Spotlight
A selection of stories from across the Federation

Advances in Sexual and Reproductive Rights and Health: 2024 in Review
Let’s take a leap back in time to the beginning of 2024: In twelve months, what victories has our movement managed to secure in the face of growing opposition and the rise of the far right? These victories for sexual and reproductive rights and health are the result of relentless grassroots work and advocacy by our Member Associations, in partnership with community organizations, allied politicians, and the mobilization of public opinion.
Most Popular This Week

Advances in Sexual and Reproductive Rights and Health: 2024 in Review
Let’s take a leap back in time to the beginning of 2024: In twelve months, what victories has our movement managed to secure in t
Kazakhstan

Kazakhstan's Rising HIV Crisis: A Call for Action
On World AIDS Day, we commemorate the remarkable achievements of IPPF Member Associations in their unwavering commitment to combating the HIV epidemic.

Ensuring SRHR in Humanitarian Crises: What You Need to Know
Over the past two decades, global forced displacement has consistently increased, affecting an estimated 114 million people as of mid-2023.
Estonia, Nepal, Namibia, Japan, Thailand

The Rainbow Wave for Marriage Equality
Love wins! The fight for marriage equality has seen incredible progress worldwide, with a recent surge in legalizations.
France, Germany, Poland, United Kingdom, United States, Colombia, India, Tunisia

Abortion Rights: Latest Decisions and Developments around the World
Over the past 30 years, more than

Palestine

In their own words: The people providing sexual and reproductive health care under bombardment in Gaza
Week after week, heavy Israeli bombardment from air, land, and sea, has continued across most of the Gaza Strip.
Vanuatu

When getting to the hospital is difficult, Vanuatu mobile outreach can save lives
In the mountains of Kumera on Tanna Island, Vanuatu, the village women of Kamahaul normally spend over 10,000 Vatu ($83 USD) to travel to the nearest hospital.
Filter our stories by:
- Afghanistan
- Albania
- Aruba
- Bangladesh
- Benin
- Botswana
- Burundi
- Cambodia
- (-) Cameroon
- Colombia
- Congo, Dem. Rep.
- Cook Islands
- El Salvador
- Estonia
- Ethiopia
- Fiji
- France
- Germany
- Ghana
- Guinea-Conakry
- India
- Ireland
- Jamaica
- Japan
- Kazakhstan
- Kenya
- Kiribati
- Lesotho
- Malawi
- Mali
- Mozambique
- Namibia
- Nepal
- Nigeria
- Pakistan
- Palestine
- Poland
- Senegal
- Somaliland
- Sri Lanka
- Sudan
- Thailand
- Togo
- Tonga
- (-) Trinidad and Tobago
- Tunisia
- Uganda
- United Kingdom
- United States
- Vanuatu
- Zambia


| 24 June 2021
Changing mindsets through medicine and motivation
“You work with people who have HIV? Why?” That was the question Dr. Gregory Boyce was asked by the young intern that stood before him. He had come to the hospital ward to visit a client who was known to be living with HIV. He approached the intern at the desk and gave his name and designation. The intern looked at him, confused and somewhat amused and asked the question that he has neither forgotten, nor understood to this day. However, this young intern’s question comes from a mindset that Dr. Boyce is working fervently to change. As Deputy Director of the Medical Research Foundation of Trinidad and Tobago (MRF), Dr. Boyce provides clinical and administrative support to a team of doctors and nurses providing care to their clients who are living with HIV. Due to MRF’s long-standing work in HIV research and healthcare, the Family Planning Association of Trinidad and Tobago (FPATT), has referred many clients to Dr. Boyce and his team, and especially clients from the LGBTI+ community. Providing specialist care and support “Persons coming to us from key populations, have very layered needs. They are facing unique challenges in addition to living with the virus. There is still that myth that being HIV positive means that you will positively die. Added to that, there’s the discrimination that the community faces in every aspect of their lives on a daily basis. As a staff, we’ve had to seek special training to guide the way we interact with these clients so that we can meet all their needs appropriately and sensitively,” explains Dr. Boyce. “Apart from medical interventions which are needed to ensure that our clients continue to live healthy lives, we focus heavily on their psychosocial needs. It’s easy to think that because a client is physically healthy that they are also emotionally healthy. We have clients that won’t leave abusive relationships because they think no one else would accept them. We have other clients that are dealing with long-term medication fatigue because they have been taking pills for over 10 years. With that sometimes comes depression and other drug addictions, which is why it’s necessary for us to maintain open and honest relationships to address those accompanying issues.” Making HIV a non-issue Dr Boyce has been committed to providing treatment and care to clients living with HIV for over 20 years. He had worked at the Port of Spain General Hospital after graduating, during which time, medicine for persons living with HIV was expensive and out of reach for many. A few years later, through government programmes, medicine became more affordable, and treatment centres were opening up across the island. However, Dr. Boyce realized that the mortality rate had not changed by much. He wondered why people were still dying from a virus when medicine was easily accessible. “That first conversation – giving a client the news that they’ve tested positive – is very important. We get to show them that HIV is not an impediment. Most times, with the wrong information, they start to draw up a list of things that they can no longer do, like go after a promotion or start a family. Then they go through life shrunken and unrecognizable, not the person they once were. So to answer that intern’s question about why I work with persons living with HIV: I want to make HIV a non-issue,” he states. Dr. Boyce hopes to see HIV disclosure become as acceptable as other chronic illnesses such as cancer or diabetes, where an entire family would work towards caring for the affected person, instead of alienating them. He also hopes to see more inclusion and tolerance towards persons living with HIV, especially those within the LGBTI+ community. “Until a gay or transgender person can walk the streets freely and not be jeered at by passers-by, we still have a long way to go. Until they can access treatment at any public facility without fear or judgment, we have a lot of work to do. It would take a lot of education to change the stigma and discrimination but there is absolutely no reason why another person’s life should be miserable because their expression is different to ours.” He commends the work of FPATT in upholding the sexual and reproductive health and rights of the LGBTI+ community, through ensuring that they have a safe and non-judgmental environment for treatment and care. He says that the Medical Research Foundation values the great relationship that the two organizations have had for years, even as FPATT works towards becoming its own full-service antiretroviral treatment site for persons living with HIV.

| 17 May 2025
Changing mindsets through medicine and motivation
“You work with people who have HIV? Why?” That was the question Dr. Gregory Boyce was asked by the young intern that stood before him. He had come to the hospital ward to visit a client who was known to be living with HIV. He approached the intern at the desk and gave his name and designation. The intern looked at him, confused and somewhat amused and asked the question that he has neither forgotten, nor understood to this day. However, this young intern’s question comes from a mindset that Dr. Boyce is working fervently to change. As Deputy Director of the Medical Research Foundation of Trinidad and Tobago (MRF), Dr. Boyce provides clinical and administrative support to a team of doctors and nurses providing care to their clients who are living with HIV. Due to MRF’s long-standing work in HIV research and healthcare, the Family Planning Association of Trinidad and Tobago (FPATT), has referred many clients to Dr. Boyce and his team, and especially clients from the LGBTI+ community. Providing specialist care and support “Persons coming to us from key populations, have very layered needs. They are facing unique challenges in addition to living with the virus. There is still that myth that being HIV positive means that you will positively die. Added to that, there’s the discrimination that the community faces in every aspect of their lives on a daily basis. As a staff, we’ve had to seek special training to guide the way we interact with these clients so that we can meet all their needs appropriately and sensitively,” explains Dr. Boyce. “Apart from medical interventions which are needed to ensure that our clients continue to live healthy lives, we focus heavily on their psychosocial needs. It’s easy to think that because a client is physically healthy that they are also emotionally healthy. We have clients that won’t leave abusive relationships because they think no one else would accept them. We have other clients that are dealing with long-term medication fatigue because they have been taking pills for over 10 years. With that sometimes comes depression and other drug addictions, which is why it’s necessary for us to maintain open and honest relationships to address those accompanying issues.” Making HIV a non-issue Dr Boyce has been committed to providing treatment and care to clients living with HIV for over 20 years. He had worked at the Port of Spain General Hospital after graduating, during which time, medicine for persons living with HIV was expensive and out of reach for many. A few years later, through government programmes, medicine became more affordable, and treatment centres were opening up across the island. However, Dr. Boyce realized that the mortality rate had not changed by much. He wondered why people were still dying from a virus when medicine was easily accessible. “That first conversation – giving a client the news that they’ve tested positive – is very important. We get to show them that HIV is not an impediment. Most times, with the wrong information, they start to draw up a list of things that they can no longer do, like go after a promotion or start a family. Then they go through life shrunken and unrecognizable, not the person they once were. So to answer that intern’s question about why I work with persons living with HIV: I want to make HIV a non-issue,” he states. Dr. Boyce hopes to see HIV disclosure become as acceptable as other chronic illnesses such as cancer or diabetes, where an entire family would work towards caring for the affected person, instead of alienating them. He also hopes to see more inclusion and tolerance towards persons living with HIV, especially those within the LGBTI+ community. “Until a gay or transgender person can walk the streets freely and not be jeered at by passers-by, we still have a long way to go. Until they can access treatment at any public facility without fear or judgment, we have a lot of work to do. It would take a lot of education to change the stigma and discrimination but there is absolutely no reason why another person’s life should be miserable because their expression is different to ours.” He commends the work of FPATT in upholding the sexual and reproductive health and rights of the LGBTI+ community, through ensuring that they have a safe and non-judgmental environment for treatment and care. He says that the Medical Research Foundation values the great relationship that the two organizations have had for years, even as FPATT works towards becoming its own full-service antiretroviral treatment site for persons living with HIV.

