Spotlight
A selection of stories from across the Federation

Advances in Sexual and Reproductive Rights and Health: 2024 in Review
Let’s take a leap back in time to the beginning of 2024: In twelve months, what victories has our movement managed to secure in the face of growing opposition and the rise of the far right? These victories for sexual and reproductive rights and health are the result of relentless grassroots work and advocacy by our Member Associations, in partnership with community organizations, allied politicians, and the mobilization of public opinion.
Most Popular This Week

Advances in Sexual and Reproductive Rights and Health: 2024 in Review
Let’s take a leap back in time to the beginning of 2024: In twelve months, what victories has our movement managed to secure in t
Kazakhstan

Kazakhstan's Rising HIV Crisis: A Call for Action
On World AIDS Day, we commemorate the remarkable achievements of IPPF Member Associations in their unwavering commitment to combating the HIV epidemic.

Ensuring SRHR in Humanitarian Crises: What You Need to Know
Over the past two decades, global forced displacement has consistently increased, affecting an estimated 114 million people as of mid-2023.
Estonia, Nepal, Namibia, Japan, Thailand

The Rainbow Wave for Marriage Equality
Love wins! The fight for marriage equality has seen incredible progress worldwide, with a recent surge in legalizations.
France, Germany, Poland, United Kingdom, United States, Colombia, India, Tunisia

Abortion Rights: Latest Decisions and Developments around the World
Over the past 30 years, more than

Palestine

In their own words: The people providing sexual and reproductive health care under bombardment in Gaza
Week after week, heavy Israeli bombardment from air, land, and sea, has continued across most of the Gaza Strip.
Vanuatu

When getting to the hospital is difficult, Vanuatu mobile outreach can save lives
In the mountains of Kumera on Tanna Island, Vanuatu, the village women of Kamahaul normally spend over 10,000 Vatu ($83 USD) to travel to the nearest hospital.
Filter our stories by:
- Afghanistan
- Albania
- Aruba
- Bangladesh
- Benin
- Botswana
- Burundi
- Cambodia
- Cameroon
- Colombia
- Congo, Dem. Rep.
- Cook Islands
- El Salvador
- Estonia
- Ethiopia
- (-) Fiji
- France
- Germany
- Ghana
- Guinea-Conakry
- India
- Ireland
- Jamaica
- Japan
- Kazakhstan
- Kenya
- Kiribati
- Lesotho
- Malawi
- Mali
- Mozambique
- Namibia
- (-) Nepal
- Nigeria
- Pakistan
- Palestine
- Poland
- Senegal
- Somaliland
- Sri Lanka
- Sudan
- Thailand
- Togo
- Tonga
- Trinidad and Tobago
- Tunisia
- Uganda
- United Kingdom
- United States
- Vanuatu
- Zambia

| 26 April 2024
The Rainbow Wave for Marriage Equality
Love wins! The fight for marriage equality has seen incredible progress worldwide, with a recent surge in legalizations. Across the world, 36 out of 195 countries have legalized equal marriage: Andorra, Argentina, Australia, Austria, Belgium, Brazil, Canada, Chile, Colombia, Costa Rica, Cuba, Denmark, Ecuador, Estonia, Finland, France, Germany, Greece, Iceland, Ireland, Luxembourg, Malta, Mexico, the Netherlands, New Zealand, Norway, Portugal, Slovenia, South Africa, Spain, Sweden, Switzerland, Taiwan, the United Kingdom, the United States of America and Uruguay. In 2023, three new countries legalized same-sex marriage (Andorra, Estonia and Slovenia), and three more solidified legislative progress towards decriminalizing same-sex unions: a Japanese court ruled it is unconstitutional for the nation not to legally recognize same-sex unions. And the Supreme Courts of Nepal and Namibia recognized marriages of same-sex couples registered abroad. So marriage equality marches on! Already in 2024, two more countries have said "I do" to equal rights. According to the Human Rights Campaign Foundation, even more countries could legalize equal marriage in 2024. In particular, the Czech Republic, India, Japan, Nepal and Philippines show signs of growing support for marriage equality. The fight for marriage equality isn't over, but the momentum is undeniable. IPPF stands with those working to make love win everywhere.
| 26 April 2024
The Rainbow Wave for Marriage Equality
Love wins! The fight for marriage equality has seen incredible progress worldwide, with a recent surge in legalizations. Across the world, 36 out of 195 countries have legalized equal marriage: Andorra, Argentina, Australia, Austria, Belgium, Brazil, Canada, Chile, Colombia, Costa Rica, Cuba, Denmark, Ecuador, Estonia, Finland, France, Germany, Greece, Iceland, Ireland, Luxembourg, Malta, Mexico, the Netherlands, New Zealand, Norway, Portugal, Slovenia, South Africa, Spain, Sweden, Switzerland, Taiwan, the United Kingdom, the United States of America and Uruguay. In 2023, three new countries legalized same-sex marriage (Andorra, Estonia and Slovenia), and three more solidified legislative progress towards decriminalizing same-sex unions: a Japanese court ruled it is unconstitutional for the nation not to legally recognize same-sex unions. And the Supreme Courts of Nepal and Namibia recognized marriages of same-sex couples registered abroad. So marriage equality marches on! Already in 2024, two more countries have said "I do" to equal rights. According to the Human Rights Campaign Foundation, even more countries could legalize equal marriage in 2024. In particular, the Czech Republic, India, Japan, Nepal and Philippines show signs of growing support for marriage equality. The fight for marriage equality isn't over, but the momentum is undeniable. IPPF stands with those working to make love win everywhere.

| 03 March 2021
The response to Tropical Cyclone Yasa: Through the eyes of a humanitarian surge member
Sera Vulavou is the Senior Monitoring and Evaluation Officer with IPPF’s Sub-Regional Office for the Pacific. She was trained as a humanitarian surge roster member in early 2020, to be able to deploy to emergencies to provide technical assistance to Member Associations – here she shares her experience with us. Severe Tropical Cyclone (TC) Yasa was the strongest in the South Pacific since TC Winston in 2016, as well as the fourth most intense TC on record in the basin. The Reproductive and Family Health Association of Fiji (RFHAF) humanitarian response to TC Yasa has reached some of the most difficult and geographically scattered islands and communities, which included the islands of Moala, Totoya, and Matuku. Being part of the IPPF humanitarian surge roster team gave me the opportunity to accompany the RFHAF response team during their humanitarian work. This experience was about putting in action what I could only personally describe as being at the right place at the right time.

| 15 May 2025
The response to Tropical Cyclone Yasa: Through the eyes of a humanitarian surge member
Sera Vulavou is the Senior Monitoring and Evaluation Officer with IPPF’s Sub-Regional Office for the Pacific. She was trained as a humanitarian surge roster member in early 2020, to be able to deploy to emergencies to provide technical assistance to Member Associations – here she shares her experience with us. Severe Tropical Cyclone (TC) Yasa was the strongest in the South Pacific since TC Winston in 2016, as well as the fourth most intense TC on record in the basin. The Reproductive and Family Health Association of Fiji (RFHAF) humanitarian response to TC Yasa has reached some of the most difficult and geographically scattered islands and communities, which included the islands of Moala, Totoya, and Matuku. Being part of the IPPF humanitarian surge roster team gave me the opportunity to accompany the RFHAF response team during their humanitarian work. This experience was about putting in action what I could only personally describe as being at the right place at the right time.

