This page was originally published in 2012 and has since been updated.
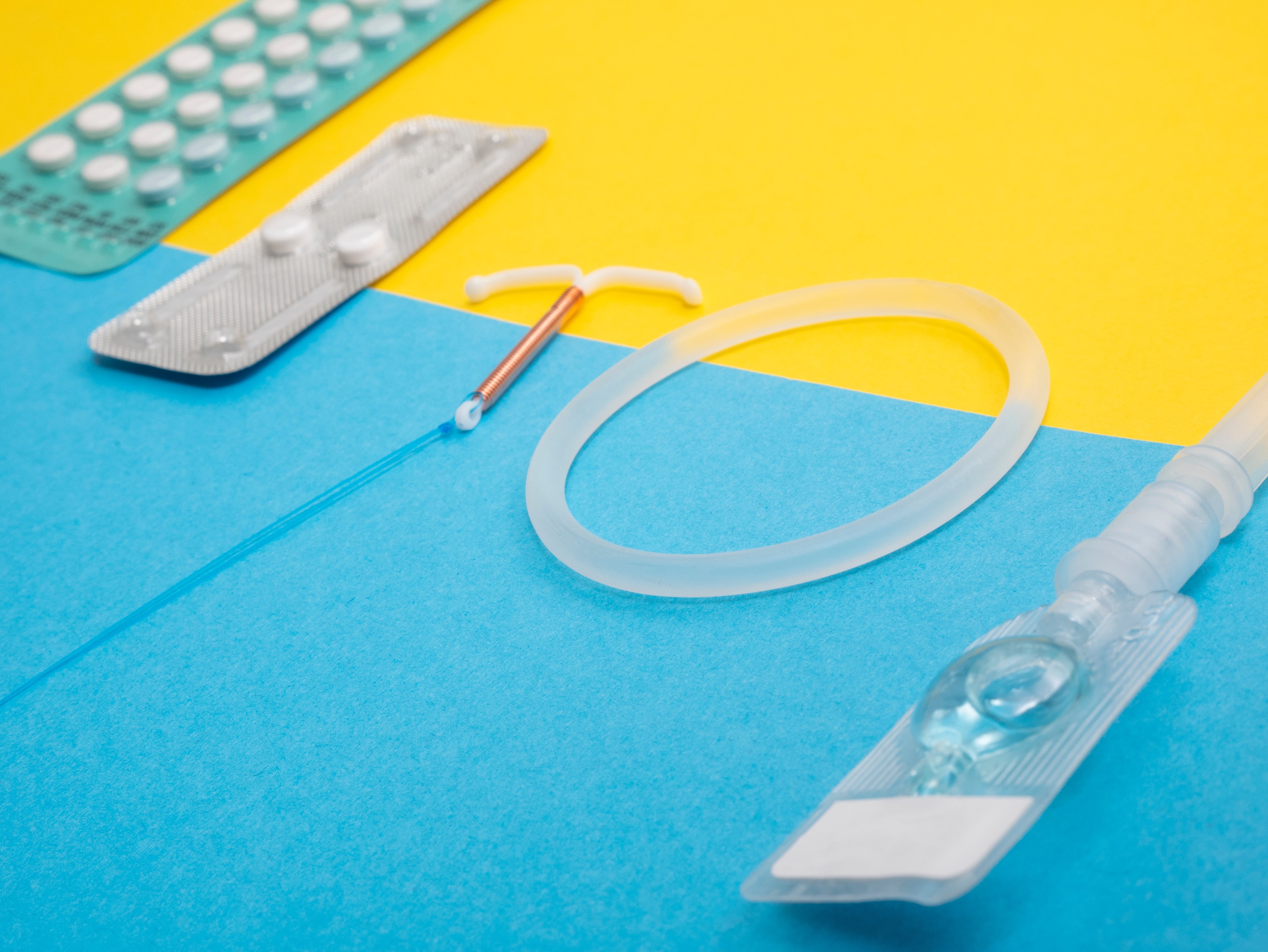
Oral contraceptives (the Pill) are hormonally active pills which are usually taken by women on a daily basis. They contain either two hormones combined (progestogen and estrogen) or a single hormone (progestogen).