| 24 June 2021
Ensuring care for Trinidad and Tobago's LGBTI+ community
Public perceptions, a lack of education, and government policies contribute to the barriers and challenges to achieving equality for all. In a country as diverse as Trinidad and Tobago, this is especially acute for certain key populations, including the LGBTI+ community. For Brandy Rodriguez, Healthcare Navigator at the Family Planning Association of Trinidad and Tobago (FPATT), the struggle is both real and personal. In 1999, Brandy began her transition to womanhood and since 2006 has been working with FPATT in their HIV programme for the LGBTI+ community. “Back in 2004, very little was said about HIV infection, transmission and prevention. In fact, if there was any information, it was misconstrued and meant to stigmatize the LGBTI+ community. I was fairly new to the transgender community, so I made it a mission to research and find out the truths behind HIV and how I could protect myself. I then felt like I had to share what I found with others who were searching as well,” she said. Overcoming prejudice and stigma That’s when FPATT asked Brandy to join their team in educating the LGBTI+ community on the types of healthcare available. Stigma surrounding the community forced many to stay hidden and avoid seeking care. Even if a member of the LGBTI+ community wanted to test for their HIV status, they would never dare to go into a public health centre, because of the fear of being judged by the healthcare professionals. “It’s a simple case of this. When a transgender or non-binary person walks into a health centre or hospital, and the triage nurse has to fill in a form that asks for gender, the only two options there are male and female. So usually, the non-binary person knows that if they want to access that healthcare, free of judgement, they would have to dress as the gender that would bring less attention. At the end of the day, the healthcare provider does not receive accurate information about the client, and the client doesn’t receive the scope of assessment and treatment that may be necessary. So part of what I do, is to simply accompany the client to the appointment so that it’s a less stressful experience and they don’t feel like they are alone,” says Brandy. The importance of access to HIV treatment and care Apart from a great lack of healthcare professionals that are willing to treat the LGBTI+ community non-judgementally, the community also lacks social support. Most of the members of the community face barriers to housing and employment, which often means earning a livelihood through sex work. Over 95% of skilled and employable persons within the LGBTI+ community have turned to sex work because they are constantly denied employment within other industries. “When I began my transition, I was fortunate to have the support of my family; they understood my heart and my need to be my authentic self. Not everyone has that support and so some either migrate or are left homeless because of the fact. Having to work within the sex industry means that they are now at greater risk for HIV or other STIs. My job as an Educator and Navigator is to promote condom use and ensure that they make use of FPATT’s regular HIV testing. If they do test positive, we then have that conversation about U=U, which means that if they [their HIV viral load] are undetectable, they will be untransferable, and then get them to that place of undetectability.” Brandy explains that being undetectable means that the client’s viral load is suppressed, and they are living healthy lives. The team works hard to ensure clients living with HIV enrol in the FPATT Programme, which supports the importance of adhering to consistent treatment, healthy eating, and rest. As well as testing, the Programme offers sexual and reproductive health education on prevention against STIs and both group and one-to-one sessions to anyone who needs it. Advocating for support FPATT has, for many years, advocated for the sexual and reproductive rights of the LGBTI+ community, ensuring that it remains a safe place for HIV testing and counselling. It holds a vision of a world where gender or sexuality are no longer a source of inequality or stigma. FPATT is poised to become a full-service HIV treatment site, offering antiretroviral treatment as well as psychosocial services for persons affected by HIV. FPATT’s goal is to stop discrimination and stigma against persons living with HIV and ultimately end the spread of HIV within Trinidad and Tobago by 2030. October 28, 2021 - We celebrate our much beloved colleague Brandy, LGBTQI+ Healthcare Navigator for FPATT and Trinidadian champion of human rights. She has long been a defender of the rights of LGBTQI+ people, and a pioneer in ensuring access to services while fighting stigma and discrimination in the community. We honor her dedication to equality across the Caribbean, her passionate advocacy for Trans rights. The fight continues in her powerful memory. Conmemoramos a nuestra querida colega Brandy, defensora por la salud LGBTQI+ para FPATT, y referente en Trinidad y Tobago por de los derechos humanos. Ha sido durante mucho tiempo una defensora de los derechos de las personas LGBTQI+, y una pionera en garantizar el acceso a los servicios de salud, al tiempo que luchaba contra el estigma y la discriminación en la comunidad. Honramos su dedicación a la igualdad en todo el Caribe y su apasionada defensa de los derechos de las personas trans. La lucha continúa en su memoria.