| 23 September 2020
In pictures: Innovating during COVID-19
Women around the world have faced multiple barriers to accessing safe abortion care during the COVID-19 pandemic including the de-prioritization of sexual and reproductive healthcare, overwhelmed health systems and restrictions on movement. The COVID-19 crisis has sparked innovation among IPPF Member Associations who responded swiftly by developing new approaches to reach women with safe abortion care including telemedicine and home-based provision of medical abortion. Strong evidence generated from this work supports the continuation and strengthening of these approaches beyond the end of the pandemic. Cameroon Cameroon National Planning Association for Family Welfare (CAMNAFAW) To ensure that quality abortion care can be provided to women during travel restrictions, CAMNAFAW’s service providers travel to partner clinics in underserved areas and to clients’ homes to provide medical and surgical abortion care. This model of taking safe abortion care closer to women will continue even with easing of travel restrictions, as this has been found to be an effective and acceptable approach to increasing access.Photo: IPPF/Xaume Olleros/Cameroon Share on Twitter Share on Facebook Share via WhatsApp Share via Email Guinea Association Guinéenne pour le Bien-Etre Familial (AGBEF) Building on lessons learned during the Ebola crisis in Guinea, AGBEF quickly took measures to prevent infection in its clinics to continue providing sexual and reproductive healthcare, including surgical and medical abortion, in a safe environment. AGBEF donated protective materials to communities, including hand-washing stations, face masks and antibacterial gel, alongside messaging on infection prevention. This community visibility reassures clients they can safely attend AGBEF clinics for abortion and contraceptive care.Photo: AGBEF/Guinea Share on Twitter Share on Facebook Share via WhatsApp Share via Email India Family Planning Association of India (FPA India) FPA India and partners advocated to have sexual and reproductive healthcare, including abortion, recognized as essential by the government, which meant FPA India could continue healthcare delivery during the national lockdown. To reduce in-person clinic visits, FPA India established teleconsultation and counselling for abortion care, and is continuing to provide in-clinic care for both medical and surgical abortion. Photo: IPPF/Alison Joyce/India Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nepal Family Planning Association of Nepal (FPAN) FPAN and partners advocated for interim approval of home provision of medical abortion and telemedicine for abortion counselling during COVID-19. FPAN is now implementing these approaches, ensuring continued access to abortion care in Nepal, where many people live in remote locations with limited mobility, which has been further restricted by COVID-19 lockdowns. Photo: FPAN/Nepal Share on Twitter Share on Facebook Share via WhatsApp Share via Email Pakistan Rahnuma – Family Planning Association of Pakistan (Rahnuma-FPAP) Rahnuma-FPAP and partners successfully advocated for the government to class sexual and reproductive healthcare as ‘essential’, which enabled the team to continue providing post-abortion care during the pandemic. Rahnuma-FPAP expanded its telemedicine and home-based provision for menstrual regulation counselling and post-abortion care. These new approaches have ensured continued access to services for clients unable to reach clinics.Photo: Rahnuma-FPAP/Pakistan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Palestine Palestinian Family Planning and Protection Association (PFPPA) In response to the government-mandated closure of its clinics, PFPPA quickly established a toll-free call centre which provides consultations, counselling, referrals and follow-up, including consultation for abortion care through a harm reduction approach, ensuring that women are provided with accurate information. Due to its success, PFPPA is exploring options for continuing this healthcare delivery model beyond the pandemic, with the aim of keeping it free of charge for users.Photo: SAAF/Samar Hazboun/Palestine Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sudan Sudan Family Planning Association (SFPA) Following a nation-wide shutdown in April, SFPA established a call centre to increase access to healthcare, including abortion and contraceptive counselling and referrals. An unexpected outcome of the new call centre is that it has reached an increased number of young women who regularly call to discuss their reproductive health and rights. SFPA is working towards institutionalizing this model for continuation beyond the pandemic.Photo: SFPA/Sudan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Togo Association Togolaise pour le Bien-Etre Familial (ATBEF) ATBEF adapted its mobile application ‘Infos Ado Jeunes’, adding a toll-free teleconsultation service for young clients to use to access abortion consultations and pre- and post-abortion counselling. This app has given young clients ongoing access to care when they face challenges travelling to clinics. It has also eased overall client flow in clinics at a time when social distancing is being implemented.Photo: ATBEF/Togo Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 15 May 2025
In pictures: Innovating during COVID-19
Women around the world have faced multiple barriers to accessing safe abortion care during the COVID-19 pandemic including the de-prioritization of sexual and reproductive healthcare, overwhelmed health systems and restrictions on movement. The COVID-19 crisis has sparked innovation among IPPF Member Associations who responded swiftly by developing new approaches to reach women with safe abortion care including telemedicine and home-based provision of medical abortion. Strong evidence generated from this work supports the continuation and strengthening of these approaches beyond the end of the pandemic. Cameroon Cameroon National Planning Association for Family Welfare (CAMNAFAW) To ensure that quality abortion care can be provided to women during travel restrictions, CAMNAFAW’s service providers travel to partner clinics in underserved areas and to clients’ homes to provide medical and surgical abortion care. This model of taking safe abortion care closer to women will continue even with easing of travel restrictions, as this has been found to be an effective and acceptable approach to increasing access.Photo: IPPF/Xaume Olleros/Cameroon Share on Twitter Share on Facebook Share via WhatsApp Share via Email Guinea Association Guinéenne pour le Bien-Etre Familial (AGBEF) Building on lessons learned during the Ebola crisis in Guinea, AGBEF quickly took measures to prevent infection in its clinics to continue providing sexual and reproductive healthcare, including surgical and medical abortion, in a safe environment. AGBEF donated protective materials to communities, including hand-washing stations, face masks and antibacterial gel, alongside messaging on infection prevention. This community visibility reassures clients they can safely attend AGBEF clinics for abortion and contraceptive care.Photo: AGBEF/Guinea Share on Twitter Share on Facebook Share via WhatsApp Share via Email India Family Planning Association of India (FPA India) FPA India and partners advocated to have sexual and reproductive healthcare, including abortion, recognized as essential by the government, which meant FPA India could continue healthcare delivery during the national lockdown. To reduce in-person clinic visits, FPA India established teleconsultation and counselling for abortion care, and is continuing to provide in-clinic care for both medical and surgical abortion. Photo: IPPF/Alison Joyce/India Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nepal Family Planning Association of Nepal (FPAN) FPAN and partners advocated for interim approval of home provision of medical abortion and telemedicine for abortion counselling during COVID-19. FPAN is now implementing these approaches, ensuring continued access to abortion care in Nepal, where many people live in remote locations with limited mobility, which has been further restricted by COVID-19 lockdowns. Photo: FPAN/Nepal Share on Twitter Share on Facebook Share via WhatsApp Share via Email Pakistan Rahnuma – Family Planning Association of Pakistan (Rahnuma-FPAP) Rahnuma-FPAP and partners successfully advocated for the government to class sexual and reproductive healthcare as ‘essential’, which enabled the team to continue providing post-abortion care during the pandemic. Rahnuma-FPAP expanded its telemedicine and home-based provision for menstrual regulation counselling and post-abortion care. These new approaches have ensured continued access to services for clients unable to reach clinics.Photo: Rahnuma-FPAP/Pakistan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Palestine Palestinian Family Planning and Protection Association (PFPPA) In response to the government-mandated closure of its clinics, PFPPA quickly established a toll-free call centre which provides consultations, counselling, referrals and follow-up, including consultation for abortion care through a harm reduction approach, ensuring that women are provided with accurate information. Due to its success, PFPPA is exploring options for continuing this healthcare delivery model beyond the pandemic, with the aim of keeping it free of charge for users.Photo: SAAF/Samar Hazboun/Palestine Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sudan Sudan Family Planning Association (SFPA) Following a nation-wide shutdown in April, SFPA established a call centre to increase access to healthcare, including abortion and contraceptive counselling and referrals. An unexpected outcome of the new call centre is that it has reached an increased number of young women who regularly call to discuss their reproductive health and rights. SFPA is working towards institutionalizing this model for continuation beyond the pandemic.Photo: SFPA/Sudan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Togo Association Togolaise pour le Bien-Etre Familial (ATBEF) ATBEF adapted its mobile application ‘Infos Ado Jeunes’, adding a toll-free teleconsultation service for young clients to use to access abortion consultations and pre- and post-abortion counselling. This app has given young clients ongoing access to care when they face challenges travelling to clinics. It has also eased overall client flow in clinics at a time when social distancing is being implemented.Photo: ATBEF/Togo Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 13 August 2020
In pictures: Delivering healthcare to remote communities in Fiji
In early April 2020, the all too familiar destruction of a Tropical Cyclone (TC) – Harold – hit the Solomon Islands, Vanuatu, Fiji and Tonga. One of the worst affected areas was the Eastern part of Fiji. Through support by Department of Foreign Affairs and Trade (DFAT), our Member Association, Reproductive and Family Health Association of Fiji (RFHAF), was quick to respond ensuring access to essential sexual and reproductive healthcare for Kadavu’s women, girls, and vulnerable groups. Fiji's vulnerable coastline Fiji’s worst affected area was the Eastern part, with TC Harold bringing destructive storm force winds and storm surge. RFHAF focused its humanitarian response on the local Kadavu population. This remote area proves a challenge to reach for the team with supplies. Share on Twitter Share on Facebook Share via WhatsApp Share via Email RFHAF's humanitarian response team tackle rough terrain National travel restrictions - due to the current COVID-19 pandemic - on all inter island transfers has slowed the response in some areas, including Kadavu. The island of Kadavu is one of the least developed areas of Fiji, the main source of income is substance living (Yaqona). Transport around the island is difficult, with very few roads, no public water system or electricity. The humanitarian team from RFHAF travels by boat and then on foot. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Asenaca, client Kadavu, the biggest island in the Eastern division has the greatest population (10,897). 197 evacuation centres were activated in total, initially hosting over 6,240 people. Many are women of reproductive age, with an estimated 150 currently pregnant. Asenaca learns about breast cancer self-checks from RFHAF’s healthcare provider, Karo. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nasi, RFHAF healthcare provider The medical mobile team deliver a broad range of healthcare including contraception, information and counselling on sexual health, pregnancy, HIV and STI care and testing. RFHAF Team in Kadavu performing general health checks after TC Harold. Nasi administers a HPV shot to a client. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Kate, client Young women and girls are at the heart of RFHAF’s healthcare provision. Kate walks home with her dignity kit after a health check at the mobile clinic. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Karo, RFHAF healthcare worker RFHAF offers sexual and reproductive healthcare as well as counselling, and referrals for follow up care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Alidi, RFHAF healthcare worker The team ensures young people in the community are not forgotten and provide information and education on relationships and sexual health and rights. Alidi conducting a session with a local group of young people at Gasele, Kadavu.Photos ©IPPF/Rob Rickman/Fiji Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 15 May 2025
In pictures: Delivering healthcare to remote communities in Fiji
In early April 2020, the all too familiar destruction of a Tropical Cyclone (TC) – Harold – hit the Solomon Islands, Vanuatu, Fiji and Tonga. One of the worst affected areas was the Eastern part of Fiji. Through support by Department of Foreign Affairs and Trade (DFAT), our Member Association, Reproductive and Family Health Association of Fiji (RFHAF), was quick to respond ensuring access to essential sexual and reproductive healthcare for Kadavu’s women, girls, and vulnerable groups. Fiji's vulnerable coastline Fiji’s worst affected area was the Eastern part, with TC Harold bringing destructive storm force winds and storm surge. RFHAF focused its humanitarian response on the local Kadavu population. This remote area proves a challenge to reach for the team with supplies. Share on Twitter Share on Facebook Share via WhatsApp Share via Email RFHAF's humanitarian response team tackle rough terrain National travel restrictions - due to the current COVID-19 pandemic - on all inter island transfers has slowed the response in some areas, including Kadavu. The island of Kadavu is one of the least developed areas of Fiji, the main source of income is substance living (Yaqona). Transport around the island is difficult, with very few roads, no public water system or electricity. The humanitarian team from RFHAF travels by boat and then on foot. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Asenaca, client Kadavu, the biggest island in the Eastern division has the greatest population (10,897). 197 evacuation centres were activated in total, initially hosting over 6,240 people. Many are women of reproductive age, with an estimated 150 currently pregnant. Asenaca learns about breast cancer self-checks from RFHAF’s healthcare provider, Karo. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nasi, RFHAF healthcare provider The medical mobile team deliver a broad range of healthcare including contraception, information and counselling on sexual health, pregnancy, HIV and STI care and testing. RFHAF Team in Kadavu performing general health checks after TC Harold. Nasi administers a HPV shot to a client. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Kate, client Young women and girls are at the heart of RFHAF’s healthcare provision. Kate walks home with her dignity kit after a health check at the mobile clinic. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Karo, RFHAF healthcare worker RFHAF offers sexual and reproductive healthcare as well as counselling, and referrals for follow up care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Alidi, RFHAF healthcare worker The team ensures young people in the community are not forgotten and provide information and education on relationships and sexual health and rights. Alidi conducting a session with a local group of young people at Gasele, Kadavu.Photos ©IPPF/Rob Rickman/Fiji Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 15 February 2019
"I’m so happy I now don’t have to worry about contraception for another five years”
In August 2017, weeks of continued and heavy rainfall across Nepal resulted in flash floods and landslides that affected 36 of the 75 districts. Many people lost their homes or were displaced. It was estimated that of those affected, 112,500 were women of reproductive age, including 8,694 pregnant women. IPPF Humanitarian, through their Member Association, The Family Planning Association of Nepal (FPAN), activated its emergency response system early on. With funding support from the Australian Government, FPAN and IPPF Humanitarian initially mobilised their response in four of the worst affected districts (Sunsari, Saptari, Bardiya, and Dang). Mobile medical camps were established to meet the sexual and reproductive health needs of the affected population, including through the distribution of short and long acting methods of contraception, STI and HIV screening, and GBV referrals. In collaboration with the USAID-SIFPO project, services were then expanded into five more affected districts. IPPF Humanitarian spoke with 21-year old Muna in her home district of Sunsari in Nepal. “I got married at 16 years old and have two children, a four-year-old girl and two-year-old boy. In my caste, we get married early, so my parents took me to get an arranged marriage. I was in the 8th class at the time, and returned to school after I got married, but only lasted one year. My husband works in construction and had to stop working for two weeks when the floods came. When he doesn’t work, he doesn’t get paid, so it’s been very difficult. A FPAN social worker told me about the mobile medical camp today. I used to be on the three-month injectable but today I changed to the five-year implant in my arm. When my youngest child was eight months old I found out I was pregnant again. I decided to discontinue that pregnancy, so I took the five small tablets given to me by my neighbourhood doctor. I was two months pregnant at the time. From this, I had two days bleeding and cramp like pain, and then weakness. I decided to abort that pregnancy because my youngest will still only eight months old, and I didn’t want any more children. If I had more than two children, it would be very difficult to feed and educate them, and would badly affect my body too. I’m so happy I now don’t have to worry about contraception for another five years.” Want to know more about safe abortion access? Join IPPF'S I Decide movement

