
Articles by Nepal
The Rainbow Wave for Marriage Equality
Love wins! The fight for marriage equality has seen incredible progress worldwide, with a recent surge in legalizations. Across the world, 36 out of 195 countries have legalized equal marriage: Andorra, Argentina, Australia, Austria, Belgium, Brazil, Canada, Chile, Colombia, Costa Rica, Cuba, Denmark, Ecuador, Estonia, Finland, France, Germany, Greece, Iceland, Ireland, Luxembourg, Malta, Mexico, the Netherlands, New Zealand, Norway, Portugal, Slovenia, South Africa, Spain, Sweden, Switzerland, Taiwan, the United Kingdom, the United States of America and Uruguay. In 2023, three new countries legalized same-sex marriage (Andorra, Estonia and Slovenia), and three more solidified legislative progress towards decriminalizing same-sex unions: a Japanese court ruled it is unconstitutional for the nation not to legally recognize same-sex unions. And the Supreme Courts of Nepal and Namibia recognized marriages of same-sex couples registered abroad. So marriage equality marches on! Already in 2024, two more countries have said "I do" to equal rights. According to the Human Rights Campaign Foundation, even more countries could legalize equal marriage in 2024. In particular, the Czech Republic, India, Japan, Nepal and Philippines show signs of growing support for marriage equality. The fight for marriage equality isn't over, but the momentum is undeniable. IPPF stands with those working to make love win everywhere.
Breaking Barriers: Inside Nepal’s First LGBTQIA+ Hormonal and Laser Therapy Clinic
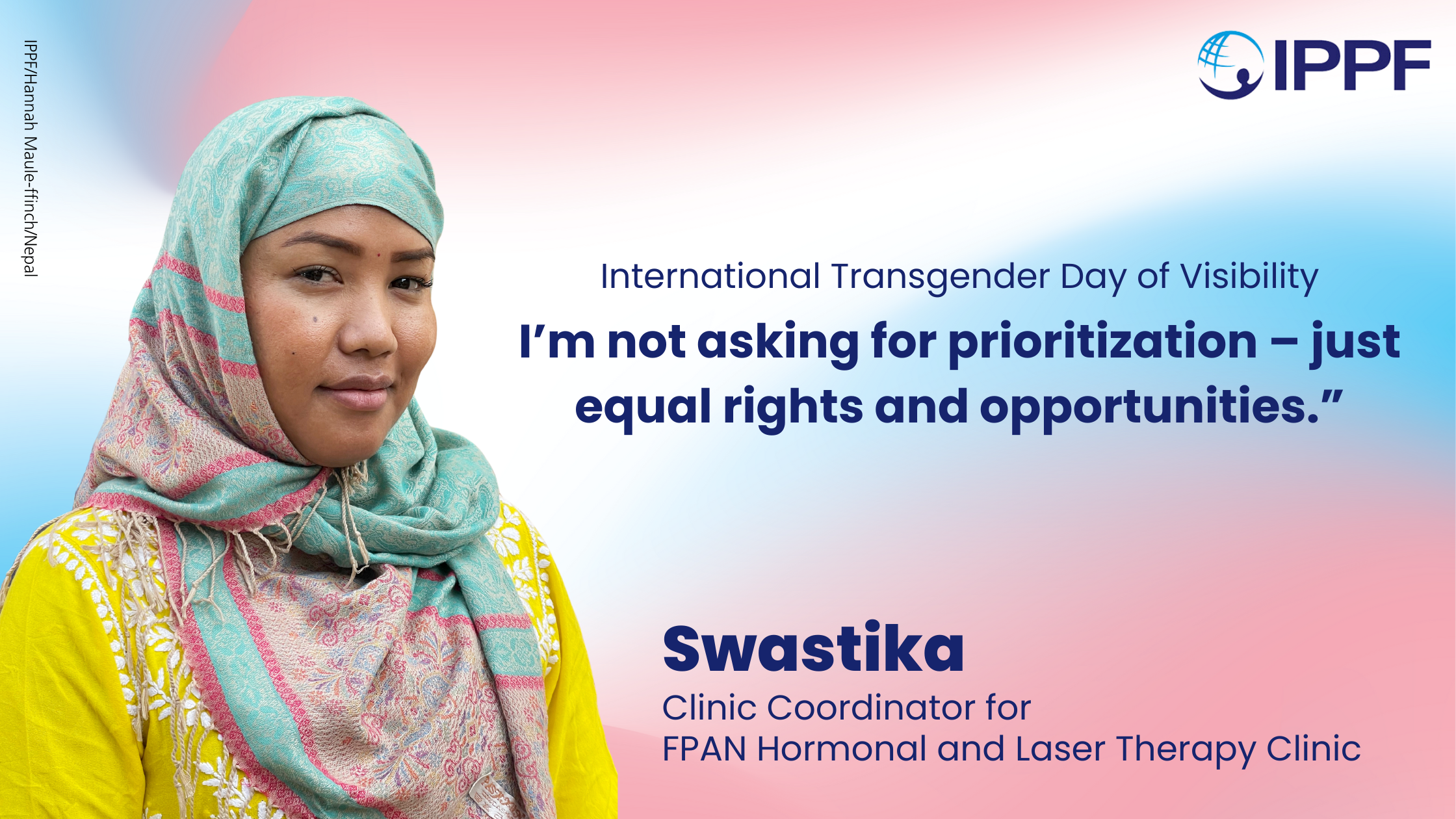
“In my mind, I only ‘came out’ once – from my mother’s womb,” says Swastika, a transgender activist and clinic coordinator of Nepal’s first Hormonal and Laser Therapy Clinic for LGBTQIA+ people. The clinic was established in 2022 in collaboration with IPPF’s member association, the Family Planning Association of Nepal (FPAN) and the Blue Diamond Society (BDS), Nepal’s pioneering LGBTQIA+ organization. Swastika’s journey as a transgender woman in Nepal has been a long one. She recalls leaving her family at the young age of 17 due to their initial rejection of her identity. “I know how much I have faced since my childhood; I have been bullied and sexually harassed, even after transitioning ... people in Nepal are slowly starting to accept our community, but there are still hurdles. For example, we are charged twice as much in rent than non-transgender people,” reflects Swastika. Nepal is often hailed as the ‘beacon of LGBTQIA+ rights in Asia’ and globally for its progressive laws towards gender and sexually diverse people. In a landmark 2007 Supreme Court decision (Blue Diamond Society and others v. Nepali Government), the court ordered the government to take three pivotal steps to strengthen the rights of LGBTQIA+ individuals: legally recognize a third gender category based on an individual’s