Combined oral contraceptives suppress ovulation. Progestogen-only contraceptives also suppress ovulation in about half of women (they are slightly less effective). Both types cause a thickening of the cervical mucus, blocking sperm penetration.
Oral contraceptives are 92 - 99% effective. A woman can decide to start taking the pill if she is sexually active or planning to become sexually active and is certain she is not pregnant. Some pills are taken daily for 21 days and stopped for 7 days before starting a new package.
Other kinds are taken continuously for 28-day cycles. Oral contraceptives should be taken in order, at a convenient and consistent time each day. They are appropriate for women who are willing to use a method that requires action daily and who will be able to obtain supplies on a continuous basis.
The pill offers continuous protection against pregnancy, it produces regular and shorter periods (and frequently a decrease in menstrual cramps), and it protects against ovarian and endometrial cancer, ectopic pregnancies and infections of the fallopian tubes.
Possible side effects include nausea, breast tenderness, mild headaches, weight gain or loss. Very rarely, it can lead to serious health risks (e.g. blood clots, heart attack, and stroke). Risks are higher for women over 35 years who smoke.
The pill does NOT protect against sexually transmitted infections (STIs, including HIV). To protect against STIs, a male or female condom must be used.
Myth: There is a risk of birth defects
Some women who seek family planning incorrectly believe that using COCs will cause birth defects in their babies.
Fact:
Good evidence shows that COCs will not cause birth defects and will not otherwise harm the fetus if a woman becomes pregnant while taking COCs or accidentally starts to take COCs when she already pregnant.
Myth: The contraceptive pill can cause cancer
Some women who seek family planning believe that combined oral contraceptives (COCs) cause cancers such as breast cancer, uterine cancer, and ovarian cancer.
Fact:
The use of combined oral contraceptives (COCs) is proven to decrease the risk of two gynecological cancers (ovarian and endometrial). It is difficult to know the effect of COC use on breast cancer and cervical cancer. The possibly increased risks that have been recorded in some studies are not large enough to outweigh benefits or to change current practice.
Use of COCs helps protect women from two kinds of cancers—cancer of the ovaries and cancer of the lining of the uterus (endometrial cancer). This protection continues for 15 or more years after stopping use.
Breast cancer
Research findings about COCs and breast cancer are difficult to interpret. In studies, breast cancer is slightly more common among women using COCs and those who have used COCs in the past 10 years than among other women. Scientists do not know whether or not COCs actually caused the slight increase in breast cancers. It is possible that the cancers were already there before COC use but were found sooner in COC users. Both COC users and women who do not use COCs can have breast cancer.
Cervical cancer
Cervical cancer is caused by certain types of human papillomavirus (HPV). HPV is a common STI that usually clears on its own without treatment, but sometimes persists. Use of COCs for five years of more appears to speed up the development of persistent HPV infection into cervical cancer. The number of cervical cancers associated with COC use is thought to be very small. If cervical screening is available, providers can advise COC users—and all other women—to be screened every three years (or as national guidelines recommend) to detect precancerous changes in the cervix, which can be removed.
Myth: You will experience general health problems
Some women believe that COCs cause hair loss (alopecia), asthma, and headaches.
Fact:
A woman may experience short term side affects associated with use of combined oral contraceptive (COCs), including changes in bleeding patterns, headaches, and nausea. However such side effects are not a sign of illness, and usually stop within the first few months of using COCs. For a woman whose side effects persist, give her a different COC formulation. In women who are otherwise well, COC use may be continued for many years as there are no adverse effects related to long-term use.
In fact, there are also long-term non-contraceptive health benefits of using COCs as they:
- Help protect against cancer of the lining of the uterus (endometrial cancer)
- Help protect against cancer of the ovaries
- Help protect against symptomatic pelvic inflammatory disease
- May help protect against ovarian cysts
- May help protect against iron-deficiency anemia
- Reduce menstrual cramps
- Reduce menstrual bleeding problems
- Reduce ovulation pain
- Reduce excess hair on face or body
- Reduce symptoms of polycystic ovarian syndrome
- Reduce symptoms of endometriosis
Myth: There is confusion about how often and when to take the pill
Some women who seek family planning are misinformed about how often or when they should take the pill.