| 15 May 2025
"I’m so happy I now don’t have to worry about contraception for another five years”
In August 2017, weeks of continued and heavy rainfall across Nepal resulted in flash floods and landslides that affected 36 of the 75 districts. Many people lost their homes or were displaced. It was estimated that of those affected, 112,500 were women of reproductive age, including 8,694 pregnant women. IPPF Humanitarian, through their Member Association, The Family Planning Association of Nepal (FPAN), activated its emergency response system early on. With funding support from the Australian Government, FPAN and IPPF Humanitarian initially mobilised their response in four of the worst affected districts (Sunsari, Saptari, Bardiya, and Dang). Mobile medical camps were established to meet the sexual and reproductive health needs of the affected population, including through the distribution of short and long acting methods of contraception, STI and HIV screening, and GBV referrals. In collaboration with the USAID-SIFPO project, services were then expanded into five more affected districts. IPPF Humanitarian spoke with 21-year old Muna in her home district of Sunsari in Nepal. “I got married at 16 years old and have two children, a four-year-old girl and two-year-old boy. In my caste, we get married early, so my parents took me to get an arranged marriage. I was in the 8th class at the time, and returned to school after I got married, but only lasted one year. My husband works in construction and had to stop working for two weeks when the floods came. When he doesn’t work, he doesn’t get paid, so it’s been very difficult. A FPAN social worker told me about the mobile medical camp today. I used to be on the three-month injectable but today I changed to the five-year implant in my arm. When my youngest child was eight months old I found out I was pregnant again. I decided to discontinue that pregnancy, so I took the five small tablets given to me by my neighbourhood doctor. I was two months pregnant at the time. From this, I had two days bleeding and cramp like pain, and then weakness. I decided to abort that pregnancy because my youngest will still only eight months old, and I didn’t want any more children. If I had more than two children, it would be very difficult to feed and educate them, and would badly affect my body too. I’m so happy I now don’t have to worry about contraception for another five years.” Want to know more about safe abortion access? Join IPPF'S I Decide movement

| 29 November 2017
Meet the college student who uses his music to battle the stigma surrounding HIV
Milan Khadka was just ten years old when he lost both his parents to HIV. “When I lost my parents, I used to feel so alone, like I didn’t have anyone in the world,” he says. “Whenever I saw other children getting love from others, I used to feel that I also might get that kind of love if I hadn’t lost my parents.” Like thousands of Nepali children, Milan’s parents left Nepal for India in search of work. Milan grew up in India until he was ten, when his mother died of AIDS-related causes. The family then returned to Nepal, but just eight months later, his father also died, and Milan was left in the care of his grandmother. “After I lost my parents, I went for VCT [voluntary counselling and testing] to check if I had HIV in my body,” Milan says. “After I was diagnosed as HIV positive, slowly all the people in the area found out about my status and there was so much discrimination. My friends at school didn’t want to sit with me and they humiliated and bullied me,” he says. “At home, I had a separate sleeping area and sleeping materials, separate dishes and a separate comb for my hair. I had to sleep alone.” Things began to improve for Milan when he met a local woman called Lakshmi Kunwar. After discovering she was HIV-positive, Lakshmi had dedicated her life to helping people living with HIV in Palpa, working as a community home-based care mobiliser for the Family Planning Association of Nepal (FPAN) and other organisations. Struck by the plight of this small, orphaned boy, Lakshmi spoke to Milan’s family and teachers, who in turn spoke to his school mates. “After she spoke to my teachers, they started to support me,” Milan says. “And after getting information about HIV, my school friends started to like me and share things with me. And they said: ‘Milan has no one in this world, so we are the ones who must be with him. Who knows that what happened to him might not happen to us?” Lakshmi mentored him through school and college, encouraging him in his schoolwork. “Lakshmi is more than my mother,” he says. “My mother only gave birth to me but Lakshmi has looked after me all this time. Even if my mother was alive today, she might not do all the things for me that Lakshmi has done.” Milan went on to become a grade A student, regularly coming top of his class and leaving school with flying colours. Today, twenty-one-year-old Milan lives a busy and fulfilling life, juggling his college studies, his work as a community home-based care (CHBC) mobiliser for FPAN and a burgeoning music career. When not studying for a Bachelor’s of education at university in Tansen, he works as a CHBC mobiliser for FPAN, visiting villages in the area to raise awareness about how to prevent and treat HIV, and to distribute contraception. He also offers support to children living with HIV, explaining to them how he lost his parents and faced discrimination but now leads a happy and successful life. “There are 40 children in this area living with HIV,” he says. “I talk to them, collect information from them and help them get the support they need. And I tell them: ‘If I had given up at that time, I would not be like this now. So you also shouldn’t give up, and you have to live your life.” Watch Milan's story below:

| 15 May 2025
Meet the college student who uses his music to battle the stigma surrounding HIV
Milan Khadka was just ten years old when he lost both his parents to HIV. “When I lost my parents, I used to feel so alone, like I didn’t have anyone in the world,” he says. “Whenever I saw other children getting love from others, I used to feel that I also might get that kind of love if I hadn’t lost my parents.” Like thousands of Nepali children, Milan’s parents left Nepal for India in search of work. Milan grew up in India until he was ten, when his mother died of AIDS-related causes. The family then returned to Nepal, but just eight months later, his father also died, and Milan was left in the care of his grandmother. “After I lost my parents, I went for VCT [voluntary counselling and testing] to check if I had HIV in my body,” Milan says. “After I was diagnosed as HIV positive, slowly all the people in the area found out about my status and there was so much discrimination. My friends at school didn’t want to sit with me and they humiliated and bullied me,” he says. “At home, I had a separate sleeping area and sleeping materials, separate dishes and a separate comb for my hair. I had to sleep alone.” Things began to improve for Milan when he met a local woman called Lakshmi Kunwar. After discovering she was HIV-positive, Lakshmi had dedicated her life to helping people living with HIV in Palpa, working as a community home-based care mobiliser for the Family Planning Association of Nepal (FPAN) and other organisations. Struck by the plight of this small, orphaned boy, Lakshmi spoke to Milan’s family and teachers, who in turn spoke to his school mates. “After she spoke to my teachers, they started to support me,” Milan says. “And after getting information about HIV, my school friends started to like me and share things with me. And they said: ‘Milan has no one in this world, so we are the ones who must be with him. Who knows that what happened to him might not happen to us?” Lakshmi mentored him through school and college, encouraging him in his schoolwork. “Lakshmi is more than my mother,” he says. “My mother only gave birth to me but Lakshmi has looked after me all this time. Even if my mother was alive today, she might not do all the things for me that Lakshmi has done.” Milan went on to become a grade A student, regularly coming top of his class and leaving school with flying colours. Today, twenty-one-year-old Milan lives a busy and fulfilling life, juggling his college studies, his work as a community home-based care (CHBC) mobiliser for FPAN and a burgeoning music career. When not studying for a Bachelor’s of education at university in Tansen, he works as a CHBC mobiliser for FPAN, visiting villages in the area to raise awareness about how to prevent and treat HIV, and to distribute contraception. He also offers support to children living with HIV, explaining to them how he lost his parents and faced discrimination but now leads a happy and successful life. “There are 40 children in this area living with HIV,” he says. “I talk to them, collect information from them and help them get the support they need. And I tell them: ‘If I had given up at that time, I would not be like this now. So you also shouldn’t give up, and you have to live your life.” Watch Milan's story below:

| 12 September 2017
"I said to myself: I will live and I will let others living with HIV live"
Lakshmi Kunwar married young, at the age of 17. Shortly afterwards, Lakshmi’s husband, who worked as a migrant labourer in India, was diagnosed with HIV and died. “At that time, I was completely unaware of HIV,” Lakshmi says. “My husband had information that if someone is diagnosed with HIV, they will die very soon. So after he was diagnosed, he didn’t eat anything and he became very ill and after six months he died. He gave up.” Lakshmi contracted HIV too, and the early years of living with it were arduous. “It was a huge burden,” she says. “I didn’t want to eat anything so I ate very little. My weight at the time was 44 kilograms. I had different infections in my skin and allergies in her body. It was really a difficult time for me. … I was just waiting for my death. I got support from my home and in-laws but my neighbours started to discriminate against me – like they said HIV may transfer via different insects and parasites like lice.” Dedicating her life to help others Lakshmi’s life began to improve when she came across an organisation in Palpa that offered support to people living with HIV (PLHIV). “They told me that there is medicine for PLHIV which will prolong our lives,” she explains. “They took me to Kathmandu, where I got training and information on HIV and I started taking ARVs [antiretroviral drugs].” In Kathmandu Lakshmi decided that she would dedicate the rest of her life to supporting people living with HIV. “I made a plan that I would come back home [to Palpa], disclose my status and then do social work with other people living with HIV, so that they too may have hope to live. I said to myself: I will live and I will let others living with HIV live”. Stories Read more stories about our work with people living with HIV