self-identification; conduct a comprehensive audit of all laws to eliminate any discriminatory provisions against LGBTQIA+ people; and form a committee to study the legal recognition of same sex marriages. Following this ruling, the government implemented a directive allowing gender and sexually diverse individuals to specify their gender identity as ‘third gender’ or ‘other’ in official documents including citizenship, certificates, voter’s ID, passports and in the national census. However, despite these progressive steps, the reality on the ground is very different. Gender and sexually diverse people still face bureaucratic and legal hurdles when it comes to self-identification. Currently, there is no legal option for those seeking to change their gender marker from ‘male’ to ‘female’ or vice versa. Similarly, implementation of the policy to obtain legal documents marked ‘other’ is unclear and inconsistent. There have been instances reported where individuals seeking to change their marker to ‘other’ have been forced to undergo medical interventions as a form of ‘proof’ of their gender identity. These medical interventions are often obtrusive and traumatizing for the individual, with a team of doctors and professionals present as they undress and are physically examined, a procedure no cis-gendered person is obliged to undertake to ‘prove’ their sex. Although some transgender individuals have successfully obtained legal documents reflecting their self-identification as ‘male’ or ‘female’, medical evidence has still been required.

IPPF marks World AIDS Day by announcing the launch of a special program to roll out new biomedical HIV prevention methods
IPPF provides comprehensive sexual and reproductive health care to clients around the world. HIV testing, prevention, and treatment services are essential parts of our integrated sexual and reproductive health care package. To expand the choices individuals have to protect themselves from HIV, IPPF is excited to announce a special program to provide the newest methods of HIV prevention - injectable PrEP (a 2-monthly injection of cabotegravir-LA) and the vaginal ring (a monthly vaginal ring of dapivirine), as well as expanding where oral PrEP is offered. This program is being launched through a consortium of IPPF Member Associations called the Consortium to Advance Access to new HIV Prevention Products (CAAPP) - led by Family Planning Association of India, and including the Family Life Association of Eswatini, Lesotho Planned Parenthood Association, Family Planning Association of Malawi, Federation of Reproductive Health Associations, Malaysia, Family Planning Association of Nepal, and Planned Parenthood Association of Thailand. We hope this program will increase access to the number of ways people can protect themselves from HIV, supporting individual's choice to find an HIV prevention method that works for them.

