua New Guinea.
Elimination of cervical cancer, which is defined as fewer than 4 cases per 100,000 women, would be a remarkable achievement in Australia and globally. The progress made thus far has been the result of new knowledge about the role of Human papillomavirus (HPV) as a causal factor for almost all cervical cancers, as well as innovations in preventive tools and technologies.
In 2020, the Director General of the WHO, Dr Tedros Ghebreysus, announced a Global Strategy to accelerate the elimination of cervical cancer as a public health problem within the next hundred years, setting interim 2030 targets across the three pillars of vaccination, screening and treatment. But continued collaborative local and global efforts are essential to ensure equity both between and within countries by 2030 and beyond. This starts by tackling the underlying inequities and the stigma associated with cervical cancer.
Cervical cancer: a disease of inequity
HPV is mainly transmitted through unprotected sexual contact. It is very common, and most sexually active people will get some type of HPV in their life, regardless of their gender or sexuality. HPV is the primary cause of cervical cancer, which is the fourth most common cancer among women globally. Despite its prevalence, cervical cancer remains a disease associated with stigma and shame, as people diagnosed with HPV infection and with cervical cancer can be wrongly accused of sexual infidelity or promiscuity, and the symptoms of cervical cancer - such as vaginal bleeding or a malodorous discharge - can be shame-inducing, and can leave women feeling isolated and alone.
Cervical cancer is also a disease of inequity both between and within countries. The latest Australian Elimination report shows that the overall incidence rate of cervical cancer is 6.3 per 100,000 women, but is nearly double for Aboriginal and Torres Strait Islander women.
In 2020, there were an estimated 604,000 new cases and 342,000 deaths globally, about 90% of which occurred in low- and middle-income countries. And the Western Pacific Region alone bears one quarter of the global cervical cancer burden, according to the WHO.
when
country
Australia
region
East and South East Asia and Oceania
Related Member Association
Family Planning Alliance Australia
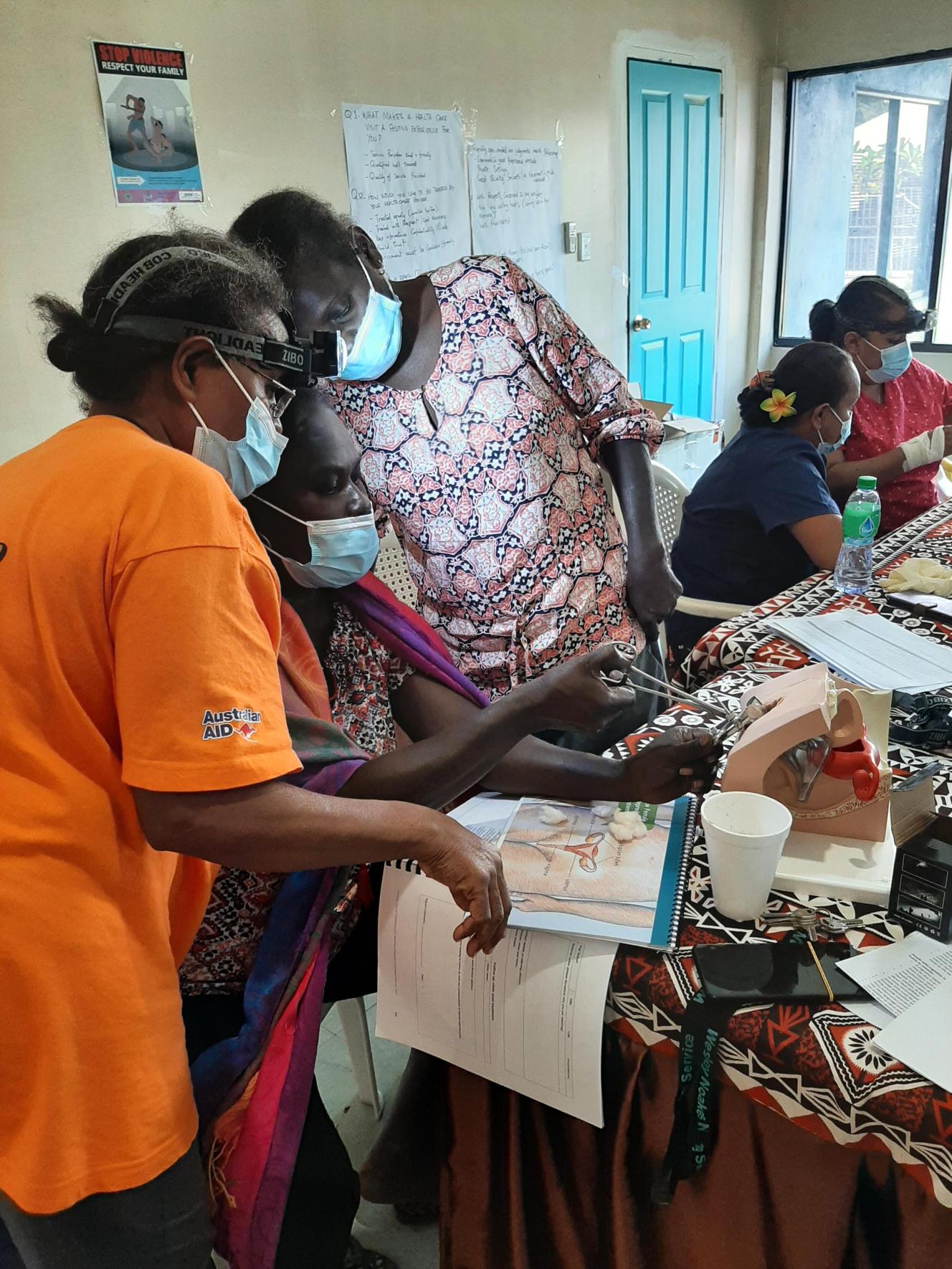
A training session between FPAA and the Solomon Islands Planned Parenthood Association
FPAADetecting and treating precancerous changes in the cervix can be life-saving. We need to make every effort to make access to screening easier and more equitable with a focus on under screened groups - particularly those from culturally and linguistically diverse communities, people living with disabilities, LGBTIQ+ people, First Nations women and those in rural and remote areas. Fortunately, several innovations are proving to be a game-changer in our efforts to eliminate cervical cancer.