| 15 May 2025
"I said to myself: I will live and I will let others living with HIV live"
Lakshmi Kunwar married young, at the age of 17. Shortly afterwards, Lakshmi’s husband, who worked as a migrant labourer in India, was diagnosed with HIV and died. “At that time, I was completely unaware of HIV,” Lakshmi says. “My husband had information that if someone is diagnosed with HIV, they will die very soon. So after he was diagnosed, he didn’t eat anything and he became very ill and after six months he died. He gave up.” Lakshmi contracted HIV too, and the early years of living with it were arduous. “It was a huge burden,” she says. “I didn’t want to eat anything so I ate very little. My weight at the time was 44 kilograms. I had different infections in my skin and allergies in her body. It was really a difficult time for me. … I was just waiting for my death. I got support from my home and in-laws but my neighbours started to discriminate against me – like they said HIV may transfer via different insects and parasites like lice.” Dedicating her life to help others Lakshmi’s life began to improve when she came across an organisation in Palpa that offered support to people living with HIV (PLHIV). “They told me that there is medicine for PLHIV which will prolong our lives,” she explains. “They took me to Kathmandu, where I got training and information on HIV and I started taking ARVs [antiretroviral drugs].” In Kathmandu Lakshmi decided that she would dedicate the rest of her life to supporting people living with HIV. “I made a plan that I would come back home [to Palpa], disclose my status and then do social work with other people living with HIV, so that they too may have hope to live. I said to myself: I will live and I will let others living with HIV live”. Stories Read more stories about our work with people living with HIV

| 08 September 2017
“Attitudes of younger people to HIV are not changing fast"
“When I was 14, I was trafficked to India,” says 35-year-old Lakshmi Lama. “I was made unconscious and was taken to Mumbai. When I woke up, I didn’t even know that I had been trafficked, I didn’t know where I was.” Every year, thousands of Nepali women and girls are trafficked to India, some lured with the promise of domestic work only to find themselves in brothels or working as sex slaves. The visa-free border with India means the actual number of women and girls trafficked from Nepal is likely to be much higher. The earthquake of April 2015 also led to a surge in trafficking: women and girls living in tents or temporary housing, and young orphaned children were particularly vulnerable to traffickers. “I was in Mumbai for three years,” says Lakshmi. “Then I managed to send letters and photographs to my parents and eventually they came to Mumbai and helped rescue me from that place". During her time in India, Lakshmi contracted HIV. Life after her diagnosis was tough, Lakshmi explains. “When I was diagnosed with HIV, people used to discriminate saying, “you’ve got HIV and it might transfer to us so don’t come to our home, don’t touch us,’” she says. “It’s very challenging for people living with HIV in Nepal. People really suffer.” Today, Lakshmi lives in Banepa, a busy town around 25 kilometres east of Kathmandu. Things began to improve for her, she says, when she started attending HIV awareness classes run by Family Planning Association of Nepal (FPAN). Eventually she herself trained as an FPAN peer educator, and she now works hard visiting communities in Kavre, raising awareness about HIV prevention and treatment, and bringing people together to tackle stigma around the virus. The government needs to do far more to tackle HIV stigma in Nepal, particularly at village level, Lakshmi says, “Attitudes of younger people to HIV are not changing fast. People still say to me: ‘you have HIV, you may die soon’. There is so much stigma and discrimination in this community.” Stories Read more stories about our work with people living with HIV

| 15 May 2025
“Attitudes of younger people to HIV are not changing fast"
“When I was 14, I was trafficked to India,” says 35-year-old Lakshmi Lama. “I was made unconscious and was taken to Mumbai. When I woke up, I didn’t even know that I had been trafficked, I didn’t know where I was.” Every year, thousands of Nepali women and girls are trafficked to India, some lured with the promise of domestic work only to find themselves in brothels or working as sex slaves. The visa-free border with India means the actual number of women and girls trafficked from Nepal is likely to be much higher. The earthquake of April 2015 also led to a surge in trafficking: women and girls living in tents or temporary housing, and young orphaned children were particularly vulnerable to traffickers. “I was in Mumbai for three years,” says Lakshmi. “Then I managed to send letters and photographs to my parents and eventually they came to Mumbai and helped rescue me from that place". During her time in India, Lakshmi contracted HIV. Life after her diagnosis was tough, Lakshmi explains. “When I was diagnosed with HIV, people used to discriminate saying, “you’ve got HIV and it might transfer to us so don’t come to our home, don’t touch us,’” she says. “It’s very challenging for people living with HIV in Nepal. People really suffer.” Today, Lakshmi lives in Banepa, a busy town around 25 kilometres east of Kathmandu. Things began to improve for her, she says, when she started attending HIV awareness classes run by Family Planning Association of Nepal (FPAN). Eventually she herself trained as an FPAN peer educator, and she now works hard visiting communities in Kavre, raising awareness about HIV prevention and treatment, and bringing people together to tackle stigma around the virus. The government needs to do far more to tackle HIV stigma in Nepal, particularly at village level, Lakshmi says, “Attitudes of younger people to HIV are not changing fast. People still say to me: ‘you have HIV, you may die soon’. There is so much stigma and discrimination in this community.” Stories Read more stories about our work with people living with HIV

| 08 September 2017
'My neighbours used to discriminate against me and I suffered violence at the hands of my community'
"My husband used to work in India, and when he came back, he got ill and died," says Durga Thame. "We didn’t know that he was HIV-positive, but then then later my daughter got sick with typhoid and went to hospital and was diagnosed with HIV and died, and then I was tested and was found positive." Her story is tragic, but one all too familiar for the women living in this region. Men often travel to India in search of work, where they contract HIV and upon their return infect their wives. For Durga, the death of her husband and daughter and her own HIV positive diagnosis threw her into despair. "My neighbours used to discriminate against me … and I suffered violence at the hands of my community. Everybody used to say that they couldn’t eat whatever I cooked because they might get HIV." Then Durga heard about HIV education classes run by the Palpa branch of the Family Planning Association of Nepal (FPAN), a short bus journey up the road in Tansen, the capital of Palpa. "At those meetings, I got information about HIV," she says. "When I came back to my village, I began telling my neighbours about HIV. They came to know the facts and they realised it was a myth that HIV could be transferred by sharing food. Then they began treating me well." FPAN ran nutrition, hygiene, sanitation and livelihood classes that helped Durga turn the fortunes of her small homestead around. Durga sells goats and hens, and with these earnings supports her family – her father-in-law and her surviving daughter, who she says has not yet been tested for HIV. "I want to educate my daughter," she says. "I really hope I can provide a better education for her." Stories Read more stories about our work with people living with HIV

| 15 May 2025
'My neighbours used to discriminate against me and I suffered violence at the hands of my community'
"My husband used to work in India, and when he came back, he got ill and died," says Durga Thame. "We didn’t know that he was HIV-positive, but then then later my daughter got sick with typhoid and went to hospital and was diagnosed with HIV and died, and then I was tested and was found positive." Her story is tragic, but one all too familiar for the women living in this region. Men often travel to India in search of work, where they contract HIV and upon their return infect their wives. For Durga, the death of her husband and daughter and her own HIV positive diagnosis threw her into despair. "My neighbours used to discriminate against me … and I suffered violence at the hands of my community. Everybody used to say that they couldn’t eat whatever I cooked because they might get HIV." Then Durga heard about HIV education classes run by the Palpa branch of the Family Planning Association of Nepal (FPAN), a short bus journey up the road in Tansen, the capital of Palpa. "At those meetings, I got information about HIV," she says. "When I came back to my village, I began telling my neighbours about HIV. They came to know the facts and they realised it was a myth that HIV could be transferred by sharing food. Then they began treating me well." FPAN ran nutrition, hygiene, sanitation and livelihood classes that helped Durga turn the fortunes of her small homestead around. Durga sells goats and hens, and with these earnings supports her family – her father-in-law and her surviving daughter, who she says has not yet been tested for HIV. "I want to educate my daughter," she says. "I really hope I can provide a better education for her." Stories Read more stories about our work with people living with HIV

| 21 August 2017
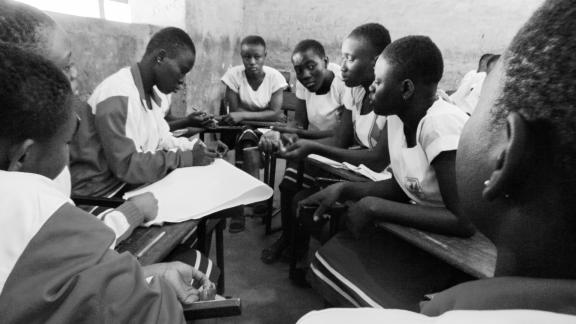
How youth volunteers are leading the conversation on HIV with young people in Nepal
Mala Neupane is just 18 years old, but is already an experienced volunteer for the Family Planning Association of Nepal (FPAN). Mala lives in Tansen, the hillside capital of Palpa, a region of rolling hills, pine forests and lush terraced fields in western Nepal. She works as a community home-based care mobiliser focusing on HIV: her job involves travelling to villages around Tansen to provide people with information about HIV and contraception. “Before, the community had very little knowledge regarding HIV and there used to be so much stigma and discrimination,” she says. “But later, when the Community Health Based Carers (CHBCs) started working in those communities, they had more knowledge and less stigma.” The youth of the volunteers proved an effective tool during their conversations with villagers. “At first, when they talked to people about family planning, they were not receptive: they felt resistance to using those devices,” Mala explains. “The CHBCs said to them: ‘young people like us are doing this kind of work, so why are you feeling such hesitation?’ After talking with them, they became ready to use contraceptives.” Her age is also important for connecting with young people, in a society of rapid change, she says. “Because we are young, we may know more about what young people’s needs and wants are. We can talk to young people about what family planning methods might be suitable for them, and what the options are.” “Young people’s involvement [in FPAN programmes] is very important to helping out young people like us.” It’s a simple message, but one reaping rich rewards for the lives and wellbeing of people in Palpa.