लाज (Shame): Reflections on workshops to deconstruct pleasure
Amidst the different dos and don’ts of sex and desire, have you ever paused and thought - what does ‘pleasure’ mean to me? I asked the same question to participants in our workshop लाज (Shame): Deconstructing Pleasure. The aim of the workshop was to create an intentional space for our participants to redefine their desires, pleasures and intimacy beyond societal pressures. I conducted a total of 4 workshops in both Pokhara and Kathmandu, Nepal from December 2021 to May 2022. The workshops consisted of 60 AFAB (Assigned Female at Birth) participants, who came together to reflect on their relationship with pleasure, specifically self-pleasure, and deconstruct the guilt, shame and stigma associated with it in our Nepali society. Here are some of my reflections from facilitating these pleasure workshops, as well as four activities that can help you create your own pleasure practice: Understand pleasure beyond penetration In Nepal due to cultural taboos around sexuality, conversations around pleasure are often hushed and pushed to private spaces. The limited knowledge that does exist in public, defines pleasure as only accessible through penetrative sex (penis in vagina), which ideally should take place within a marriage. Since only 18.4% of people with vulvas orgasm through vaginal sex alone, this narrow understanding largely prioritises the sexual pleasure of cis-het men, creating a pleasure gap. Additionally, it erases queer expressions and practices of pleasure since it equates pleasure to only exist within heterosexual (opposite-sex) relationships. In order to decentralise this single narrative of pleasure, we started our workshop with The Pleasure Project’s prompt, “I get pleasure from…”. The prompt facilitated participants to take a step back and think about the activities they received pleasure from. The answers we received included both sexual and non-sexual activities, ranging from masturbation, to eating, to reading books. This activity allowed us to establish that the only universality to pleasure is that it is subjective to each one of us and our unique needs. It also helped us expand the narrow understanding of pleasure and emphasise the importance of non-sexual activities in our pleasure script. While pleasure innately is not sexual, given the taboo, the workshop then proceeded to encourage participants to think about their experiences specifically related to sexual pleasure.

Tackling Taboos and the Fear of Using a Menstrual Cup
In many cultures and societies, individuals with vaginas are accustomed to thinking that touching and peeking at their genitals is inappropriate or that taking ownership and autonomy of our own body and pleasure seems a whimsical story. The way we are constantly lectured about our bodies has informed our ideas and attitudes around sexual and reproductive health, particularly menstrual health. I live in Nepal, where menstruation has been, and still is, a taboo. A few years ago, I signed up for the social networking platform Clubhouse, where I joined virtual ‘rooms’ where people talked openly about menstruation and menstrual cups. Being a newbie to menstrual cups while at the same time advocating their use, I felt proud and excited every time I shared or heard people talking about it.

SPRINT: Sexual and reproductive health in crisis and post-crisis situations
The SPRINT Initiative provides one of the most important aspects of humanitarian assistance that is often forgotten when disaster and conflicts strike: access to essential life-saving sexual and reproductive health services. We build capacity of humanitarian workers to deliver essential life-saving sexual and reproductive health services in crisis and post-crisis situations through the delivery of the Minimum Initial Service Package (MISP) for reproductive health in emergencies. Through funding from the Australian Government's Department of Foreign Affairs and Trade (DFAT), our SPRINT Initiative has brought sexual and reproductive health to the humanitarian agenda, increased capacity and responded to a number of humanitarian emergencies. Australia has funded the SPRINT initiative since 2007. Since then, the SPRINT initiative has responded to 105 humanitarian crises and worked with partners in 99 countries. SPRINT has reached over 1,138,175 people, delivering 2,133,141 crucial SRH services, and continues to respond to ongoing emergencies. In each priority country, we work with an IPPF Member Association to coordinate and implement life-saving sexual and reproductive activities. Through these partnerships, SPRINT helps strengthen the enabling environment, improve national capacity and provide lifesaving services during times of crisis. You can read more about IPPF Humanitarian’s Programme here. Australia's location in the Indo-Pacific provides DFAT with a unique perspective on humanitarian action. Australia is committed to helping partner governments manage crisis response themselves. This is done through building the capacity of the national government and civil society to be able to respond to disaster. DFAT also works with experienced international partners to prepare for and respond to disasters, including other donors, United Nations agencies, the International Red Cross and Red Crescent Movement and non-government organisations.