| 17 May 2025
Ensuring care for Trinidad and Tobago's LGBTI+ community
Public perceptions, a lack of education, and government policies contribute to the barriers and challenges to achieving equality for all. In a country as diverse as Trinidad and Tobago, this is especially acute for certain key populations, including the LGBTI+ community. For Brandy Rodriguez, Healthcare Navigator at the Family Planning Association of Trinidad and Tobago (FPATT), the struggle is both real and personal. In 1999, Brandy began her transition to womanhood and since 2006 has been working with FPATT in their HIV programme for the LGBTI+ community. “Back in 2004, very little was said about HIV infection, transmission and prevention. In fact, if there was any information, it was misconstrued and meant to stigmatize the LGBTI+ community. I was fairly new to the transgender community, so I made it a mission to research and find out the truths behind HIV and how I could protect myself. I then felt like I had to share what I found with others who were searching as well,” she said. Overcoming prejudice and stigma That’s when FPATT asked Brandy to join their team in educating the LGBTI+ community on the types of healthcare available. Stigma surrounding the community forced many to stay hidden and avoid seeking care. Even if a member of the LGBTI+ community wanted to test for their HIV status, they would never dare to go into a public health centre, because of the fear of being judged by the healthcare professionals. “It’s a simple case of this. When a transgender or non-binary person walks into a health centre or hospital, and the triage nurse has to fill in a form that asks for gender, the only two options there are male and female. So usually, the non-binary person knows that if they want to access that healthcare, free of judgement, they would have to dress as the gender that would bring less attention. At the end of the day, the healthcare provider does not receive accurate information about the client, and the client doesn’t receive the scope of assessment and treatment that may be necessary. So part of what I do, is to simply accompany the client to the appointment so that it’s a less stressful experience and they don’t feel like they are alone,” says Brandy. The importance of access to HIV treatment and care Apart from a great lack of healthcare professionals that are willing to treat the LGBTI+ community non-judgementally, the community also lacks social support. Most of the members of the community face barriers to housing and employment, which often means earning a livelihood through sex work. Over 95% of skilled and employable persons within the LGBTI+ community have turned to sex work because they are constantly denied employment within other industries. “When I began my transition, I was fortunate to have the support of my family; they understood my heart and my need to be my authentic self. Not everyone has that support and so some either migrate or are left homeless because of the fact. Having to work within the sex industry means that they are now at greater risk for HIV or other STIs. My job as an Educator and Navigator is to promote condom use and ensure that they make use of FPATT’s regular HIV testing. If they do test positive, we then have that conversation about U=U, which means that if they [their HIV viral load] are undetectable, they will be untransferable, and then get them to that place of undetectability.” Brandy explains that being undetectable means that the client’s viral load is suppressed, and they are living healthy lives. The team works hard to ensure clients living with HIV enrol in the FPATT Programme, which supports the importance of adhering to consistent treatment, healthy eating, and rest. As well as testing, the Programme offers sexual and reproductive health education on prevention against STIs and both group and one-to-one sessions to anyone who needs it. Advocating for support FPATT has, for many years, advocated for the sexual and reproductive rights of the LGBTI+ community, ensuring that it remains a safe place for HIV testing and counselling. It holds a vision of a world where gender or sexuality are no longer a source of inequality or stigma. FPATT is poised to become a full-service HIV treatment site, offering antiretroviral treatment as well as psychosocial services for persons affected by HIV. FPATT’s goal is to stop discrimination and stigma against persons living with HIV and ultimately end the spread of HIV within Trinidad and Tobago by 2030. October 28, 2021 - We celebrate our much beloved colleague Brandy, LGBTQI+ Healthcare Navigator for FPATT and Trinidadian champion of human rights. She has long been a defender of the rights of LGBTQI+ people, and a pioneer in ensuring access to services while fighting stigma and discrimination in the community. We honor her dedication to equality across the Caribbean, her passionate advocacy for Trans rights. The fight continues in her powerful memory. Conmemoramos a nuestra querida colega Brandy, defensora por la salud LGBTQI+ para FPATT, y referente en Trinidad y Tobago por de los derechos humanos. Ha sido durante mucho tiempo una defensora de los derechos de las personas LGBTQI+, y una pionera en garantizar el acceso a los servicios de salud, al tiempo que luchaba contra el estigma y la discriminación en la comunidad. Honramos su dedicación a la igualdad en todo el Caribe y su apasionada defensa de los derechos de las personas trans. La lucha continúa en su memoria.

| 23 September 2020
In pictures: Innovating during COVID-19
Women around the world have faced multiple barriers to accessing safe abortion care during the COVID-19 pandemic including the de-prioritization of sexual and reproductive healthcare, overwhelmed health systems and restrictions on movement. The COVID-19 crisis has sparked innovation among IPPF Member Associations who responded swiftly by developing new approaches to reach women with safe abortion care including telemedicine and home-based provision of medical abortion. Strong evidence generated from this work supports the continuation and strengthening of these approaches beyond the end of the pandemic. Cameroon Cameroon National Planning Association for Family Welfare (CAMNAFAW) To ensure that quality abortion care can be provided to women during travel restrictions, CAMNAFAW’s service providers travel to partner clinics in underserved areas and to clients’ homes to provide medical and surgical abortion care. This model of taking safe abortion care closer to women will continue even with easing of travel restrictions, as this has been found to be an effective and acceptable approach to increasing access.Photo: IPPF/Xaume Olleros/Cameroon Share on Twitter Share on Facebook Share via WhatsApp Share via Email Guinea Association Guinéenne pour le Bien-Etre Familial (AGBEF) Building on lessons learned during the Ebola crisis in Guinea, AGBEF quickly took measures to prevent infection in its clinics to continue providing sexual and reproductive healthcare, including surgical and medical abortion, in a safe environment. AGBEF donated protective materials to communities, including hand-washing stations, face masks and antibacterial gel, alongside messaging on infection prevention. This community visibility reassures clients they can safely attend AGBEF clinics for abortion and contraceptive care.Photo: AGBEF/Guinea Share on Twitter Share on Facebook Share via WhatsApp Share via Email India Family Planning Association of India (FPA India) FPA India and partners advocated to have sexual and reproductive healthcare, including abortion, recognized as essential by the government, which meant FPA India could continue healthcare delivery during the national lockdown. To reduce in-person clinic visits, FPA India established teleconsultation and counselling for abortion care, and is continuing to provide in-clinic care for both medical and surgical abortion. Photo: IPPF/Alison Joyce/India Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nepal Family Planning Association of Nepal (FPAN) FPAN and partners advocated for interim approval of home provision of medical abortion and telemedicine for abortion counselling during COVID-19. FPAN is now implementing these approaches, ensuring continued access to abortion care in Nepal, where many people live in remote locations with limited mobility, which has been further restricted by COVID-19 lockdowns. Photo: FPAN/Nepal Share on Twitter Share on Facebook Share via WhatsApp Share via Email Pakistan Rahnuma – Family Planning Association of Pakistan (Rahnuma-FPAP) Rahnuma-FPAP and partners successfully advocated for the government to class sexual and reproductive healthcare as ‘essential’, which enabled the team to continue providing post-abortion care during the pandemic. Rahnuma-FPAP expanded its telemedicine and home-based provision for menstrual regulation counselling and post-abortion care. These new approaches have ensured continued access to services for clients unable to reach clinics.Photo: Rahnuma-FPAP/Pakistan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Palestine Palestinian Family Planning and Protection Association (PFPPA) In response to the government-mandated closure of its clinics, PFPPA quickly established a toll-free call centre which provides consultations, counselling, referrals and follow-up, including consultation for abortion care through a harm reduction approach, ensuring that women are provided with accurate information. Due to its success, PFPPA is exploring options for continuing this healthcare delivery model beyond the pandemic, with the aim of keeping it free of charge for users.Photo: SAAF/Samar Hazboun/Palestine Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sudan Sudan Family Planning Association (SFPA) Following a nation-wide shutdown in April, SFPA established a call centre to increase access to healthcare, including abortion and contraceptive counselling and referrals. An unexpected outcome of the new call centre is that it has reached an increased number of young women who regularly call to discuss their reproductive health and rights. SFPA is working towards institutionalizing this model for continuation beyond the pandemic.Photo: SFPA/Sudan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Togo Association Togolaise pour le Bien-Etre Familial (ATBEF) ATBEF adapted its mobile application ‘Infos Ado Jeunes’, adding a toll-free teleconsultation service for young clients to use to access abortion consultations and pre- and post-abortion counselling. This app has given young clients ongoing access to care when they face challenges travelling to clinics. It has also eased overall client flow in clinics at a time when social distancing is being implemented.Photo: ATBEF/Togo Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 17 May 2025
In pictures: Innovating during COVID-19
Women around the world have faced multiple barriers to accessing safe abortion care during the COVID-19 pandemic including the de-prioritization of sexual and reproductive healthcare, overwhelmed health systems and restrictions on movement. The COVID-19 crisis has sparked innovation among IPPF Member Associations who responded swiftly by developing new approaches to reach women with safe abortion care including telemedicine and home-based provision of medical abortion. Strong evidence generated from this work supports the continuation and strengthening of these approaches beyond the end of the pandemic. Cameroon Cameroon National Planning Association for Family Welfare (CAMNAFAW) To ensure that quality abortion care can be provided to women during travel restrictions, CAMNAFAW’s service providers travel to partner clinics in underserved areas and to clients’ homes to provide medical and surgical abortion care. This model of taking safe abortion care closer to women will continue even with easing of travel restrictions, as this has been found to be an effective and acceptable approach to increasing access.Photo: IPPF/Xaume Olleros/Cameroon Share on Twitter Share on Facebook Share via WhatsApp Share via Email Guinea Association Guinéenne pour le Bien-Etre Familial (AGBEF) Building on lessons learned during the Ebola crisis in Guinea, AGBEF quickly took measures to prevent infection in its clinics to continue providing sexual and reproductive healthcare, including surgical and medical abortion, in a safe environment. AGBEF donated protective materials to communities, including hand-washing stations, face masks and antibacterial gel, alongside messaging on infection prevention. This community visibility reassures clients they can safely attend AGBEF clinics for abortion and contraceptive care.Photo: AGBEF/Guinea Share on Twitter Share on Facebook Share via WhatsApp Share via Email India Family Planning Association of India (FPA India) FPA India and partners advocated to have sexual and reproductive healthcare, including abortion, recognized as essential by the government, which meant FPA India could continue healthcare delivery during the national lockdown. To reduce in-person clinic visits, FPA India established teleconsultation and counselling for abortion care, and is continuing to provide in-clinic care for both medical and surgical abortion. Photo: IPPF/Alison Joyce/India Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nepal Family Planning Association of Nepal (FPAN) FPAN and partners advocated for interim approval of home provision of medical abortion and telemedicine for abortion counselling during COVID-19. FPAN is now implementing these approaches, ensuring continued access to abortion care in Nepal, where many people live in remote locations with limited mobility, which has been further restricted by COVID-19 lockdowns. Photo: FPAN/Nepal Share on Twitter Share on Facebook Share via WhatsApp Share via Email Pakistan Rahnuma – Family Planning Association of Pakistan (Rahnuma-FPAP) Rahnuma-FPAP and partners successfully advocated for the government to class sexual and reproductive healthcare as ‘essential’, which enabled the team to continue providing post-abortion care during the pandemic. Rahnuma-FPAP expanded its telemedicine and home-based provision for menstrual regulation counselling and post-abortion care. These new approaches have ensured continued access to services for clients unable to reach clinics.Photo: Rahnuma-FPAP/Pakistan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Palestine Palestinian Family Planning and Protection Association (PFPPA) In response to the government-mandated closure of its clinics, PFPPA quickly established a toll-free call centre which provides consultations, counselling, referrals and follow-up, including consultation for abortion care through a harm reduction approach, ensuring that women are provided with accurate information. Due to its success, PFPPA is exploring options for continuing this healthcare delivery model beyond the pandemic, with the aim of keeping it free of charge for users.Photo: SAAF/Samar Hazboun/Palestine Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sudan Sudan Family Planning Association (SFPA) Following a nation-wide shutdown in April, SFPA established a call centre to increase access to healthcare, including abortion and contraceptive counselling and referrals. An unexpected outcome of the new call centre is that it has reached an increased number of young women who regularly call to discuss their reproductive health and rights. SFPA is working towards institutionalizing this model for continuation beyond the pandemic.Photo: SFPA/Sudan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Togo Association Togolaise pour le Bien-Etre Familial (ATBEF) ATBEF adapted its mobile application ‘Infos Ado Jeunes’, adding a toll-free teleconsultation service for young clients to use to access abortion consultations and pre- and post-abortion counselling. This app has given young clients ongoing access to care when they face challenges travelling to clinics. It has also eased overall client flow in clinics at a time when social distancing is being implemented.Photo: ATBEF/Togo Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 08 July 2019
"I help to raise awareness of why we have to protect ourselves"
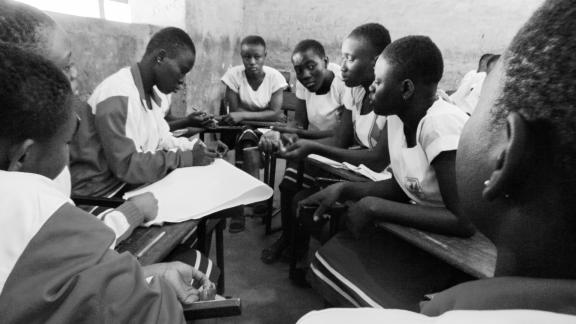
“The first time I met Chariette [a peer educator for the Cameroon National Planning Association for Family Welfare] was at Sunday football, around four years ago. She was invited by the organizer to come and talk to us when the match was over. We were all men but she wasn’t intimidated and she handled the stupid jokes well. We stayed in touch and then one day I realized I had an STI. It’s a little taboo and I didn’t want to talk about it. I bought some drugs at the local market but they didn’t have any effect. I called Chariette and we discussed what had happened. She told me to come to the CAMNAFAW clinic and I did, where I spoke about my problem and they gave me proper drugs to get rid of it. That day, I decided to become a peer educator myself. There are a lot of guys who are suffering but too scared to speak out. Above all, men are scared of talking about STIs. I now work in schools and youth groups, especially sports teams. They will insist they don’t have anything wrong but every Sunday since then I have gone round the teams and chatted with them. I speak about pregnancy as well. It’s the guys who push women to have sex without a condom and also to have an abortion afterwards. I help to raise awareness of why we have to protect ourselves. It’s hard to recruit people to become peer educators because we are volunteers. It’s not easy to persuade people to change their ways. The view from a lot of churches is very strict and centers on abstinence. The young men want to be macho.” Hervé Tchuigwa Djiya is a peer educator for the Cameroon National Planning Association for Family Welfare (CAMNAFAW)

