Spotlight
A selection of stories from across the Federation

Advances in Sexual and Reproductive Rights and Health: 2024 in Review
Let’s take a leap back in time to the beginning of 2024: In twelve months, what victories has our movement managed to secure in the face of growing opposition and the rise of the far right? These victories for sexual and reproductive rights and health are the result of relentless grassroots work and advocacy by our Member Associations, in partnership with community organizations, allied politicians, and the mobilization of public opinion.
Most Popular This Week

Advances in Sexual and Reproductive Rights and Health: 2024 in Review
Let’s take a leap back in time to the beginning of 2024: In twelve months, what victories has our movement managed to secure in t
Kazakhstan

Kazakhstan's Rising HIV Crisis: A Call for Action
On World AIDS Day, we commemorate the remarkable achievements of IPPF Member Associations in their unwavering commitment to combating the HIV epidemic.

Ensuring SRHR in Humanitarian Crises: What You Need to Know
Over the past two decades, global forced displacement has consistently increased, affecting an estimated 114 million people as of mid-2023.
Estonia, Nepal, Namibia, Japan, Thailand

The Rainbow Wave for Marriage Equality
Love wins! The fight for marriage equality has seen incredible progress worldwide, with a recent surge in legalizations.
France, Germany, Poland, United Kingdom, United States, Colombia, India, Tunisia

Abortion Rights: Latest Decisions and Developments around the World
Over the past 30 years, more than

Palestine

In their own words: The people providing sexual and reproductive health care under bombardment in Gaza
Week after week, heavy Israeli bombardment from air, land, and sea, has continued across most of the Gaza Strip.
Vanuatu

When getting to the hospital is difficult, Vanuatu mobile outreach can save lives
In the mountains of Kumera on Tanna Island, Vanuatu, the village women of Kamahaul normally spend over 10,000 Vatu ($83 USD) to travel to the nearest hospital.
Filter our stories by:
- Associação Moçambicana para Desenvolvimento da Família
- (-) Association Togolaise pour le Bien-Etre Familial
- (-) Family Guidance Association of Ethiopia
- Family Planning Association of Malawi
- Family Planning Association of Nepal
- Foundation for the Promotion of Responsible Parenthood - Aruba
- Jamaica Family Planning Association
- Lesotho Planned Parenthood Association
- Planned Parenthood Association of Ghana
- Planned Parenthood Federation of Nigeria
- Reproductive Health Uganda
- Vanuatu Family Health Association


| 16 July 2020
"Before, there was no safe abortion"
Rewda Kedir works as a midwife in a rural area of the Oromia region in southwest Ethiopia. Only 14% of married women are using any method of contraception here. The government hospital Rewda works in is supported to provide a full range of sexual and reproductive healthcare, which includes providing free contraceptives and comprehensive abortion care. In January 2017, the maternal healthcare clinic faced shortages of contraceptives after the US administration reactivated and expanded the Global Gag Rule, which does not allow any funding to go to organizations associated with providing abortion care. Fortunately in this case, the shortages only lasted a month due to the government of the Netherlands stepping in and matching lost funding. “Before, we had a shortage of contraceptive pills and emergency contraceptives. We would have to give people prescriptions and they would go to private clinics and where they had to pay," Rewda tells us. "When I first came to this clinic, there was a real shortage of people trained in family planning. I was the only one. Now there are many people trained on family planning, and when I’m not here, people can help." "There used to be a shortage of choice and alternatives, and now there are many. And the implant procedures are better because there are newer products that are much smaller so putting them in is less invasive.” Opening a dialogue on contraception The hospital has been providing medical abortions for six years. “Before, there was no safe abortion," says Rewda. She explains how people would go to 'traditional' healers and then come to the clinic with complications like sepsis, bleeding, anaemia and toxic shock. If they had complications or infections above nine weeks, Rewda and her colleagues would send them to Jimma, the regional capital. "Before, it was very difficult to persuade them to use family planning, and we had to have a lot of conversations. Now, they come 45 days after delivery to speak to us about this and get their babies immunised," she explains. "They want contraceptives to space out their children. Sometimes their husbands don’t like them coming to get family planning so we have to lock their appointment cards away. Their husbands want more children and they think that women who do not keep having their children will go with other men." "More kids, more wealth" Rewda tells us that they've used family counselling to try and persuade men to reconsider their ideas about contraception, by explaining to them that continuously giving birth under unsafe circumstances can affect a woman's health and might lead to maternal death, damage the uterus and lead to long-term complications. "Here, people believe that more kids means more wealth, and religion restricts family planning services. Before, they did not have good training on family planning and abortion. Now, women that have abortions get proper care and the counseling and education has improved. There are still unsafe abortions but they have really reduced. We used to see about 40 a year and now it’s one or two." However, problems still exist. "There are some complications, like irregular bleeding from some contraceptives," Rewda says, and that "women still face conflict with their husbands over family planning and sometimes have to go to court to fight this or divorce them.”