Nepal: Ensuring safe and compassionate SRH services for sex workers during COVID-19
“Even though we know we shouldn’t be ashamed to seek medical treatments, sometimes we are ashamed to go to clinics for check-ups,” said Dhriti* (pictured above), a 24-year-old sex worker in Kathmandu, Nepal. In nearly every country around the world, the stigmatization of sex workers creates barriers to sex workers accessing sexual and reproductive healthcare. These barriers have been compounded and exacerbated throughout the COVID-19 pandemic as a result of lockdown measures and the diversion of medical staff and resources. As a result, many young sex workers like Dhriti – who have a heightened risk of contracting COVID-19 due to the nature of the work – are reluctant to come forward and seek help, and they are largely excluded from government pandemic response measures and programs. 22-year-old Anisha* is also a sex worker in Kathmandu. She added that during the lockdown, many sex workers faced significant or total loss of income and were forced to put themselves at risk to earn enough money to eat. “We lied to police officers at checkpoints in the city and made our way to places where we could get our clients,” she said. “We were scared because of the coronavirus but there was no work or money for us.”

'Khaskhus': an innovative group chat in Nepal supports people living with disabilities during COVID-19
“Menstruation does not stop just because of lockdown,” says Sanjiya Shrestha (pictured), a Peer Educator at the Family Planning Association of Nepal, an IPPF Member Association. But when the second wave of the COVID-19 pandemic hit Nepal in early 2021, it had a profound impact on the lives of women, girls and people living with disabilities. Strict measures imposed during the country’s second national lockdown restricted access to and availability of essential sexual and reproductive health services including sanitary kits, maternal health care, safe delivery services, contraception, abortion services, and many others. “During COVID-19, we were not able to be close to anyone or touch each other. Even getting outside to buy sanitary items was difficult,” said Shrestha, who is visually impaired. “But some people with disabilities require care from others, and they need to be close together. It was difficult for people in wheelchairs and visually impaired people to get outside. In that way, the pandemic has had an even greater impact on people with disabilities.” Greater need brings innovation The Family Planning Association of Nepal (FPAN) works with over 200 clinical service providers and over 600 community-based distributors to ensure women and girls get access to essential SRH services during this critical health emergency. With the support of the Australian Government, FPAN has also partnered with a number of community-based organizations including the Blind Youth Association Nepal, the Nepal Disabled Women Association, Community Based Rehabilitation and Action on Disability Rights and Development Nepal. Part of Shrestha’s work as a peer educator is to regularly conduct training sessions to educate people about gender and sexual and reproductive health issues. She also organizes health camps in rural communities and explains contraceptives and birth control measures for people living with disabilities. But during the lockdown, she needed an innovative way to communicate with vulnerable people and ensure they get access to reliable sexual and reproductive health information and services. Shrestha decided to launch a talk and text group chat, which she named ‘Khaskhus’, or ‘special talk’, in English. “There are some things that cannot be covered in trainings and seminars, but these gaps can be filled by this group,” she said. At first, the group was made up of visually-impaired youth, but Shrestha says it has grown to include a range of different people. “Now, everyone who is interested can join and share with those around them. Through this group, we talk about sexual and reproductive health, life skills, and development. Everyone in our group talks openly... we share our experiences and we have learned many new things from this discussion.” Direct and inclusive support As government-imposed movement restrictions gradually loosen in Nepal, FPAN staff and volunteers continue to meet the needs of community members by providing essential SRH materials and services, such as condoms, pills and emergency contraceptive, pregnancy tests, and referrals for sexually transmitted infections and abortion cases to an FPAN branch clinic. Thirty-year-old Sunita Duwal lives with a physical disability. Her husband, Suman Palikhel, uses a wheelchair. The couple receives information from FPAN on family planning and reproductive health and they volunteer by coordinating home deliveries of essential items across the capital, Kathmandu. “I used to feel a little hesitant and ashamed to talk about these issues,” said Palikhel. “But FPAN has brought about some changes in our lives... we even share this information with others.” Duwal said the organization has played a crucial role in educating people about COVID-19 and delivering essentials directly to vulnerable people. “One of my friends told us that during the coronavirus period, she was experiencing continued bleeding from her menstrual cycle. We shared this issue with FPAN and they sent a technical person to help her,” she said. “There was another physically disabled person with a spinal injury who needed diapers and a catheter. During the lockdown period, we delivered much-needed items such as masks, sanitizers, gloves, face shields, Dettol and soap to people’s homes.” Since June 2021, FPAN has been working in 15 districts most affected by COVID-19 through 15 family health clinics, 15 community clinics and 210 volunteer-run community-based distribution outlets. As part of its emergency response to the COVID-19 pandemic in Nepal, FPAN is filling an important gap as a result of the diversion of medical equipment and staff that were usually involved in SRH delivery services to fulfil other emergency health needs. “This support has brought about a lot of change for us,” said Duwal. “We have learned that without sharing our problems and having a two-way communication, we cannot solve our problems. This outlook has helped us out.”