| 15 May 2025
How youth volunteers are leading the conversation on HIV with young people in Nepal
Mala Neupane is just 18 years old, but is already an experienced volunteer for the Family Planning Association of Nepal (FPAN). Mala lives in Tansen, the hillside capital of Palpa, a region of rolling hills, pine forests and lush terraced fields in western Nepal. She works as a community home-based care mobiliser focusing on HIV: her job involves travelling to villages around Tansen to provide people with information about HIV and contraception. “Before, the community had very little knowledge regarding HIV and there used to be so much stigma and discrimination,” she says. “But later, when the Community Health Based Carers (CHBCs) started working in those communities, they had more knowledge and less stigma.” The youth of the volunteers proved an effective tool during their conversations with villagers. “At first, when they talked to people about family planning, they were not receptive: they felt resistance to using those devices,” Mala explains. “The CHBCs said to them: ‘young people like us are doing this kind of work, so why are you feeling such hesitation?’ After talking with them, they became ready to use contraceptives.” Her age is also important for connecting with young people, in a society of rapid change, she says. “Because we are young, we may know more about what young people’s needs and wants are. We can talk to young people about what family planning methods might be suitable for them, and what the options are.” “Young people’s involvement [in FPAN programmes] is very important to helping out young people like us.” It’s a simple message, but one reaping rich rewards for the lives and wellbeing of people in Palpa.
| 26 April 2024
The Rainbow Wave for Marriage Equality
Love wins! The fight for marriage equality has seen incredible progress worldwide, with a recent surge in legalizations. Across the world, 36 out of 195 countries have legalized equal marriage: Andorra, Argentina, Australia, Austria, Belgium, Brazil, Canada, Chile, Colombia, Costa Rica, Cuba, Denmark, Ecuador, Estonia, Finland, France, Germany, Greece, Iceland, Ireland, Luxembourg, Malta, Mexico, the Netherlands, New Zealand, Norway, Portugal, Slovenia, South Africa, Spain, Sweden, Switzerland, Taiwan, the United Kingdom, the United States of America and Uruguay. In 2023, three new countries legalized same-sex marriage (Andorra, Estonia and Slovenia), and three more solidified legislative progress towards decriminalizing same-sex unions: a Japanese court ruled it is unconstitutional for the nation not to legally recognize same-sex unions. And the Supreme Courts of Nepal and Namibia recognized marriages of same-sex couples registered abroad. So marriage equality marches on! Already in 2024, two more countries have said "I do" to equal rights. According to the Human Rights Campaign Foundation, even more countries could legalize equal marriage in 2024. In particular, the Czech Republic, India, Japan, Nepal and Philippines show signs of growing support for marriage equality. The fight for marriage equality isn't over, but the momentum is undeniable. IPPF stands with those working to make love win everywhere.
| 26 April 2024
The Rainbow Wave for Marriage Equality
Love wins! The fight for marriage equality has seen incredible progress worldwide, with a recent surge in legalizations. Across the world, 36 out of 195 countries have legalized equal marriage: Andorra, Argentina, Australia, Austria, Belgium, Brazil, Canada, Chile, Colombia, Costa Rica, Cuba, Denmark, Ecuador, Estonia, Finland, France, Germany, Greece, Iceland, Ireland, Luxembourg, Malta, Mexico, the Netherlands, New Zealand, Norway, Portugal, Slovenia, South Africa, Spain, Sweden, Switzerland, Taiwan, the United Kingdom, the United States of America and Uruguay. In 2023, three new countries legalized same-sex marriage (Andorra, Estonia and Slovenia), and three more solidified legislative progress towards decriminalizing same-sex unions: a Japanese court ruled it is unconstitutional for the nation not to legally recognize same-sex unions. And the Supreme Courts of Nepal and Namibia recognized marriages of same-sex couples registered abroad. So marriage equality marches on! Already in 2024, two more countries have said "I do" to equal rights. According to the Human Rights Campaign Foundation, even more countries could legalize equal marriage in 2024. In particular, the Czech Republic, India, Japan, Nepal and Philippines show signs of growing support for marriage equality. The fight for marriage equality isn't over, but the momentum is undeniable. IPPF stands with those working to make love win everywhere.

| 03 March 2021
The response to Tropical Cyclone Yasa: Through the eyes of a humanitarian surge member
Sera Vulavou is the Senior Monitoring and Evaluation Officer with IPPF’s Sub-Regional Office for the Pacific. She was trained as a humanitarian surge roster member in early 2020, to be able to deploy to emergencies to provide technical assistance to Member Associations – here she shares her experience with us. Severe Tropical Cyclone (TC) Yasa was the strongest in the South Pacific since TC Winston in 2016, as well as the fourth most intense TC on record in the basin. The Reproductive and Family Health Association of Fiji (RFHAF) humanitarian response to TC Yasa has reached some of the most difficult and geographically scattered islands and communities, which included the islands of Moala, Totoya, and Matuku. Being part of the IPPF humanitarian surge roster team gave me the opportunity to accompany the RFHAF response team during their humanitarian work. This experience was about putting in action what I could only personally describe as being at the right place at the right time.

| 15 May 2025
The response to Tropical Cyclone Yasa: Through the eyes of a humanitarian surge member
Sera Vulavou is the Senior Monitoring and Evaluation Officer with IPPF’s Sub-Regional Office for the Pacific. She was trained as a humanitarian surge roster member in early 2020, to be able to deploy to emergencies to provide technical assistance to Member Associations – here she shares her experience with us. Severe Tropical Cyclone (TC) Yasa was the strongest in the South Pacific since TC Winston in 2016, as well as the fourth most intense TC on record in the basin. The Reproductive and Family Health Association of Fiji (RFHAF) humanitarian response to TC Yasa has reached some of the most difficult and geographically scattered islands and communities, which included the islands of Moala, Totoya, and Matuku. Being part of the IPPF humanitarian surge roster team gave me the opportunity to accompany the RFHAF response team during their humanitarian work. This experience was about putting in action what I could only personally describe as being at the right place at the right time.