| 17 May 2025
"Before, there was no safe abortion"
Rewda Kedir works as a midwife in a rural area of the Oromia region in southwest Ethiopia. Only 14% of married women are using any method of contraception here. The government hospital Rewda works in is supported to provide a full range of sexual and reproductive healthcare, which includes providing free contraceptives and comprehensive abortion care. In January 2017, the maternal healthcare clinic faced shortages of contraceptives after the US administration reactivated and expanded the Global Gag Rule, which does not allow any funding to go to organizations associated with providing abortion care. Fortunately in this case, the shortages only lasted a month due to the government of the Netherlands stepping in and matching lost funding. “Before, we had a shortage of contraceptive pills and emergency contraceptives. We would have to give people prescriptions and they would go to private clinics and where they had to pay," Rewda tells us. "When I first came to this clinic, there was a real shortage of people trained in family planning. I was the only one. Now there are many people trained on family planning, and when I’m not here, people can help." "There used to be a shortage of choice and alternatives, and now there are many. And the implant procedures are better because there are newer products that are much smaller so putting them in is less invasive.” Opening a dialogue on contraception The hospital has been providing medical abortions for six years. “Before, there was no safe abortion," says Rewda. She explains how people would go to 'traditional' healers and then come to the clinic with complications like sepsis, bleeding, anaemia and toxic shock. If they had complications or infections above nine weeks, Rewda and her colleagues would send them to Jimma, the regional capital. "Before, it was very difficult to persuade them to use family planning, and we had to have a lot of conversations. Now, they come 45 days after delivery to speak to us about this and get their babies immunised," she explains. "They want contraceptives to space out their children. Sometimes their husbands don’t like them coming to get family planning so we have to lock their appointment cards away. Their husbands want more children and they think that women who do not keep having their children will go with other men." "More kids, more wealth" Rewda tells us that they've used family counselling to try and persuade men to reconsider their ideas about contraception, by explaining to them that continuously giving birth under unsafe circumstances can affect a woman's health and might lead to maternal death, damage the uterus and lead to long-term complications. "Here, people believe that more kids means more wealth, and religion restricts family planning services. Before, they did not have good training on family planning and abortion. Now, women that have abortions get proper care and the counseling and education has improved. There are still unsafe abortions but they have really reduced. We used to see about 40 a year and now it’s one or two." However, problems still exist. "There are some complications, like irregular bleeding from some contraceptives," Rewda says, and that "women still face conflict with their husbands over family planning and sometimes have to go to court to fight this or divorce them.”