| 17 May 2025
"I help to raise awareness of why we have to protect ourselves"
“The first time I met Chariette [a peer educator for the Cameroon National Planning Association for Family Welfare] was at Sunday football, around four years ago. She was invited by the organizer to come and talk to us when the match was over. We were all men but she wasn’t intimidated and she handled the stupid jokes well. We stayed in touch and then one day I realized I had an STI. It’s a little taboo and I didn’t want to talk about it. I bought some drugs at the local market but they didn’t have any effect. I called Chariette and we discussed what had happened. She told me to come to the CAMNAFAW clinic and I did, where I spoke about my problem and they gave me proper drugs to get rid of it. That day, I decided to become a peer educator myself. There are a lot of guys who are suffering but too scared to speak out. Above all, men are scared of talking about STIs. I now work in schools and youth groups, especially sports teams. They will insist they don’t have anything wrong but every Sunday since then I have gone round the teams and chatted with them. I speak about pregnancy as well. It’s the guys who push women to have sex without a condom and also to have an abortion afterwards. I help to raise awareness of why we have to protect ourselves. It’s hard to recruit people to become peer educators because we are volunteers. It’s not easy to persuade people to change their ways. The view from a lot of churches is very strict and centers on abstinence. The young men want to be macho.” Hervé Tchuigwa Djiya is a peer educator for the Cameroon National Planning Association for Family Welfare (CAMNAFAW)

| 08 July 2019
"I have brothers and I have helped them to change too. I’ve helped them to adopt a healthier sex life"
“Chariette was my neighbor. We lived next door to each other. She often organized group information sessions in the neighbourhood to talk about sexually transmitted infections (STIs) and early pregnancy, and unintended pregnancies as well. When I started attending her sessions I was in a bit of unstable relationship. My life was chaotic. My boyfriend didn’t like using protection and we told each other that as we loved each other we weren’t taking any risks. Once I caught something and I was itching a lot. My boyfriend told me that I must have caught it in a public toilet. I trusted him and I didn’t realize I could catch something. When I started listening to Chariette it opened my eyes and I realized I was running big risks. As we aren’t married and we are still studying, we shouldn’t have an unintended pregnancy. What would we do? She told me about sexually transmitted infections as well. I tried to talk to my boyfriend about it but he didn’t want to hear about it, especially about using condoms. I asked for a private session with Chariette for him, and she spoke to us both and he finally understood. Today we have a much more stable sex life and we aren’t running those risks anymore. He learned how to use a condom. After attending her sessions, I was able to save a friend with Chariette’s help. This friend tried to perform an abortion herself and she was bleeding everywhere. I remembered that Chariette told me about the Cameroon National Planning Association for Family Welfare clinic, so I called her and asked how she could be admitted. She was able to receive post-abortion care but if I hadn’t known Chariette I don’t know what would have happened. I have brothers and I have helped them to change too. I’ve helped them to adopt a healthier sex life. There is HIV around and it’s scary.” Gertrude Zouakeu Noutcha, 29, is a student and peer educator for the Cameroon National Planning Association for Family Welfare (CAMNAFAW)