Aid cuts could lead to more than two million unintended pregnancies before the end of the year in continued blow for women and girls
New data from the International Planned Parenthood Federation (IPPF) has revealed that unless alternative funding is sourced, the UK government's £131 million ($186 million) cut to UNFPA supplies – the largest provider of donated contraception for some of the world's poorest communities - will lead to an estimated additional: 2.4 million unintended pregnancies 685,000 unsafe abortions and 7,447 maternal deaths across IPPF's services alone before the end of 2021.[i] IPPF uses donations of contraception from UNFPA supplies, including the pill, injectables, implants, IUDs, and condoms, to deliver much-needed sexual and reproductive healthcare across 45[ii] countries via its Member Associations (M.A.s). For 2021, IPPF has received just $1.5 million worth of contraception out of the $14 million requested for the year. It is growing increasingly concerned that the remaining $12.5 million worth of contraception will no longer be available, meaning Member Associations will be dangerously close to running out of stock by the end of 2021, with shortages becoming increasingly acute for 2022 unless replacement funding can be found. The $14 million equates to 40% of IPPF's overall budget of $35 million for contraceptive supplies across the entire Federation. Some IPPF Member Associations have reported that they are 100% reliant[iii] on the millions of dollars worth of contraception they receive from UNFPA Supplies, including M.A.s in Nepal, Cameroon, Cote d'Ivoire, Mozambique, Yemen, and South Sudan. For others, donations from UNFPA form a significant part of their budgets, such as M.A.s in Ethiopia, Ghana, Mali, Malawi, Nigeria, and Sudan. Furthermore, with the gap between procurement of contraception and supply often taking six months or more, and with UNFPA Supplies also the primary provider for Ministries of Health in the countries that IPPF and UNFPA work with, other avenues for Member Associations to receive contraception and commodities are also severely restricted. The crushing figures come on top of already devastating news for IPPF, the world's largest sexual and reproductive healthcare organization, which saw cuts of around £72 million, approximately $100 million at the end of April. These cuts include the dismantling of the U.K.'s hugely successful WISH (Women's Integrated Sexual Health) programme just three years into its creation, as well as the closure of IPPF's ACCESS (Approaches in Complex and Challenging Environments For Sustainable Sexual and Reproductive Health) programme. Both initiatives help deliver life-saving contraception and sexual and reproductive healthcare for some of the most marginalized women and girls, including those living in poverty, refugees, those living with HIV, and survivors of sexual and gender-based violence. In some of the 45 countries, IPPF works with UNFPA Supplies alongside the WISH and ACCESS programmes. Dr Alvaro Bermejo, IPPF’s Director-General, said: "Millions of women[iv] in the world's poorest countries want to access contraception but can't, and this number will only increase following the U.K government's decision to axe hundreds of millions of promised pounds from the expert organizations that provide sexual and reproductive healthcare worldwide. "Not only are the government dismantling well-established healthcare clinics and teams, but they are also stripping the remaining ones of valuable resources with little to no notice. Soon, healthcare teams will be left with nothing to give the women and girls who come to clinics for contraception, inevitably leading to millions of unintended pregnancies, thousands of unsafe abortions, and thousands of maternal deaths. "While the government has presented these cuts as inevitable, no other country has slashed international aid in this way, and it will take years to rebuild programmes and regain the trust of devastated communities. "What the government fails to recognize is that cuts to a body like UNFPA Supplies have a devastating ripple effect through the entire global healthcare ecosystem, weakening it in the process. This naive and short-sighted decision will have long-lasting consequences, with the lives of thousands of women and girls lost in the process." Manuelle Hurwitz, Director of Programmes, added: "Not only are these cuts a disgrace, but they completely contradict the U.K government's 'priorities' of gender equality and getting 40 million more girls into education by 2025. Because how can a girl stay in school if she is pregnant before she is 16? "It is especially galling that this comes at the time when the U.K government, as leaders of the G7 summit, will urge nations to "build back better" after the coronavirus pandemic while