| 23 September 2020
In pictures: Innovating during COVID-19
Women around the world have faced multiple barriers to accessing safe abortion care during the COVID-19 pandemic including the de-prioritization of sexual and reproductive healthcare, overwhelmed health systems and restrictions on movement. The COVID-19 crisis has sparked innovation among IPPF Member Associations who responded swiftly by developing new approaches to reach women with safe abortion care including telemedicine and home-based provision of medical abortion. Strong evidence generated from this work supports the continuation and strengthening of these approaches beyond the end of the pandemic. Cameroon Cameroon National Planning Association for Family Welfare (CAMNAFAW) To ensure that quality abortion care can be provided to women during travel restrictions, CAMNAFAW’s service providers travel to partner clinics in underserved areas and to clients’ homes to provide medical and surgical abortion care. This model of taking safe abortion care closer to women will continue even with easing of travel restrictions, as this has been found to be an effective and acceptable approach to increasing access.Photo: IPPF/Xaume Olleros/Cameroon Share on Twitter Share on Facebook Share via WhatsApp Share via Email Guinea Association Guinéenne pour le Bien-Etre Familial (AGBEF) Building on lessons learned during the Ebola crisis in Guinea, AGBEF quickly took measures to prevent infection in its clinics to continue providing sexual and reproductive healthcare, including surgical and medical abortion, in a safe environment. AGBEF donated protective materials to communities, including hand-washing stations, face masks and antibacterial gel, alongside messaging on infection prevention. This community visibility reassures clients they can safely attend AGBEF clinics for abortion and contraceptive care.Photo: AGBEF/Guinea Share on Twitter Share on Facebook Share via WhatsApp Share via Email India Family Planning Association of India (FPA India) FPA India and partners advocated to have sexual and reproductive healthcare, including abortion, recognized as essential by the government, which meant FPA India could continue healthcare delivery during the national lockdown. To reduce in-person clinic visits, FPA India established teleconsultation and counselling for abortion care, and is continuing to provide in-clinic care for both medical and surgical abortion. Photo: IPPF/Alison Joyce/India Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nepal Family Planning Association of Nepal (FPAN) FPAN and partners advocated for interim approval of home provision of medical abortion and telemedicine for abortion counselling during COVID-19. FPAN is now implementing these approaches, ensuring continued access to abortion care in Nepal, where many people live in remote locations with limited mobility, which has been further restricted by COVID-19 lockdowns. Photo: FPAN/Nepal Share on Twitter Share on Facebook Share via WhatsApp Share via Email Pakistan Rahnuma – Family Planning Association of Pakistan (Rahnuma-FPAP) Rahnuma-FPAP and partners successfully advocated for the government to class sexual and reproductive healthcare as ‘essential’, which enabled the team to continue providing post-abortion care during the pandemic. Rahnuma-FPAP expanded its telemedicine and home-based provision for menstrual regulation counselling and post-abortion care. These new approaches have ensured continued access to services for clients unable to reach clinics.Photo: Rahnuma-FPAP/Pakistan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Palestine Palestinian Family Planning and Protection Association (PFPPA) In response to the government-mandated closure of its clinics, PFPPA quickly established a toll-free call centre which provides consultations, counselling, referrals and follow-up, including consultation for abortion care through a harm reduction approach, ensuring that women are provided with accurate information. Due to its success, PFPPA is exploring options for continuing this healthcare delivery model beyond the pandemic, with the aim of keeping it free of charge for users.Photo: SAAF/Samar Hazboun/Palestine Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sudan Sudan Family Planning Association (SFPA) Following a nation-wide shutdown in April, SFPA established a call centre to increase access to healthcare, including abortion and contraceptive counselling and referrals. An unexpected outcome of the new call centre is that it has reached an increased number of young women who regularly call to discuss their reproductive health and rights. SFPA is working towards institutionalizing this model for continuation beyond the pandemic.Photo: SFPA/Sudan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Togo Association Togolaise pour le Bien-Etre Familial (ATBEF) ATBEF adapted its mobile application ‘Infos Ado Jeunes’, adding a toll-free teleconsultation service for young clients to use to access abortion consultations and pre- and post-abortion counselling. This app has given young clients ongoing access to care when they face challenges travelling to clinics. It has also eased overall client flow in clinics at a time when social distancing is being implemented.Photo: ATBEF/Togo Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 15 May 2025
In pictures: Innovating during COVID-19
Women around the world have faced multiple barriers to accessing safe abortion care during the COVID-19 pandemic including the de-prioritization of sexual and reproductive healthcare, overwhelmed health systems and restrictions on movement. The COVID-19 crisis has sparked innovation among IPPF Member Associations who responded swiftly by developing new approaches to reach women with safe abortion care including telemedicine and home-based provision of medical abortion. Strong evidence generated from this work supports the continuation and strengthening of these approaches beyond the end of the pandemic. Cameroon Cameroon National Planning Association for Family Welfare (CAMNAFAW) To ensure that quality abortion care can be provided to women during travel restrictions, CAMNAFAW’s service providers travel to partner clinics in underserved areas and to clients’ homes to provide medical and surgical abortion care. This model of taking safe abortion care closer to women will continue even with easing of travel restrictions, as this has been found to be an effective and acceptable approach to increasing access.Photo: IPPF/Xaume Olleros/Cameroon Share on Twitter Share on Facebook Share via WhatsApp Share via Email Guinea Association Guinéenne pour le Bien-Etre Familial (AGBEF) Building on lessons learned during the Ebola crisis in Guinea, AGBEF quickly took measures to prevent infection in its clinics to continue providing sexual and reproductive healthcare, including surgical and medical abortion, in a safe environment. AGBEF donated protective materials to communities, including hand-washing stations, face masks and antibacterial gel, alongside messaging on infection prevention. This community visibility reassures clients they can safely attend AGBEF clinics for abortion and contraceptive care.Photo: AGBEF/Guinea Share on Twitter Share on Facebook Share via WhatsApp Share via Email India Family Planning Association of India (FPA India) FPA India and partners advocated to have sexual and reproductive healthcare, including abortion, recognized as essential by the government, which meant FPA India could continue healthcare delivery during the national lockdown. To reduce in-person clinic visits, FPA India established teleconsultation and counselling for abortion care, and is continuing to provide in-clinic care for both medical and surgical abortion. Photo: IPPF/Alison Joyce/India Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nepal Family Planning Association of Nepal (FPAN) FPAN and partners advocated for interim approval of home provision of medical abortion and telemedicine for abortion counselling during COVID-19. FPAN is now implementing these approaches, ensuring continued access to abortion care in Nepal, where many people live in remote locations with limited mobility, which has been further restricted by COVID-19 lockdowns. Photo: FPAN/Nepal Share on Twitter Share on Facebook Share via WhatsApp Share via Email Pakistan Rahnuma – Family Planning Association of Pakistan (Rahnuma-FPAP) Rahnuma-FPAP and partners successfully advocated for the government to class sexual and reproductive healthcare as ‘essential’, which enabled the team to continue providing post-abortion care during the pandemic. Rahnuma-FPAP expanded its telemedicine and home-based provision for menstrual regulation counselling and post-abortion care. These new approaches have ensured continued access to services for clients unable to reach clinics.Photo: Rahnuma-FPAP/Pakistan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Palestine Palestinian Family Planning and Protection Association (PFPPA) In response to the government-mandated closure of its clinics, PFPPA quickly established a toll-free call centre which provides consultations, counselling, referrals and follow-up, including consultation for abortion care through a harm reduction approach, ensuring that women are provided with accurate information. Due to its success, PFPPA is exploring options for continuing this healthcare delivery model beyond the pandemic, with the aim of keeping it free of charge for users.Photo: SAAF/Samar Hazboun/Palestine Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sudan Sudan Family Planning Association (SFPA) Following a nation-wide shutdown in April, SFPA established a call centre to increase access to healthcare, including abortion and contraceptive counselling and referrals. An unexpected outcome of the new call centre is that it has reached an increased number of young women who regularly call to discuss their reproductive health and rights. SFPA is working towards institutionalizing this model for continuation beyond the pandemic.Photo: SFPA/Sudan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Togo Association Togolaise pour le Bien-Etre Familial (ATBEF) ATBEF adapted its mobile application ‘Infos Ado Jeunes’, adding a toll-free teleconsultation service for young clients to use to access abortion consultations and pre- and post-abortion counselling. This app has given young clients ongoing access to care when they face challenges travelling to clinics. It has also eased overall client flow in clinics at a time when social distancing is being implemented.Photo: ATBEF/Togo Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 13 August 2020
In pictures: Delivering healthcare to remote communities in Fiji
In early April 2020, the all too familiar destruction of a Tropical Cyclone (TC) – Harold – hit the Solomon Islands, Vanuatu, Fiji and Tonga. One of the worst affected areas was the Eastern part of Fiji. Through support by Department of Foreign Affairs and Trade (DFAT), our Member Association, Reproductive and Family Health Association of Fiji (RFHAF), was quick to respond ensuring access to essential sexual and reproductive healthcare for Kadavu’s women, girls, and vulnerable groups. Fiji's vulnerable coastline Fiji’s worst affected area was the Eastern part, with TC Harold bringing destructive storm force winds and storm surge. RFHAF focused its humanitarian response on the local Kadavu population. This remote area proves a challenge to reach for the team with supplies. Share on Twitter Share on Facebook Share via WhatsApp Share via Email RFHAF's humanitarian response team tackle rough terrain National travel restrictions - due to the current COVID-19 pandemic - on all inter island transfers has slowed the response in some areas, including Kadavu. The island of Kadavu is one of the least developed areas of Fiji, the main source of income is substance living (Yaqona). Transport around the island is difficult, with very few roads, no public water system or electricity. The humanitarian team from RFHAF travels by boat and then on foot. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Asenaca, client Kadavu, the biggest island in the Eastern division has the greatest population (10,897). 197 evacuation centres were activated in total, initially hosting over 6,240 people. Many are women of reproductive age, with an estimated 150 currently pregnant. Asenaca learns about breast cancer self-checks from RFHAF’s healthcare provider, Karo. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nasi, RFHAF healthcare provider The medical mobile team deliver a broad range of healthcare including contraception, information and counselling on sexual health, pregnancy, HIV and STI care and testing. RFHAF Team in Kadavu performing general health checks after TC Harold. Nasi administers a HPV shot to a client. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Kate, client Young women and girls are at the heart of RFHAF’s healthcare provision. Kate walks home with her dignity kit after a health check at the mobile clinic. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Karo, RFHAF healthcare worker RFHAF offers sexual and reproductive healthcare as well as counselling, and referrals for follow up care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Alidi, RFHAF healthcare worker The team ensures young people in the community are not forgotten and provide information and education on relationships and sexual health and rights. Alidi conducting a session with a local group of young people at Gasele, Kadavu.Photos ©IPPF/Rob Rickman/Fiji Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 15 May 2025
In pictures: Delivering healthcare to remote communities in Fiji
In early April 2020, the all too familiar destruction of a Tropical Cyclone (TC) – Harold – hit the Solomon Islands, Vanuatu, Fiji and Tonga. One of the worst affected areas was the Eastern part of Fiji. Through support by Department of Foreign Affairs and Trade (DFAT), our Member Association, Reproductive and Family Health Association of Fiji (RFHAF), was quick to respond ensuring access to essential sexual and reproductive healthcare for Kadavu’s women, girls, and vulnerable groups. Fiji's vulnerable coastline Fiji’s worst affected area was the Eastern part, with TC Harold bringing destructive storm force winds and storm surge. RFHAF focused its humanitarian response on the local Kadavu population. This remote area proves a challenge to reach for the team with supplies. Share on Twitter Share on Facebook Share via WhatsApp Share via Email RFHAF's humanitarian response team tackle rough terrain National travel restrictions - due to the current COVID-19 pandemic - on all inter island transfers has slowed the response in some areas, including Kadavu. The island of Kadavu is one of the least developed areas of Fiji, the main source of income is substance living (Yaqona). Transport around the island is difficult, with very few roads, no public water system or electricity. The humanitarian team from RFHAF travels by boat and then on foot. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Asenaca, client Kadavu, the biggest island in the Eastern division has the greatest population (10,897). 197 evacuation centres were activated in total, initially hosting over 6,240 people. Many are women of reproductive age, with an estimated 150 currently pregnant. Asenaca learns about breast cancer self-checks from RFHAF’s healthcare provider, Karo. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nasi, RFHAF healthcare provider The medical mobile team deliver a broad range of healthcare including contraception, information and counselling on sexual health, pregnancy, HIV and STI care and testing. RFHAF Team in Kadavu performing general health checks after TC Harold. Nasi administers a HPV shot to a client. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Kate, client Young women and girls are at the heart of RFHAF’s healthcare provision. Kate walks home with her dignity kit after a health check at the mobile clinic. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Karo, RFHAF healthcare worker RFHAF offers sexual and reproductive healthcare as well as counselling, and referrals for follow up care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Alidi, RFHAF healthcare worker The team ensures young people in the community are not forgotten and provide information and education on relationships and sexual health and rights. Alidi conducting a session with a local group of young people at Gasele, Kadavu.Photos ©IPPF/Rob Rickman/Fiji Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 15 February 2019
"I’m so happy I now don’t have to worry about contraception for another five years”
In August 2017, weeks of continued and heavy rainfall across Nepal resulted in flash floods and landslides that affected 36 of the 75 districts. Many people lost their homes or were displaced. It was estimated that of those affected, 112,500 were women of reproductive age, including 8,694 pregnant women. IPPF Humanitarian, through their Member Association, The Family Planning Association of Nepal (FPAN), activated its emergency response system early on. With funding support from the Australian Government, FPAN and IPPF Humanitarian initially mobilised their response in four of the worst affected districts (Sunsari, Saptari, Bardiya, and Dang). Mobile medical camps were established to meet the sexual and reproductive health needs of the affected population, including through the distribution of short and long acting methods of contraception, STI and HIV screening, and GBV referrals. In collaboration with the USAID-SIFPO project, services were then expanded into five more affected districts. IPPF Humanitarian spoke with 21-year old Muna in her home district of Sunsari in Nepal. “I got married at 16 years old and have two children, a four-year-old girl and two-year-old boy. In my caste, we get married early, so my parents took me to get an arranged marriage. I was in the 8th class at the time, and returned to school after I got married, but only lasted one year. My husband works in construction and had to stop working for two weeks when the floods came. When he doesn’t work, he doesn’t get paid, so it’s been very difficult. A FPAN social worker told me about the mobile medical camp today. I used to be on the three-month injectable but today I changed to the five-year implant in my arm. When my youngest child was eight months old I found out I was pregnant again. I decided to discontinue that pregnancy, so I took the five small tablets given to me by my neighbourhood doctor. I was two months pregnant at the time. From this, I had two days bleeding and cramp like pain, and then weakness. I decided to abort that pregnancy because my youngest will still only eight months old, and I didn’t want any more children. If I had more than two children, it would be very difficult to feed and educate them, and would badly affect my body too. I’m so happy I now don’t have to worry about contraception for another five years.” Want to know more about safe abortion access? Join IPPF'S I Decide movement