| 17 May 2025
"I have brothers and I have helped them to change too. I’ve helped them to adopt a healthier sex life"
“Chariette was my neighbor. We lived next door to each other. She often organized group information sessions in the neighbourhood to talk about sexually transmitted infections (STIs) and early pregnancy, and unintended pregnancies as well. When I started attending her sessions I was in a bit of unstable relationship. My life was chaotic. My boyfriend didn’t like using protection and we told each other that as we loved each other we weren’t taking any risks. Once I caught something and I was itching a lot. My boyfriend told me that I must have caught it in a public toilet. I trusted him and I didn’t realize I could catch something. When I started listening to Chariette it opened my eyes and I realized I was running big risks. As we aren’t married and we are still studying, we shouldn’t have an unintended pregnancy. What would we do? She told me about sexually transmitted infections as well. I tried to talk to my boyfriend about it but he didn’t want to hear about it, especially about using condoms. I asked for a private session with Chariette for him, and she spoke to us both and he finally understood. Today we have a much more stable sex life and we aren’t running those risks anymore. He learned how to use a condom. After attending her sessions, I was able to save a friend with Chariette’s help. This friend tried to perform an abortion herself and she was bleeding everywhere. I remembered that Chariette told me about the Cameroon National Planning Association for Family Welfare clinic, so I called her and asked how she could be admitted. She was able to receive post-abortion care but if I hadn’t known Chariette I don’t know what would have happened. I have brothers and I have helped them to change too. I’ve helped them to adopt a healthier sex life. There is HIV around and it’s scary.” Gertrude Zouakeu Noutcha, 29, is a student and peer educator for the Cameroon National Planning Association for Family Welfare (CAMNAFAW)

| 24 June 2021
Changing mindsets through medicine and motivation
“You work with people who have HIV? Why?” That was the question Dr. Gregory Boyce was asked by the young intern that stood before him. He had come to the hospital ward to visit a client who was known to be living with HIV. He approached the intern at the desk and gave his name and designation. The intern looked at him, confused and somewhat amused and asked the question that he has neither forgotten, nor understood to this day. However, this young intern’s question comes from a mindset that Dr. Boyce is working fervently to change. As Deputy Director of the Medical Research Foundation of Trinidad and Tobago (MRF), Dr. Boyce provides clinical and administrative support to a team of doctors and nurses providing care to their clients who are living with HIV. Due to MRF’s long-standing work in HIV research and healthcare, the Family Planning Association of Trinidad and Tobago (FPATT), has referred many clients to Dr. Boyce and his team, and especially clients from the LGBTI+ community. Providing specialist care and support “Persons coming to us from key populations, have very layered needs. They are facing unique challenges in addition to living with the virus. There is still that myth that being HIV positive means that you will positively die. Added to that, there’s the discrimination that the community faces in every aspect of their lives on a daily basis. As a staff, we’ve had to seek special training to guide the way we interact with these clients so that we can meet all their needs appropriately and sensitively,” explains Dr. Boyce. “Apart from medical interventions which are needed to ensure that our clients continue to live healthy lives, we focus heavily on their psychosocial needs. It’s easy to think that because a client is physically healthy that they are also emotionally healthy. We have clients that won’t leave abusive relationships because they think no one else would accept them. We have other clients that are dealing with long-term medication fatigue because they have been taking pills for over 10 years. With that sometimes comes depression and other drug addictions, which is why it’s necessary for us to maintain open and honest relationships to address those accompanying issues.” Making HIV a non-issue Dr Boyce has been committed to providing treatment and care to clients living with HIV for over 20 years. He had worked at the Port of Spain General Hospital after graduating, during which time, medicine for persons living with HIV was expensive and out of reach for many. A few years later, through government programmes, medicine became more affordable, and treatment centres were opening up across the island. However, Dr. Boyce realized that the mortality rate had not changed by much. He wondered why people were still dying from a virus when medicine was easily accessible. “That first conversation – giving a client the news that they’ve tested positive – is very important. We get to show them that HIV is not an impediment. Most times, with the wrong information, they start to draw up a list of things that they can no longer do, like go after a promotion or start a family. Then they go through life shrunken and unrecognizable, not the person they once were. So to answer that intern’s question about why I work with persons living with HIV: I want to make HIV a non-issue,” he states. Dr. Boyce hopes to see HIV disclosure become as acceptable as other chronic illnesses such as cancer or diabetes, where an entire family would work towards caring for the affected person, instead of alienating them. He also hopes to see more inclusion and tolerance towards persons living with HIV, especially those within the LGBTI+ community. “Until a gay or transgender person can walk the streets freely and not be jeered at by passers-by, we still have a long way to go. Until they can access treatment at any public facility without fear or judgment, we have a lot of work to do. It would take a lot of education to change the stigma and discrimination but there is absolutely no reason why another person’s life should be miserable because their expression is different to ours.” He commends the work of FPATT in upholding the sexual and reproductive health and rights of the LGBTI+ community, through ensuring that they have a safe and non-judgmental environment for treatment and care. He says that the Medical Research Foundation values the great relationship that the two organizations have had for years, even as FPATT works towards becoming its own full-service antiretroviral treatment site for persons living with HIV.

| 17 May 2025
Changing mindsets through medicine and motivation
“You work with people who have HIV? Why?” That was the question Dr. Gregory Boyce was asked by the young intern that stood before him. He had come to the hospital ward to visit a client who was known to be living with HIV. He approached the intern at the desk and gave his name and designation. The intern looked at him, confused and somewhat amused and asked the question that he has neither forgotten, nor understood to this day. However, this young intern’s question comes from a mindset that Dr. Boyce is working fervently to change. As Deputy Director of the Medical Research Foundation of Trinidad and Tobago (MRF), Dr. Boyce provides clinical and administrative support to a team of doctors and nurses providing care to their clients who are living with HIV. Due to MRF’s long-standing work in HIV research and healthcare, the Family Planning Association of Trinidad and Tobago (FPATT), has referred many clients to Dr. Boyce and his team, and especially clients from the LGBTI+ community. Providing specialist care and support “Persons coming to us from key populations, have very layered needs. They are facing unique challenges in addition to living with the virus. There is still that myth that being HIV positive means that you will positively die. Added to that, there’s the discrimination that the community faces in every aspect of their lives on a daily basis. As a staff, we’ve had to seek special training to guide the way we interact with these clients so that we can meet all their needs appropriately and sensitively,” explains Dr. Boyce. “Apart from medical interventions which are needed to ensure that our clients continue to live healthy lives, we focus heavily on their psychosocial needs. It’s easy to think that because a client is physically healthy that they are also emotionally healthy. We have clients that won’t leave abusive relationships because they think no one else would accept them. We have other clients that are dealing with long-term medication fatigue because they have been taking pills for over 10 years. With that sometimes comes depression and other drug addictions, which is why it’s necessary for us to maintain open and honest relationships to address those accompanying issues.” Making HIV a non-issue Dr Boyce has been committed to providing treatment and care to clients living with HIV for over 20 years. He had worked at the Port of Spain General Hospital after graduating, during which time, medicine for persons living with HIV was expensive and out of reach for many. A few years later, through government programmes, medicine became more affordable, and treatment centres were opening up across the island. However, Dr. Boyce realized that the mortality rate had not changed by much. He wondered why people were still dying from a virus when medicine was easily accessible. “That first conversation – giving a client the news that they’ve tested positive – is very important. We get to show them that HIV is not an impediment. Most times, with the wrong information, they start to draw up a list of things that they can no longer do, like go after a promotion or start a family. Then they go through life shrunken and unrecognizable, not the person they once were. So to answer that intern’s question about why I work with persons living with HIV: I want to make HIV a non-issue,” he states. Dr. Boyce hopes to see HIV disclosure become as acceptable as other chronic illnesses such as cancer or diabetes, where an entire family would work towards caring for the affected person, instead of alienating them. He also hopes to see more inclusion and tolerance towards persons living with HIV, especially those within the LGBTI+ community. “Until a gay or transgender person can walk the streets freely and not be jeered at by passers-by, we still have a long way to go. Until they can access treatment at any public facility without fear or judgment, we have a lot of work to do. It would take a lot of education to change the stigma and discrimination but there is absolutely no reason why another person’s life should be miserable because their expression is different to ours.” He commends the work of FPATT in upholding the sexual and reproductive health and rights of the LGBTI+ community, through ensuring that they have a safe and non-judgmental environment for treatment and care. He says that the Medical Research Foundation values the great relationship that the two organizations have had for years, even as FPATT works towards becoming its own full-service antiretroviral treatment site for persons living with HIV.