choosing to abandon the poorest women and girls in the world's darkest hour." In the wake of the continued blows for women and girls worldwide, IPPF is asking the government to urgently recommit to setting aside 0.7% of the U.K.'s national income for international aid, as per its legal commitments. Programme delivery on hold Since its launch in 2008, UNFPA supplies, alongside IPPF and other partners, has helped prevent: 89 million unintended pregnancies 26.8 million unsafe abortions 227,000 maternal deaths[v] But the unexpected level of cuts in the middle of the financial year now means services and deliveries are on hold while partners grapple with the overwhelming task of securing funds for contraception and medical supplies. Dr Naresh Pratap is the Executive Director for the Family Planning Association Nepal (FPAN), one of IPPF's Member Associations. FPAN is heavily reliant on UNFPA Supplies, with 100% of its average annual commodities budget of $700,000[viii] supported by UNFPA donations. Nepal has also been affected by the ACCESS programme's immediate closure and is subject to ongoing humanitarian crises due to its geographic remoteness, natural hazards, limited healthcare capacity and one-quarter of the nation living in extreme poverty. He said: "At the time when Nepal has already been affected by Trump's Gag Rule and gripped by the COVID-19 pandemic, the funding cuts to UNFPA supplies will mean that millions of people on the ground will struggle to access contraception. As an organization that depends heavily on UNFPA supplies and has been hard-hit by the recent closure of the ACCESS programme, the U.K. government's funding cut has further exacerbated FPAN's capacity to serve underprivileged people in urgent need of sexual and reproductive healthcare services – it is unacceptable and beyond humanity." Investing in women means investing in sexual and reproductive healthcare With 120 million people about to be pushed back into extreme poverty due to the global pandemic, and women and girls already suffering the pandemic's effects disproportionately compared to men, the cuts have come at one of the most challenging times for nations around the world. If countries are to build back better after the coronavirus pandemic, investing in sexual and reproductive healthcare is one of the best ways to break the cycle of poverty. As the U.K. heads into the G7 summit, leadership, commitment and intelligent forward-thinking is needed now, more than ever. "These cuts will be devastating for women and girls and their families across the world," said UNFPA Executive Director Dr Natalia Kanem in a statement about the cuts. "UNFPA recognizes the challenging situation facing many donor governments, yet deeply regrets the decision of our longstanding partner and advocate to step away from its commitments at a time when inequalities are deepening, and international solidarity is needed more than ever. "The truth is that when funding stops, women and girls suffer, especially the poor, those living in remote, underserved communities and those living through humanitarian crises. The needs of women and girls and their right to modern contraceptives have not changed, and UNFPA remains resolute and dedicated to our mandate." [i] Internal data from IPPF calculated using the pending $12.5 million pending request from UNFPA supplies. [ii] The 45 countries include: Afghanistan, Benin, Burkina-Faso, Burundi, Cameroon, Cambodia, CAR, Chad, Comoros, Congo, Cote d'Ivoire, Djibouti, DR Congo, Ethiopia, Ghana, Guinea-Conakry, Guinea-Bissau, Kyrgyzstan, Laos, Lesotho, Liberia, Madagascar Mali, Malawi, Mauritania, Mozambique, Myanmar, Nepal, Niger, Nigera, Pacific Island Countries (Cook Islands, Fiji, Kiribati, Samoa, Solomon Islands, Tonga, Tuvalu, Vanuatu) Papua New Guinea, Sao Tome & Principe, Senegal, Sierra Leone, Somaliland, South Sudan, Sudan, Tajikistan, Tanzania, Togo, Uganda, Yemen,Zambia and Zimbabwe. [iii] MA’s 100% reliant on donations from UNFPA include Cameroon, Cote d'Ivoire, Guinea Conakry, Nepal, Samoa, Sierra Leone, South Sudan and Yemen. [iv] 217 million women who want to avoid pregnancy have an unmet need for contraception. [v] Internal data from IPPF calculated using 2020 actual donation and 2021 requested value

In pictures: Innovating during COVID-19