| 15 May 2025
"I’m so happy I now don’t have to worry about contraception for another five years”
In August 2017, weeks of continued and heavy rainfall across Nepal resulted in flash floods and landslides that affected 36 of the 75 districts. Many people lost their homes or were displaced. It was estimated that of those affected, 112,500 were women of reproductive age, including 8,694 pregnant women. IPPF Humanitarian, through their Member Association, The Family Planning Association of Nepal (FPAN), activated its emergency response system early on. With funding support from the Australian Government, FPAN and IPPF Humanitarian initially mobilised their response in four of the worst affected districts (Sunsari, Saptari, Bardiya, and Dang). Mobile medical camps were established to meet the sexual and reproductive health needs of the affected population, including through the distribution of short and long acting methods of contraception, STI and HIV screening, and GBV referrals. In collaboration with the USAID-SIFPO project, services were then expanded into five more affected districts. IPPF Humanitarian spoke with 21-year old Muna in her home district of Sunsari in Nepal. “I got married at 16 years old and have two children, a four-year-old girl and two-year-old boy. In my caste, we get married early, so my parents took me to get an arranged marriage. I was in the 8th class at the time, and returned to school after I got married, but only lasted one year. My husband works in construction and had to stop working for two weeks when the floods came. When he doesn’t work, he doesn’t get paid, so it’s been very difficult. A FPAN social worker told me about the mobile medical camp today. I used to be on the three-month injectable but today I changed to the five-year implant in my arm. When my youngest child was eight months old I found out I was pregnant again. I decided to discontinue that pregnancy, so I took the five small tablets given to me by my neighbourhood doctor. I was two months pregnant at the time. From this, I had two days bleeding and cramp like pain, and then weakness. I decided to abort that pregnancy because my youngest will still only eight months old, and I didn’t want any more children. If I had more than two children, it would be very difficult to feed and educate them, and would badly affect my body too. I’m so happy I now don’t have to worry about contraception for another five years.” Want to know more about safe abortion access? Join IPPF'S I Decide movement

| 29 November 2017
Meet the college student who uses his music to battle the stigma surrounding HIV
Milan Khadka was just ten years old when he lost both his parents to HIV. “When I lost my parents, I used to feel so alone, like I didn’t have anyone in the world,” he says. “Whenever I saw other children getting love from others, I used to feel that I also might get that kind of love if I hadn’t lost my parents.” Like thousands of Nepali children, Milan’s parents left Nepal for India in search of work. Milan grew up in India until he was ten, when his mother died of AIDS-related causes. The family then returned to Nepal, but just eight months later, his father also died, and Milan was left in the care of his grandmother. “After I lost my parents, I went for VCT [voluntary counselling and testing] to check if I had HIV in my body,” Milan says. “After I was diagnosed as HIV positive, slowly all the people in the area found out about my status and there was so much discrimination. My friends at school didn’t want to sit with me and they humiliated and bullied me,” he says. “At home, I had a separate sleeping area and sleeping materials, separate dishes and a separate comb for my hair. I had to sleep alone.” Things began to improve for Milan when he met a local woman called Lakshmi Kunwar. After discovering she was HIV-positive, Lakshmi had dedicated her life to helping people living with HIV in Palpa, working as a community home-based care mobiliser for the Family Planning Association of Nepal (FPAN) and other organisations. Struck by the plight of this small, orphaned boy, Lakshmi spoke to Milan’s family and teachers, who in turn spoke to his school mates. “After she spoke to my teachers, they started to support me,” Milan says. “And after getting information about HIV, my school friends started to like me and share things with me. And they said: ‘Milan has no one in this world, so we are the ones who must be with him. Who knows that what happened to him might not happen to us?” Lakshmi mentored him through school and college, encouraging him in his schoolwork. “Lakshmi is more than my mother,” he says. “My mother only gave birth to me but Lakshmi has looked after me all this time. Even if my mother was alive today, she might not do all the things for me that Lakshmi has done.” Milan went on to become a grade A student, regularly coming top of his class and leaving school with flying colours. Today, twenty-one-year-old Milan lives a busy and fulfilling life, juggling his college studies, his work as a community home-based care (CHBC) mobiliser for FPAN and a burgeoning music career. When not studying for a Bachelor’s of education at university in Tansen, he works as a CHBC mobiliser for FPAN, visiting villages in the area to raise awareness about how to prevent and treat HIV, and to distribute contraception. He also offers support to children living with HIV, explaining to them how he lost his parents and faced discrimination but now leads a happy and successful life. “There are 40 children in this area living with HIV,” he says. “I talk to them, collect information from them and help them get the support they need. And I tell them: ‘If I had given up at that time, I would not be like this now. So you also shouldn’t give up, and you have to live your life.” Watch Milan's story below:

| 15 May 2025
Meet the college student who uses his music to battle the stigma surrounding HIV
Milan Khadka was just ten years old when he lost both his parents to HIV. “When I lost my parents, I used to feel so alone, like I didn’t have anyone in the world,” he says. “Whenever I saw other children getting love from others, I used to feel that I also might get that kind of love if I hadn’t lost my parents.” Like thousands of Nepali children, Milan’s parents left Nepal for India in search of work. Milan grew up in India until he was ten, when his mother died of AIDS-related causes. The family then returned to Nepal, but just eight months later, his father also died, and Milan was left in the care of his grandmother. “After I lost my parents, I went for VCT [voluntary counselling and testing] to check if I had HIV in my body,” Milan says. “After I was diagnosed as HIV positive, slowly all the people in the area found out about my status and there was so much discrimination. My friends at school didn’t want to sit with me and they humiliated and bullied me,” he says. “At home, I had a separate sleeping area and sleeping materials, separate dishes and a separate comb for my hair. I had to sleep alone.” Things began to improve for Milan when he met a local woman called Lakshmi Kunwar. After discovering she was HIV-positive, Lakshmi had dedicated her life to helping people living with HIV in Palpa, working as a community home-based care mobiliser for the Family Planning Association of Nepal (FPAN) and other organisations. Struck by the plight of this small, orphaned boy, Lakshmi spoke to Milan’s family and teachers, who in turn spoke to his school mates. “After she spoke to my teachers, they started to support me,” Milan says. “And after getting information about HIV, my school friends started to like me and share things with me. And they said: ‘Milan has no one in this world, so we are the ones who must be with him. Who knows that what happened to him might not happen to us?” Lakshmi mentored him through school and college, encouraging him in his schoolwork. “Lakshmi is more than my mother,” he says. “My mother only gave birth to me but Lakshmi has looked after me all this time. Even if my mother was alive today, she might not do all the things for me that Lakshmi has done.” Milan went on to become a grade A student, regularly coming top of his class and leaving school with flying colours. Today, twenty-one-year-old Milan lives a busy and fulfilling life, juggling his college studies, his work as a community home-based care (CHBC) mobiliser for FPAN and a burgeoning music career. When not studying for a Bachelor’s of education at university in Tansen, he works as a CHBC mobiliser for FPAN, visiting villages in the area to raise awareness about how to prevent and treat HIV, and to distribute contraception. He also offers support to children living with HIV, explaining to them how he lost his parents and faced discrimination but now leads a happy and successful life. “There are 40 children in this area living with HIV,” he says. “I talk to them, collect information from them and help them get the support they need. And I tell them: ‘If I had given up at that time, I would not be like this now. So you also shouldn’t give up, and you have to live your life.” Watch Milan's story below:

| 12 September 2017
"I said to myself: I will live and I will let others living with HIV live"
Lakshmi Kunwar married young, at the age of 17. Shortly afterwards, Lakshmi’s husband, who worked as a migrant labourer in India, was diagnosed with HIV and died. “At that time, I was completely unaware of HIV,” Lakshmi says. “My husband had information that if someone is diagnosed with HIV, they will die very soon. So after he was diagnosed, he didn’t eat anything and he became very ill and after six months he died. He gave up.” Lakshmi contracted HIV too, and the early years of living with it were arduous. “It was a huge burden,” she says. “I didn’t want to eat anything so I ate very little. My weight at the time was 44 kilograms. I had different infections in my skin and allergies in her body. It was really a difficult time for me. … I was just waiting for my death. I got support from my home and in-laws but my neighbours started to discriminate against me – like they said HIV may transfer via different insects and parasites like lice.” Dedicating her life to help others Lakshmi’s life began to improve when she came across an organisation in Palpa that offered support to people living with HIV (PLHIV). “They told me that there is medicine for PLHIV which will prolong our lives,” she explains. “They took me to Kathmandu, where I got training and information on HIV and I started taking ARVs [antiretroviral drugs].” In Kathmandu Lakshmi decided that she would dedicate the rest of her life to supporting people living with HIV. “I made a plan that I would come back home [to Palpa], disclose my status and then do social work with other people living with HIV, so that they too may have hope to live. I said to myself: I will live and I will let others living with HIV live”. Stories Read more stories about our work with people living with HIV