| 24 June 2021
Ensuring care for Trinidad and Tobago's LGBTI+ community
Public perceptions, a lack of education, and government policies contribute to the barriers and challenges to achieving equality for all. In a country as diverse as Trinidad and Tobago, this is especially acute for certain key populations, including the LGBTI+ community. For Brandy Rodriguez, Healthcare Navigator at the Family Planning Association of Trinidad and Tobago (FPATT), the struggle is both real and personal. In 1999, Brandy began her transition to womanhood and since 2006 has been working with FPATT in their HIV programme for the LGBTI+ community. “Back in 2004, very little was said about HIV infection, transmission and prevention. In fact, if there was any information, it was misconstrued and meant to stigmatize the LGBTI+ community. I was fairly new to the transgender community, so I made it a mission to research and find out the truths behind HIV and how I could protect myself. I then felt like I had to share what I found with others who were searching as well,” she said. Overcoming prejudice and stigma That’s when FPATT asked Brandy to join their team in educating the LGBTI+ community on the types of healthcare available. Stigma surrounding the community forced many to stay hidden and avoid seeking care. Even if a member of the LGBTI+ community wanted to test for their HIV status, they would never dare to go into a public health centre, because of the fear of being judged by the healthcare professionals. “It’s a simple case of this. When a transgender or non-binary person walks into a health centre or hospital, and the triage nurse has to fill in a form that asks for gender, the only two options there are male and female. So usually, the non-binary person knows that if they want to access that healthcare, free of judgement, they would have to dress as the gender that would bring less attention. At the end of the day, the healthcare provider does not receive accurate information about the client, and the client doesn’t receive the scope of assessment and treatment that may be necessary. So part of what I do, is to simply accompany the client to the appointment so that it’s a less stressful experience and they don’t feel like they are alone,” says Brandy. The importance of access to HIV treatment and care Apart from a great lack of healthcare professionals that are willing to treat the LGBTI+ community non-judgementally, the community also lacks social support. Most of the members of the community face barriers to housing and employment, which often means earning a livelihood through sex work. Over 95% of skilled and employable persons within the LGBTI+ community have turned to sex work because they are constantly denied employment within other industries. “When I began my transition, I was fortunate to have the support of my family; they understood my heart and my need to be my authentic self. Not everyone has that support and so some either migrate or are left homeless because of the fact. Having to work within the sex industry means that they are now at greater risk for HIV or other STIs. My job as an Educator and Navigator is to promote condom use and ensure that they make use of FPATT’s regular HIV testing. If they do test positive, we then have that conversation about U=U, which means that if they [their HIV viral load] are undetectable, they will be untransferable, and then get them to that place of undetectability.” Brandy explains that being undetectable means that the client’s viral load is suppressed, and they are living healthy lives. The team works hard to ensure clients living with HIV enrol in the FPATT Programme, which supports the importance of adhering to consistent treatment, healthy eating, and rest. As well as testing, the Programme offers sexual and reproductive health education on prevention against STIs and both group and one-to-one sessions to anyone who needs it. Advocating for support FPATT has, for many years, advocated for the sexual and reproductive rights of the LGBTI+ community, ensuring that it remains a safe place for HIV testing and counselling. It holds a vision of a world where gender or sexuality are no longer a source of inequality or stigma. FPATT is poised to become a full-service HIV treatment site, offering antiretroviral treatment as well as psychosocial services for persons affected by HIV. FPATT’s goal is to stop discrimination and stigma against persons living with HIV and ultimately end the spread of HIV within Trinidad and Tobago by 2030. October 28, 2021 - We celebrate our much beloved colleague Brandy, LGBTQI+ Healthcare Navigator for FPATT and Trinidadian champion of human rights. She has long been a defender of the rights of LGBTQI+ people, and a pioneer in ensuring access to services while fighting stigma and discrimination in the community. We honor her dedication to equality across the Caribbean, her passionate advocacy for Trans rights. The fight continues in her powerful memory. Conmemoramos a nuestra querida colega Brandy, defensora por la salud LGBTQI+ para FPATT, y referente en Trinidad y Tobago por de los derechos humanos. Ha sido durante mucho tiempo una defensora de los derechos de las personas LGBTQI+, y una pionera en garantizar el acceso a los servicios de salud, al tiempo que luchaba contra el estigma y la discriminación en la comunidad. Honramos su dedicación a la igualdad en todo el Caribe y su apasionada defensa de los derechos de las personas trans. La lucha continúa en su memoria.

| 17 May 2025
Ensuring care for Trinidad and Tobago's LGBTI+ community
Public perceptions, a lack of education, and government policies contribute to the barriers and challenges to achieving equality for all. In a country as diverse as Trinidad and Tobago, this is especially acute for certain key populations, including the LGBTI+ community. For Brandy Rodriguez, Healthcare Navigator at the Family Planning Association of Trinidad and Tobago (FPATT), the struggle is both real and personal. In 1999, Brandy began her transition to womanhood and since 2006 has been working with FPATT in their HIV programme for the LGBTI+ community. “Back in 2004, very little was said about HIV infection, transmission and prevention. In fact, if there was any information, it was misconstrued and meant to stigmatize the LGBTI+ community. I was fairly new to the transgender community, so I made it a mission to research and find out the truths behind HIV and how I could protect myself. I then felt like I had to share what I found with others who were searching as well,” she said. Overcoming prejudice and stigma That’s when FPATT asked Brandy to join their team in educating the LGBTI+ community on the types of healthcare available. Stigma surrounding the community forced many to stay hidden and avoid seeking care. Even if a member of the LGBTI+ community wanted to test for their HIV status, they would never dare to go into a public health centre, because of the fear of being judged by the healthcare professionals. “It’s a simple case of this. When a transgender or non-binary person walks into a health centre or hospital, and the triage nurse has to fill in a form that asks for gender, the only two options there are male and female. So usually, the non-binary person knows that if they want to access that healthcare, free of judgement, they would have to dress as the gender that would bring less attention. At the end of the day, the healthcare provider does not receive accurate information about the client, and the client doesn’t receive the scope of assessment and treatment that may be necessary. So part of what I do, is to simply accompany the client to the appointment so that it’s a less stressful experience and they don’t feel like they are alone,” says Brandy. The importance of access to HIV treatment and care Apart from a great lack of healthcare professionals that are willing to treat the LGBTI+ community non-judgementally, the community also lacks social support. Most of the members of the community face barriers to housing and employment, which often means earning a livelihood through sex work. Over 95% of skilled and employable persons within the LGBTI+ community have turned to sex work because they are constantly denied employment within other industries. “When I began my transition, I was fortunate to have the support of my family; they understood my heart and my need to be my authentic self. Not everyone has that support and so some either migrate or are left homeless because of the fact. Having to work within the sex industry means that they are now at greater risk for HIV or other STIs. My job as an Educator and Navigator is to promote condom use and ensure that they make use of FPATT’s regular HIV testing. If they do test positive, we then have that conversation about U=U, which means that if they [their HIV viral load] are undetectable, they will be untransferable, and then get them to that place of undetectability.” Brandy explains that being undetectable means that the client’s viral load is suppressed, and they are living healthy lives. The team works hard to ensure clients living with HIV enrol in the FPATT Programme, which supports the importance of adhering to consistent treatment, healthy eating, and rest. As well as testing, the Programme offers sexual and reproductive health education on prevention against STIs and both group and one-to-one sessions to anyone who needs it. Advocating for support FPATT has, for many years, advocated for the sexual and reproductive rights of the LGBTI+ community, ensuring that it remains a safe place for HIV testing and counselling. It holds a vision of a world where gender or sexuality are no longer a source of inequality or stigma. FPATT is poised to become a full-service HIV treatment site, offering antiretroviral treatment as well as psychosocial services for persons affected by HIV. FPATT’s goal is to stop discrimination and stigma against persons living with HIV and ultimately end the spread of HIV within Trinidad and Tobago by 2030. October 28, 2021 - We celebrate our much beloved colleague Brandy, LGBTQI+ Healthcare Navigator for FPATT and Trinidadian champion of human rights. She has long been a defender of the rights of LGBTQI+ people, and a pioneer in ensuring access to services while fighting stigma and discrimination in the community. We honor her dedication to equality across the Caribbean, her passionate advocacy for Trans rights. The fight continues in her powerful memory. Conmemoramos a nuestra querida colega Brandy, defensora por la salud LGBTQI+ para FPATT, y referente en Trinidad y Tobago por de los derechos humanos. Ha sido durante mucho tiempo una defensora de los derechos de las personas LGBTQI+, y una pionera en garantizar el acceso a los servicios de salud, al tiempo que luchaba contra el estigma y la discriminación en la comunidad. Honramos su dedicación a la igualdad en todo el Caribe y su apasionada defensa de los derechos de las personas trans. La lucha continúa en su memoria.