| 01 July 2020
In pictures: Ensuring confidentiality, safety, and care for sex workers
Meseret* and Melat*, volunteers Known in their local community as demand creators, Meseret and Melat, from the Family Guidance Association of Ethiopia’s (FGAE) confidential clinic head out to visit sex workers in Jimma town. This group of volunteers are former, or current, sex workers teaching others how to protect themselves from sexually transmitted infections (STIs) and unintended pregnancy. Their work is challenging, and they travel in pairs for safety - their messages are not always welcome. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Meseret* and Melat*, volunteers Meseret and Melat from the Jimma clinic talk to sex workers in their local community about sexual health concerns, as well as provide contraception. “It’s very difficult to convince sex workers to come to the clinic. Some sex workers tend to have no knowledge, even about how to use a condom.” says Meseret. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Melat, volunteer It can be challenging persuading women that the staff at the confidential clinic are friendly towards sex workers and will keep their information private. “When we try to tell people about HIV we can be insulted and told: ‘You are just working for yourself and earn money if you bring us in.’ They sometimes throw stones and sticks at us,” said 25-year-old Melat. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Fantaye, sex worker Getting information and contraception to women often involves going out to find them, such as Fantaye, a sex worker currently living in a rental space in Mekelle. Peer educators focus on areas populated with hotels and bars and broker's houses, where sex workers find clients. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sister Mahader, FGAE Sister Mahader from FGAEs' youth centre talks to sex workers in Mekelle, about sexual health, wellbeing, and various methods of contraception. This outreach takes place weekly where information and advice is given to groups of women, and contraception is provided free of charge. Under threat from the loss of funding from the US Administration, the Jimma clinic has been forced to reduce the range of commodities available to its clients such as sanitary products, soap and water purification tablets. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Hiwot Abera*, sex worker Hiwot* after her appointment at FGAEs confidential clinic in Jimma. The clinic offers free and bespoke healthcare including HIV and STI testing, treatment and counselling, contraceptives and safe abortion care. Many sex workers have experienced stigma and discrimination at other clinics. In contrast, ensuring confidentiality and a safe environment for the women to talk openly is at the heart of FGAEs’ healthcare provision at its clinics.*pseudonymPhotos: ©IPPF/Zacharias Abubeker Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 17 May 2025
In pictures: Ensuring confidentiality, safety, and care for sex workers
Meseret* and Melat*, volunteers Known in their local community as demand creators, Meseret and Melat, from the Family Guidance Association of Ethiopia’s (FGAE) confidential clinic head out to visit sex workers in Jimma town. This group of volunteers are former, or current, sex workers teaching others how to protect themselves from sexually transmitted infections (STIs) and unintended pregnancy. Their work is challenging, and they travel in pairs for safety - their messages are not always welcome. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Meseret* and Melat*, volunteers Meseret and Melat from the Jimma clinic talk to sex workers in their local community about sexual health concerns, as well as provide contraception. “It’s very difficult to convince sex workers to come to the clinic. Some sex workers tend to have no knowledge, even about how to use a condom.” says Meseret. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Melat, volunteer It can be challenging persuading women that the staff at the confidential clinic are friendly towards sex workers and will keep their information private. “When we try to tell people about HIV we can be insulted and told: ‘You are just working for yourself and earn money if you bring us in.’ They sometimes throw stones and sticks at us,” said 25-year-old Melat. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Fantaye, sex worker Getting information and contraception to women often involves going out to find them, such as Fantaye, a sex worker currently living in a rental space in Mekelle. Peer educators focus on areas populated with hotels and bars and broker's houses, where sex workers find clients. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sister Mahader, FGAE Sister Mahader from FGAEs' youth centre talks to sex workers in Mekelle, about sexual health, wellbeing, and various methods of contraception. This outreach takes place weekly where information and advice is given to groups of women, and contraception is provided free of charge. Under threat from the loss of funding from the US Administration, the Jimma clinic has been forced to reduce the range of commodities available to its clients such as sanitary products, soap and water purification tablets. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Hiwot Abera*, sex worker Hiwot* after her appointment at FGAEs confidential clinic in Jimma. The clinic offers free and bespoke healthcare including HIV and STI testing, treatment and counselling, contraceptives and safe abortion care. Many sex workers have experienced stigma and discrimination at other clinics. In contrast, ensuring confidentiality and a safe environment for the women to talk openly is at the heart of FGAEs’ healthcare provision at its clinics.*pseudonymPhotos: ©IPPF/Zacharias Abubeker Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 25 February 2019