Fact:
A woman can start using COCs any time she wants if she is reasonably certain that she is not pregnant. To be reasonably certain a client is not pregnant, providers can use the Pregnancy Checklist.
If a client is starting her pack of pills within five days after the start of her menstrual period, there is no need for a backup method as she is immediately protected from pregnancy. If she starts COCs more than five days after the start of her menstrual period, she can start them any time it is reasonably certain she is not pregnant. She will need to use a "back up" method of contraception, such as a male or female condom, for the first seven days of taking pills to ensure protection from pregnancy.
The effectiveness of oral contraception depends on a regular intake of the hormones contained in the pill. Therefore pills must be taken daily, until the pack is empty. Although the specific time of day does not matter, the pills should be taken at the same time every day to reduce side effects and to help women remember to take their pills more consistently. The client should be advised not to interrupt taking the pills before a pack is finished, even if she does not have sexual intercourse. If the pills are taken correctly, the client will always start a new pack on the same day of the week. If a client is taking pills from a 21-pill pack, she will wait seven days after taking the last pill in the pack before beginning a new pack. If a client is taking pills from a 28-pill pack, she will take the next pill from the next pack on the very next day.
Women do not need to take a “rest” from COCs after taking them for a time. There is no evidence that taking a “rest” is helpful. In fact, taking a”rest” from COCs can lead to unintended pregnancy. COCs can safely be used for many years without having to stop taking them periodically.
Myth: There is a risk of infertility, or a delayed return to fertility
Women who seek family planning may incorrectly believe that using COCs will cause a long delay in conceiving or prevent them from being able to have children in the future.
Fact:
The combined oral contraceptive (COC) does not cause infertility. This is true regardless of how long a woman has taken the pill, the number of children the woman has had, or the age of the woman. In fact, some of the non-contraceptive benefits of the pill include preserving fertility by offering protection against pelvic inflammatory disease, endometriosis, and ectopic pregnancy.
There is no evidence that COCs delay a woman's return to fertility after she stops taking them. Women who stop using COCs can become pregnant as quickly as women who stop using non-hormonal methods.
Myth: Contraceptive pills can get absorbed into the wrong part of the body
Many women who seek family planning incorrectly believe that COCs accumulate in the body and cause diseases and tumors, or get stored in the stomach, ovaries, or uterus and form stones.
Fact:
After the pills are swallowed, they dissolve in the digestive system, and the hormones they contain are absorbed into the bloodstream. After they produce their contraceptive effect, the hormones are metabolised in the liver and gut and are then eliminated from the body. They do not accumulate in the body anywhere.
Myth: Contraceptive pills encourage 'promiscuity'
Some clients who seek family planning wrongly believe that the pill encourages infidelity, promiscuity, or prostitution in women.
Fact:
There is no evidence that COCs affect women’s sexual behavior. The evidence on contraception in general shows that sexual behavior is unrelated to contraceptive use. In fact, using contraception shows responsible behavior in order to avoid unintended pregnancy and sexually transmitted infections.
Myth: There will be an impact sexual desire and pleasure
Some clients who seek family planning may believe that COCs reduce sexual pleasure or interest in sex (loss of libido) or that they cause frigidity in women.
Fact:
There is no evidence that COCs affect a woman's sex drive. Although some women using the pill have reported either an increase or decrease in sexual interest and performance, it is difficult to say whether such changes are a result of COCs or other life events.
Myth: You will experience weight changes
Some clients believe that COCs cause women to gain or lose weight.
Fact:
Most women do not gain or lose weight as a result of COC use. A woman's weight may fluctuate naturally due to changes in age or life circumstance. Because changes in weight are common, many women attribute their natural weight gain or loss to the use of COCs. Although a very small number of COC users may report weight change following COC use, studies have found that, on average, COCs do not affect weight. A few women experience sudden changes in weight when using COCs. These changes reverse after they stop taking COCs. It is not known why these women respond to COCs this way.
when
Blog Series
Adolescent Health
Subject
Contraception