Women around the world have faced multiple barriers to accessing safe abortion care during the COVID-19 pandemic including the de-prioritization of sexual and reproductive healthcare, overwhelmed health systems and restrictions on movement. The COVID-19 crisis has sparked innovation among IPPF Member Associations who responded swiftly by developing new approaches to reach women with safe abortion care including telemedicine and home-based provision of medical abortion. Strong evidence generated from this work supports the continuation and strengthening of these approaches beyond the end of the pandemic. Cameroon Cameroon National Planning Association for Family Welfare (CAMNAFAW) To ensure that quality abortion care can be provided to women during travel restrictions, CAMNAFAW’s service providers travel to partner clinics in underserved areas and to clients’ homes to provide medical and surgical abortion care. This model of taking safe abortion care closer to women will continue even with easing of travel restrictions, as this has been found to be an effective and acceptable approach to increasing access.Photo: IPPF/Xaume Olleros/Cameroon Share on Twitter Share on Facebook Share via WhatsApp Share via Email Guinea Association Guinéenne pour le Bien-Etre Familial (AGBEF) Building on lessons learned during the Ebola crisis in Guinea, AGBEF quickly took measures to prevent infection in its clinics to continue providing sexual and reproductive healthcare, including surgical and medical abortion, in a safe environment. AGBEF donated protective materials to communities, including hand-washing stations, face masks and antibacterial gel, alongside messaging on infection prevention. This community visibility reassures clients they can safely attend AGBEF clinics for abortion and contraceptive care.Photo: AGBEF/Guinea Share on Twitter Share on Facebook Share via WhatsApp Share via Email India Family Planning Association of India (FPA India) FPA India and partners advocated to have sexual and reproductive healthcare, including abortion, recognized as essential by the government, which meant FPA India could continue healthcare delivery during the national lockdown. To reduce in-person clinic visits, FPA India established teleconsultation and counselling for abortion care, and is continuing to provide in-clinic care for both medical and surgical abortion. Photo: IPPF/Alison Joyce/India Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nepal Family Planning Association of Nepal (FPAN) FPAN and partners advocated for interim approval of home provision of medical abortion and telemedicine for abortion counselling during COVID-19. FPAN is now implementing these approaches, ensuring continued access to abortion care in Nepal, where many people live in remote locations with limited mobility, which has been further restricted by COVID-19 lockdowns. Photo: FPAN/Nepal Share on Twitter Share on Facebook Share via WhatsApp Share via Email Pakistan Rahnuma – Family Planning Association of Pakistan (Rahnuma-FPAP) Rahnuma-FPAP and partners successfully advocated for the government to class sexual and reproductive healthcare as ‘essential’, which enabled the team to continue providing post-abortion care during the pandemic. Rahnuma-FPAP expanded its telemedicine and home-based provision for menstrual regulation counselling and post-abortion care. These new approaches have ensured continued access to services for clients unable to reach clinics.Photo: Rahnuma-FPAP/Pakistan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Palestine Palestinian Family Planning and Protection Association (PFPPA) In response to the government-mandated closure of its clinics, PFPPA quickly established a toll-free call centre which provides consultations, counselling, referrals and follow-up, including consultation for abortion care through a harm reduction approach, ensuring that women are provided with accurate information. Due to its success, PFPPA is exploring options for continuing this healthcare delivery model beyond the pandemic, with the aim of keeping it free of charge for users.Photo: SAAF/Samar Hazboun/Palestine Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sudan Sudan Family Planning Association (SFPA) Following a nation-wide shutdown in April, SFPA established a call centre to increase access to healthcare, including abortion and contraceptive counselling and referrals. An unexpected outcome of the new call centre is that it has reached an increased number of young women who regularly call to discuss their reproductive health and rights. SFPA is working towards institutionalizing this model for continuation beyond the pandemic.Photo: SFPA/Sudan Share on Twitter Share on Facebook Share via WhatsApp Share via Email Togo Association Togolaise pour le Bien-Etre Familial (ATBEF) ATBEF adapted its mobile application ‘Infos Ado Jeunes’, adding a toll-free teleconsultation service for young clients to use to access abortion consultations and pre- and post-abortion counselling. This app has given young clients ongoing access to care when they face challenges travelling to clinics. It has also eased overall client flow in clinics at a time when social distancing is being implemented.Photo: ATBEF/Togo Share on Twitter Share on Facebook Share via WhatsApp Share via Email
Pagination
- Page 1
- Next page