| 23 September 2020
In pictures: Innovating during COVID-19
Women around the world have faced multiple barriers to accessing safe abortion care during the COVID-19 pandemic including the de-prioritization of sexual and reproductive healthcare, overwhelmed health systems and restrictions on movement. The COVID-19 crisis has sparked innovation among IPPF Member Associations who responded swiftly by developing new approaches to reach women with safe abortion care including telemedicine and home-based provision of medical abortion. Strong evidence generated from this work supports the continuation and strengthening of these approaches beyond the end of the pandemic. Cameroon Cameroon National Planning Association for Family Welfare (CAMNAFAW) To ensure that quality abortion care can be provided to women during travel restrictions, CAMNAFAW’s service providers travel to partner clinics in underserved areas and to clients’ homes to provide medical and surgical abortion care. This model of taking safe abortion care closer to women will continue even with easing of travel restrictions, as this has been found to be an effective and acceptable approach to increasing access.Photo: IPPF/Xaume Olleros/Cameroon Share on Twitter Share on Facebook Share via WhatsApp Share via Email Guinea Association Guinéenne pour le Bien-Etre Familial (AGBEF) Building on lessons learned during the Ebola crisis in Guinea, AGBEF quickly took measures to prevent infection in its clinics to continue providing sexual and reproductive healthcare, including surgical and medical abortion, in a safe environment. AGBEF donated protective materials to communities, including hand-washing stations, face masks and antibacterial gel, alongside messaging on infection prevention. This community visibility reassures clients they can safely attend AGBEF clinics for abortion and contraceptive care.Photo: AGBEF/Guinea Share on Twitter Share on Facebook Share via WhatsApp Share via Email India Family Planning Association of India (FPA India) FPA India and partners advocated to have sexual and reproductive healthcare, including abortion, recognized as essential by the government, which meant FPA India could continue healthcare delivery during the national lockdown. To reduce in-person clinic visits, FPA India established teleconsultation and counselling for abortion care, and is continuing to provide in-clinic care for both medical and surgical abortion. Photo: IPPF/Alison Joyce/India Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nepal Family Planning Association of Nepal (FPAN) FPAN and partners advocated for interim approval of home provision of medical abortion and telemedicine for abortion counselling during COVID-19. FPAN is now implementing these approaches, ensuring continued access to abortion care in Nepal, where many people live in remote locations with limited mobility, which has been further restricted by COVID-19 lockdowns. Photo: FPAN/Nepal Share on Twitter Share on Facebook Share via WhatsApp Share via Email Pakistan Rahnuma – Family Planning Association of Pakistan (Rahnuma-FPAP) Rahnuma-FPAP and partners successfully advocated for the government to class sexual and reproductive healthcare as ‘essential’, which enabled the team to continue providing post-abortion care during the pandemic. Rahnuma-FPAP expanded its telemedicine and home-based provision for menstrual regulation counselling and post-abortion care. These new approaches have ensured continued access to services for clients unable to reach clinics.Photo: Rahnuma-FPAP/Pakistan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Palestine Palestinian Family Planning and Protection Association (PFPPA) In response to the government-mandated closure of its clinics, PFPPA quickly established a toll-free call centre which provides consultations, counselling, referrals and follow-up, including consultation for abortion care through a harm reduction approach, ensuring that women are provided with accurate information. Due to its success, PFPPA is exploring options for continuing this healthcare delivery model beyond the pandemic, with the aim of keeping it free of charge for users.Photo: SAAF/Samar Hazboun/Palestine Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sudan Sudan Family Planning Association (SFPA) Following a nation-wide shutdown in April, SFPA established a call centre to increase access to healthcare, including abortion and contraceptive counselling and referrals. An unexpected outcome of the new call centre is that it has reached an increased number of young women who regularly call to discuss their reproductive health and rights. SFPA is working towards institutionalizing this model for continuation beyond the pandemic.Photo: SFPA/Sudan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Togo Association Togolaise pour le Bien-Etre Familial (ATBEF) ATBEF adapted its mobile application ‘Infos Ado Jeunes’, adding a toll-free teleconsultation service for young clients to use to access abortion consultations and pre- and post-abortion counselling. This app has given young clients ongoing access to care when they face challenges travelling to clinics. It has also eased overall client flow in clinics at a time when social distancing is being implemented.Photo: ATBEF/Togo Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 17 May 2025
In pictures: Innovating during COVID-19
Women around the world have faced multiple barriers to accessing safe abortion care during the COVID-19 pandemic including the de-prioritization of sexual and reproductive healthcare, overwhelmed health systems and restrictions on movement. The COVID-19 crisis has sparked innovation among IPPF Member Associations who responded swiftly by developing new approaches to reach women with safe abortion care including telemedicine and home-based provision of medical abortion. Strong evidence generated from this work supports the continuation and strengthening of these approaches beyond the end of the pandemic. Cameroon Cameroon National Planning Association for Family Welfare (CAMNAFAW) To ensure that quality abortion care can be provided to women during travel restrictions, CAMNAFAW’s service providers travel to partner clinics in underserved areas and to clients’ homes to provide medical and surgical abortion care. This model of taking safe abortion care closer to women will continue even with easing of travel restrictions, as this has been found to be an effective and acceptable approach to increasing access.Photo: IPPF/Xaume Olleros/Cameroon Share on Twitter Share on Facebook Share via WhatsApp Share via Email Guinea Association Guinéenne pour le Bien-Etre Familial (AGBEF) Building on lessons learned during the Ebola crisis in Guinea, AGBEF quickly took measures to prevent infection in its clinics to continue providing sexual and reproductive healthcare, including surgical and medical abortion, in a safe environment. AGBEF donated protective materials to communities, including hand-washing stations, face masks and antibacterial gel, alongside messaging on infection prevention. This community visibility reassures clients they can safely attend AGBEF clinics for abortion and contraceptive care.Photo: AGBEF/Guinea Share on Twitter Share on Facebook Share via WhatsApp Share via Email India Family Planning Association of India (FPA India) FPA India and partners advocated to have sexual and reproductive healthcare, including abortion, recognized as essential by the government, which meant FPA India could continue healthcare delivery during the national lockdown. To reduce in-person clinic visits, FPA India established teleconsultation and counselling for abortion care, and is continuing to provide in-clinic care for both medical and surgical abortion. Photo: IPPF/Alison Joyce/India Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nepal Family Planning Association of Nepal (FPAN) FPAN and partners advocated for interim approval of home provision of medical abortion and telemedicine for abortion counselling during COVID-19. FPAN is now implementing these approaches, ensuring continued access to abortion care in Nepal, where many people live in remote locations with limited mobility, which has been further restricted by COVID-19 lockdowns. Photo: FPAN/Nepal Share on Twitter Share on Facebook Share via WhatsApp Share via Email Pakistan Rahnuma – Family Planning Association of Pakistan (Rahnuma-FPAP) Rahnuma-FPAP and partners successfully advocated for the government to class sexual and reproductive healthcare as ‘essential’, which enabled the team to continue providing post-abortion care during the pandemic. Rahnuma-FPAP expanded its telemedicine and home-based provision for menstrual regulation counselling and post-abortion care. These new approaches have ensured continued access to services for clients unable to reach clinics.Photo: Rahnuma-FPAP/Pakistan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Palestine Palestinian Family Planning and Protection Association (PFPPA) In response to the government-mandated closure of its clinics, PFPPA quickly established a toll-free call centre which provides consultations, counselling, referrals and follow-up, including consultation for abortion care through a harm reduction approach, ensuring that women are provided with accurate information. Due to its success, PFPPA is exploring options for continuing this healthcare delivery model beyond the pandemic, with the aim of keeping it free of charge for users.Photo: SAAF/Samar Hazboun/Palestine Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sudan Sudan Family Planning Association (SFPA) Following a nation-wide shutdown in April, SFPA established a call centre to increase access to healthcare, including abortion and contraceptive counselling and referrals. An unexpected outcome of the new call centre is that it has reached an increased number of young women who regularly call to discuss their reproductive health and rights. SFPA is working towards institutionalizing this model for continuation beyond the pandemic.Photo: SFPA/Sudan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Togo Association Togolaise pour le Bien-Etre Familial (ATBEF) ATBEF adapted its mobile application ‘Infos Ado Jeunes’, adding a toll-free teleconsultation service for young clients to use to access abortion consultations and pre- and post-abortion counselling. This app has given young clients ongoing access to care when they face challenges travelling to clinics. It has also eased overall client flow in clinics at a time when social distancing is being implemented.Photo: ATBEF/Togo Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 08 July 2019
"I help to raise awareness of why we have to protect ourselves"
“The first time I met Chariette [a peer educator for the Cameroon National Planning Association for Family Welfare] was at Sunday football, around four years ago. She was invited by the organizer to come and talk to us when the match was over. We were all men but she wasn’t intimidated and she handled the stupid jokes well. We stayed in touch and then one day I realized I had an STI. It’s a little taboo and I didn’t want to talk about it. I bought some drugs at the local market but they didn’t have any effect. I called Chariette and we discussed what had happened. She told me to come to the CAMNAFAW clinic and I did, where I spoke about my problem and they gave me proper drugs to get rid of it. That day, I decided to become a peer educator myself. There are a lot of guys who are suffering but too scared to speak out. Above all, men are scared of talking about STIs. I now work in schools and youth groups, especially sports teams. They will insist they don’t have anything wrong but every Sunday since then I have gone round the teams and chatted with them. I speak about pregnancy as well. It’s the guys who push women to have sex without a condom and also to have an abortion afterwards. I help to raise awareness of why we have to protect ourselves. It’s hard to recruit people to become peer educators because we are volunteers. It’s not easy to persuade people to change their ways. The view from a lot of churches is very strict and centers on abstinence. The young men want to be macho.” Hervé Tchuigwa Djiya is a peer educator for the Cameroon National Planning Association for Family Welfare (CAMNAFAW)