Extraordinary advances in HPV knowledge
The development of the HPV vaccine was a major milestone in the quest to eliminate cervical cancer, and FPAA played a key role as a partner in a national research study to determine the impact of HPV vaccination on HPV prevalence, including amongst Indigenous women. This and other research showing the very high effectiveness of HPV screening in predicting current and future risk of high grade precancerous lesions and invasive cancer, helped pave the way for Australia’s ‘renewed’ National Cervical Screening Program (NCSP). In 2017 the NCSP transitioned from 2-yearly cytology screening for people with a cervix aged 18-20 to 69 years, to 5-yearly primary HPV screening from 25 to 74 years of age.
Another recent innovation is a new approach to HPV screening with a self-collected vaginal test without a speculum. This is a safe, acceptable and easy approach that can overcome barriers to screening to reach women who otherwise may not participate in a screening. Here in Australia, a major policy change in July 2022 saw the roll out of universal choice of either a clinician-collected cervical sample or a self-collected vaginal sample. For women who have experienced sexual assault, have pain due to vaginismus or other pelvic conditions, or have had prior poor screening experiences, this self-sampling option can be literally life-saving.
But screening is much more than taking a test. We need to ensure that all women and people with a cervix are aware of screening and that we provide culturally safe and acceptable services.
But screening is much more than taking a test. We need to ensure that all women and people with a cervix are aware of screening and that we provide culturally safe and acceptable services. We need high quality information and service provision by skilled, trained practitioners with correct techniques and equipment. We also need quality assured laboratories which provide evidence-based recommendations, and an ability to deliver the results to women efficiently and effectively.
Ensuring equitable access across the Pacific
Countries in the Pacific are very diverse with respect to geography, population, economy and culture. There is also variation in relation to cervical cancer prevention with some countries having organised programmes for vaccination and screening, while others may offer local opportunistic screening with Pap smears or with VIA (visual inspection with acetic acid).
While these approaches still play an important role in screening, countries are now urged by WHO to transition to HPV based screening – recognizing that the timeframe for this transition needs to be tailored to the unique and specific circumstances of each country, particularly those which are resource-constrained. Importantly, however, the skills employed by the existing workforce in cytology and VIA services can be adapted for HPV screening provision.
In Vanuatu and Papua New Guinea, for example, the C4 Elimination of Cervical Cancer in the Western Pacific project is supporting the WHO three-pronged approach including HPV vaccination, HPV screening and treatment or precancers, with referral pathways in place for invasive cancers.
Self-sampling is already being used widely in the ECCWP project, with one woman in Vanuatu stating: “The cervical cancer swab was not painful and it was easy and fast. I also got my result an hour later. There is not much waiting."
Global and local efforts are essential for ensuring equitable access to HPV tests as the costs of these tests can be prohibitive for some countries. FPNSW is currently working with its partners and Ministries of Health supporting screening through training programs In Tuvalu, Vanuatu and the Western Highlands of Papua New Guinea and The Solomon Islands.
Staying on track to meet the 2030 targets
Australia is managing to stay on track to eliminate cervical cancer despite challenges including the COVID-19 pandemic and pushback from some religious schools fuelling pockets of HPV vaccine hesitancy. All of the lessons we’ve learned with regards to the three pillars of vaccination, screening and treatment can potentially be adapted to other settings around the world, but it is crucial that these approaches are locally-led and community-designed.
Firstly, equitable access to HPV vaccine supplies at affordable prices is essential so the vaccine can be integrated within existing vaccine delivery programs in low and middle-income countries. The same is true for affordable HPV tests, and integration of screening into family planning, sexual health and HIV services is crucial.
All of the lessons we’ve learned with regards to the three pillars of vaccination, screening and treatment can potentially be adapted to other settings around the world, but it is crucial that these approaches are locally-led and community-designed.
But perhaps the most challenging pillar with regard to global equity is the treatment pillar. In Australia, women with high risk cancer-causing HPV types are referred for colposcopy to confirm whether treatment of a precancerous lesion is needed, or to specialised services if diagnosed with invasive cancer. However, we need to ensure that all women, including those who have had a self-collected screening test and those who may be fearful of a cancer diagnosis, can access services that are tailored to meet their particular needs. Access to these treatment services, particularly to cancer services, can be extremely limited in low resource settings.
Innovations such as the use of lightweight, portable and affordable hand-held thermal ablation devices by trained nurses in screen and treat programmes can address some of the challenges in treatment of precancer. But inequities in access to treatment of invasive cancers are stark, due to infrastructure costs and highly specialised workforce training needs, with women often needing to travel to other countries away from their families to receive care.
However, plans for locally generated sustainable solutions are underway including support for collaborative cross-country treatment hubs and raised awareness of the need for integrated palliative care and support services delivered through primary care for people diagnosed with cervical cancer.
While there is still work to be done in Australia, to reach elimination before 2035 would be an extraordinary achievement. We have the evidence and a shared commitment and now we have to prioritise the work to eliminate cervical cancer for everyone, everywhere.