| 15 May 2025
"I said to myself: I will live and I will let others living with HIV live"
Lakshmi Kunwar married young, at the age of 17. Shortly afterwards, Lakshmi’s husband, who worked as a migrant labourer in India, was diagnosed with HIV and died. “At that time, I was completely unaware of HIV,” Lakshmi says. “My husband had information that if someone is diagnosed with HIV, they will die very soon. So after he was diagnosed, he didn’t eat anything and he became very ill and after six months he died. He gave up.” Lakshmi contracted HIV too, and the early years of living with it were arduous. “It was a huge burden,” she says. “I didn’t want to eat anything so I ate very little. My weight at the time was 44 kilograms. I had different infections in my skin and allergies in her body. It was really a difficult time for me. … I was just waiting for my death. I got support from my home and in-laws but my neighbours started to discriminate against me – like they said HIV may transfer via different insects and parasites like lice.” Dedicating her life to help others Lakshmi’s life began to improve when she came across an organisation in Palpa that offered support to people living with HIV (PLHIV). “They told me that there is medicine for PLHIV which will prolong our lives,” she explains. “They took me to Kathmandu, where I got training and information on HIV and I started taking ARVs [antiretroviral drugs].” In Kathmandu Lakshmi decided that she would dedicate the rest of her life to supporting people living with HIV. “I made a plan that I would come back home [to Palpa], disclose my status and then do social work with other people living with HIV, so that they too may have hope to live. I said to myself: I will live and I will let others living with HIV live”. Stories Read more stories about our work with people living with HIV

| 08 September 2017
“Attitudes of younger people to HIV are not changing fast"
“When I was 14, I was trafficked to India,” says 35-year-old Lakshmi Lama. “I was made unconscious and was taken to Mumbai. When I woke up, I didn’t even know that I had been trafficked, I didn’t know where I was.” Every year, thousands of Nepali women and girls are trafficked to India, some lured with the promise of domestic work only to find themselves in brothels or working as sex slaves. The visa-free border with India means the actual number of women and girls trafficked from Nepal is likely to be much higher. The earthquake of April 2015 also led to a surge in trafficking: women and girls living in tents or temporary housing, and young orphaned children were particularly vulnerable to traffickers. “I was in Mumbai for three years,” says Lakshmi. “Then I managed to send letters and photographs to my parents and eventually they came to Mumbai and helped rescue me from that place". During her time in India, Lakshmi contracted HIV. Life after her diagnosis was tough, Lakshmi explains. “When I was diagnosed with HIV, people used to discriminate saying, “you’ve got HIV and it might transfer to us so don’t come to our home, don’t touch us,’” she says. “It’s very challenging for people living with HIV in Nepal. People really suffer.” Today, Lakshmi lives in Banepa, a busy town around 25 kilometres east of Kathmandu. Things began to improve for her, she says, when she started attending HIV awareness classes run by Family Planning Association of Nepal (FPAN). Eventually she herself trained as an FPAN peer educator, and she now works hard visiting communities in Kavre, raising awareness about HIV prevention and treatment, and bringing people together to tackle stigma around the virus. The government needs to do far more to tackle HIV stigma in Nepal, particularly at village level, Lakshmi says, “Attitudes of younger people to HIV are not changing fast. People still say to me: ‘you have HIV, you may die soon’. There is so much stigma and discrimination in this community.” Stories Read more stories about our work with people living with HIV

| 15 May 2025
“Attitudes of younger people to HIV are not changing fast"
“When I was 14, I was trafficked to India,” says 35-year-old Lakshmi Lama. “I was made unconscious and was taken to Mumbai. When I woke up, I didn’t even know that I had been trafficked, I didn’t know where I was.” Every year, thousands of Nepali women and girls are trafficked to India, some lured with the promise of domestic work only to find themselves in brothels or working as sex slaves. The visa-free border with India means the actual number of women and girls trafficked from Nepal is likely to be much higher. The earthquake of April 2015 also led to a surge in trafficking: women and girls living in tents or temporary housing, and young orphaned children were particularly vulnerable to traffickers. “I was in Mumbai for three years,” says Lakshmi. “Then I managed to send letters and photographs to my parents and eventually they came to Mumbai and helped rescue me from that place". During her time in India, Lakshmi contracted HIV. Life after her diagnosis was tough, Lakshmi explains. “When I was diagnosed with HIV, people used to discriminate saying, “you’ve got HIV and it might transfer to us so don’t come to our home, don’t touch us,’” she says. “It’s very challenging for people living with HIV in Nepal. People really suffer.” Today, Lakshmi lives in Banepa, a busy town around 25 kilometres east of Kathmandu. Things began to improve for her, she says, when she started attending HIV awareness classes run by Family Planning Association of Nepal (FPAN). Eventually she herself trained as an FPAN peer educator, and she now works hard visiting communities in Kavre, raising awareness about HIV prevention and treatment, and bringing people together to tackle stigma around the virus. The government needs to do far more to tackle HIV stigma in Nepal, particularly at village level, Lakshmi says, “Attitudes of younger people to HIV are not changing fast. People still say to me: ‘you have HIV, you may die soon’. There is so much stigma and discrimination in this community.” Stories Read more stories about our work with people living with HIV

| 08 September 2017
'My neighbours used to discriminate against me and I suffered violence at the hands of my community'
"My husband used to work in India, and when he came back, he got ill and died," says Durga Thame. "We didn’t know that he was HIV-positive, but then then later my daughter got sick with typhoid and went to hospital and was diagnosed with HIV and died, and then I was tested and was found positive." Her story is tragic, but one all too familiar for the women living in this region. Men often travel to India in search of work, where they contract HIV and upon their return infect their wives. For Durga, the death of her husband and daughter and her own HIV positive diagnosis threw her into despair. "My neighbours used to discriminate against me … and I suffered violence at the hands of my community. Everybody used to say that they couldn’t eat whatever I cooked because they might get HIV." Then Durga heard about HIV education classes run by the Palpa branch of the Family Planning Association of Nepal (FPAN), a short bus journey up the road in Tansen, the capital of Palpa. "At those meetings, I got information about HIV," she says. "When I came back to my village, I began telling my neighbours about HIV. They came to know the facts and they realised it was a myth that HIV could be transferred by sharing food. Then they began treating me well." FPAN ran nutrition, hygiene, sanitation and livelihood classes that helped Durga turn the fortunes of her small homestead around. Durga sells goats and hens, and with these earnings supports her family – her father-in-law and her surviving daughter, who she says has not yet been tested for HIV. "I want to educate my daughter," she says. "I really hope I can provide a better education for her." Stories Read more stories about our work with people living with HIV

| 15 May 2025
'My neighbours used to discriminate against me and I suffered violence at the hands of my community'
"My husband used to work in India, and when he came back, he got ill and died," says Durga Thame. "We didn’t know that he was HIV-positive, but then then later my daughter got sick with typhoid and went to hospital and was diagnosed with HIV and died, and then I was tested and was found positive." Her story is tragic, but one all too familiar for the women living in this region. Men often travel to India in search of work, where they contract HIV and upon their return infect their wives. For Durga, the death of her husband and daughter and her own HIV positive diagnosis threw her into despair. "My neighbours used to discriminate against me … and I suffered violence at the hands of my community. Everybody used to say that they couldn’t eat whatever I cooked because they might get HIV." Then Durga heard about HIV education classes run by the Palpa branch of the Family Planning Association of Nepal (FPAN), a short bus journey up the road in Tansen, the capital of Palpa. "At those meetings, I got information about HIV," she says. "When I came back to my village, I began telling my neighbours about HIV. They came to know the facts and they realised it was a myth that HIV could be transferred by sharing food. Then they began treating me well." FPAN ran nutrition, hygiene, sanitation and livelihood classes that helped Durga turn the fortunes of her small homestead around. Durga sells goats and hens, and with these earnings supports her family – her father-in-law and her surviving daughter, who she says has not yet been tested for HIV. "I want to educate my daughter," she says. "I really hope I can provide a better education for her." Stories Read more stories about our work with people living with HIV

| 21 August 2017
How youth volunteers are leading the conversation on HIV with young people in Nepal
Mala Neupane is just 18 years old, but is already an experienced volunteer for the Family Planning Association of Nepal (FPAN). Mala lives in Tansen, the hillside capital of Palpa, a region of rolling hills, pine forests and lush terraced fields in western Nepal. She works as a community home-based care mobiliser focusing on HIV: her job involves travelling to villages around Tansen to provide people with information about HIV and contraception. “Before, the community had very little knowledge regarding HIV and there used to be so much stigma and discrimination,” she says. “But later, when the Community Health Based Carers (CHBCs) started working in those communities, they had more knowledge and less stigma.” The youth of the volunteers proved an effective tool during their conversations with villagers. “At first, when they talked to people about family planning, they were not receptive: they felt resistance to using those devices,” Mala explains. “The CHBCs said to them: ‘young people like us are doing this kind of work, so why are you feeling such hesitation?’ After talking with them, they became ready to use contraceptives.” Her age is also important for connecting with young people, in a society of rapid change, she says. “Because we are young, we may know more about what young people’s needs and wants are. We can talk to young people about what family planning methods might be suitable for them, and what the options are.” “Young people’s involvement [in FPAN programmes] is very important to helping out young people like us.” It’s a simple message, but one reaping rich rewards for the lives and wellbeing of people in Palpa.

| 15 May 2025
How youth volunteers are leading the conversation on HIV with young people in Nepal
Mala Neupane is just 18 years old, but is already an experienced volunteer for the Family Planning Association of Nepal (FPAN). Mala lives in Tansen, the hillside capital of Palpa, a region of rolling hills, pine forests and lush terraced fields in western Nepal. She works as a community home-based care mobiliser focusing on HIV: her job involves travelling to villages around Tansen to provide people with information about HIV and contraception. “Before, the community had very little knowledge regarding HIV and there used to be so much stigma and discrimination,” she says. “But later, when the Community Health Based Carers (CHBCs) started working in those communities, they had more knowledge and less stigma.” The youth of the volunteers proved an effective tool during their conversations with villagers. “At first, when they talked to people about family planning, they were not receptive: they felt resistance to using those devices,” Mala explains. “The CHBCs said to them: ‘young people like us are doing this kind of work, so why are you feeling such hesitation?’ After talking with them, they became ready to use contraceptives.” Her age is also important for connecting with young people, in a society of rapid change, she says. “Because we are young, we may know more about what young people’s needs and wants are. We can talk to young people about what family planning methods might be suitable for them, and what the options are.” “Young people’s involvement [in FPAN programmes] is very important to helping out young people like us.” It’s a simple message, but one reaping rich rewards for the lives and wellbeing of people in Palpa.