| 17 May 2025
"I help to raise awareness of why we have to protect ourselves"
“The first time I met Chariette [a peer educator for the Cameroon National Planning Association for Family Welfare] was at Sunday football, around four years ago. She was invited by the organizer to come and talk to us when the match was over. We were all men but she wasn’t intimidated and she handled the stupid jokes well. We stayed in touch and then one day I realized I had an STI. It’s a little taboo and I didn’t want to talk about it. I bought some drugs at the local market but they didn’t have any effect. I called Chariette and we discussed what had happened. She told me to come to the CAMNAFAW clinic and I did, where I spoke about my problem and they gave me proper drugs to get rid of it. That day, I decided to become a peer educator myself. There are a lot of guys who are suffering but too scared to speak out. Above all, men are scared of talking about STIs. I now work in schools and youth groups, especially sports teams. They will insist they don’t have anything wrong but every Sunday since then I have gone round the teams and chatted with them. I speak about pregnancy as well. It’s the guys who push women to have sex without a condom and also to have an abortion afterwards. I help to raise awareness of why we have to protect ourselves. It’s hard to recruit people to become peer educators because we are volunteers. It’s not easy to persuade people to change their ways. The view from a lot of churches is very strict and centers on abstinence. The young men want to be macho.” Hervé Tchuigwa Djiya is a peer educator for the Cameroon National Planning Association for Family Welfare (CAMNAFAW)

| 08 July 2019
"I have brothers and I have helped them to change too. I’ve helped them to adopt a healthier sex life"
“Chariette was my neighbor. We lived next door to each other. She often organized group information sessions in the neighbourhood to talk about sexually transmitted infections (STIs) and early pregnancy, and unintended pregnancies as well. When I started attending her sessions I was in a bit of unstable relationship. My life was chaotic. My boyfriend didn’t like using protection and we told each other that as we loved each other we weren’t taking any risks. Once I caught something and I was itching a lot. My boyfriend told me that I must have caught it in a public toilet. I trusted him and I didn’t realize I could catch something. When I started listening to Chariette it opened my eyes and I realized I was running big risks. As we aren’t married and we are still studying, we shouldn’t have an unintended pregnancy. What would we do? She told me about sexually transmitted infections as well. I tried to talk to my boyfriend about it but he didn’t want to hear about it, especially about using condoms. I asked for a private session with Chariette for him, and she spoke to us both and he finally understood. Today we have a much more stable sex life and we aren’t running those risks anymore. He learned how to use a condom. After attending her sessions, I was able to save a friend with Chariette’s help. This friend tried to perform an abortion herself and she was bleeding everywhere. I remembered that Chariette told me about the Cameroon National Planning Association for Family Welfare clinic, so I called her and asked how she could be admitted. She was able to receive post-abortion care but if I hadn’t known Chariette I don’t know what would have happened. I have brothers and I have helped them to change too. I’ve helped them to adopt a healthier sex life. There is HIV around and it’s scary.” Gertrude Zouakeu Noutcha, 29, is a student and peer educator for the Cameroon National Planning Association for Family Welfare (CAMNAFAW)

| 17 May 2025
"I have brothers and I have helped them to change too. I’ve helped them to adopt a healthier sex life"
“Chariette was my neighbor. We lived next door to each other. She often organized group information sessions in the neighbourhood to talk about sexually transmitted infections (STIs) and early pregnancy, and unintended pregnancies as well. When I started attending her sessions I was in a bit of unstable relationship. My life was chaotic. My boyfriend didn’t like using protection and we told each other that as we loved each other we weren’t taking any risks. Once I caught something and I was itching a lot. My boyfriend told me that I must have caught it in a public toilet. I trusted him and I didn’t realize I could catch something. When I started listening to Chariette it opened my eyes and I realized I was running big risks. As we aren’t married and we are still studying, we shouldn’t have an unintended pregnancy. What would we do? She told me about sexually transmitted infections as well. I tried to talk to my boyfriend about it but he didn’t want to hear about it, especially about using condoms. I asked for a private session with Chariette for him, and she spoke to us both and he finally understood. Today we have a much more stable sex life and we aren’t running those risks anymore. He learned how to use a condom. After attending her sessions, I was able to save a friend with Chariette’s help. This friend tried to perform an abortion herself and she was bleeding everywhere. I remembered that Chariette told me about the Cameroon National Planning Association for Family Welfare clinic, so I called her and asked how she could be admitted. She was able to receive post-abortion care but if I hadn’t known Chariette I don’t know what would have happened. I have brothers and I have helped them to change too. I’ve helped them to adopt a healthier sex life. There is HIV around and it’s scary.” Gertrude Zouakeu Noutcha, 29, is a student and peer educator for the Cameroon National Planning Association for Family Welfare (CAMNAFAW)