In pictures: Togo and the rise in contraception use
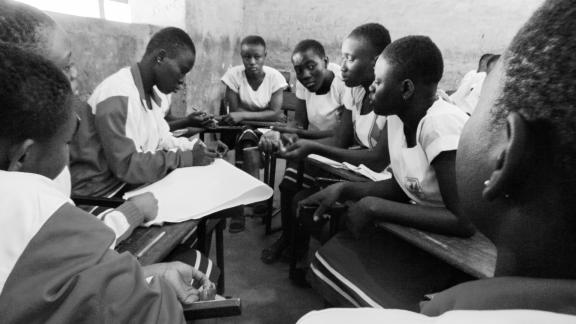
Félicité Sonhaye ATBEF Regional Coordinator The Association Togolaise pour le Bien-Être Familial (ATBEF), has led a pioneering programme training community health workers to administer contraception in the rural areas where they live. “The injection is used more than any other method. Around 60% of women use it,” said Félicité Sonhaye, ATBEF Regional Coordinator for Togo’s Plateaux region, which covers Ilama. “Women appreciate the reliability and long-lasting effects of the injection, which allow them to stop worrying about unexpected pregnancies”, Sonhaye added. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sossou Sagna Ilama village chief Men like Sossou Sagna, have great influence and respect within Togo’s rural communities. As Ilama’s village chief his approval was required for the ATBEF community project to take root. “I sent my own wife to seek family planning. The lady helped us and it worked really well. I also went with my older brother’s wife and she was very satisfied. Every member of this community is now aware that having a large family drives them towards poverty. Ignorance was the reason why we had so many children per family here before. Now with the family planning advice we have received, spacing births has become a reality and the reduction of the number of children per family.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Abla Abassa Community health worker Abla is a community health worker, and spends her days cycling around Ilama’s dusty streets visiting households that have signed up to an innovative programme providing contraception in hard-to-reach places. “Before, people didn’t have a lot of information about contraception. With the project the community is now able to space their births. I have seen the number of children per family going down. That’s contraception but also the increasing cost of living, and the fact that everyone wants to send their children to school.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Essivi Koutchona Client Facing prohibitive costs of school fees and food prices for six children, Essivi Koutchona, began using the contraceptive injection after deciding with her husband they did not want another child. She has received the injection every three months and has not experienced any side effects. “The community health worker passed by our house one day and explained the method and a bit about the possible side effects. We agreed as a couple that we wanted me to start using the injection.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Edem Badagbo Client 33-year-old Edem is a widowed father of three children. Edem hopes to have a vasectomy within the next month or so. His wife died following the birth of their third child but he is adamant he wants to follow through with a procedure they agreed upon before her death. “My wife agreed with the idea. I was scared when I first heard of it, but that’s because there was so little information available. When I came to the ATBEF clinic I received a lot more detail and that’s when I decided to do it. I have three children. That’s enough.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Yaori Ajossou Vasectomy client Yaori Ajossou, a retired soldier, heard about vasectomy while listening to an ABTEF awareness raising campaign on the radio. It prompted him to take on the responsibility for family planning in his marriage. “Before I had the idea that maybe I'd want to have more children, but after the campaign, and after my wife had talked a little bit about her health problems, I thought, well, maybe it's better to put the brakes on. I was about to retire. Why carry on having children? Six children is already a lot. It's already maybe too many.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Dede Koussawo Client 34-year-old Dede visits the ATBEF clinic in Lomé, Togo with her husband, Edem. “We do this together if his schedule permits it. I asked and he accepted. It's not typical (for men to come). Before the pregnancy, I was taking the pill. Before the first I was taking the pill and I used an IUD after my son's birth and after my daughter's birth as well. We've been really happy with the family planning we've got here so we decided to come here for Prescillia’s birth as well.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Mensah Awity Teacher and ABTEF youth club coordinator in Tohoun Mensah Awity is a teacher at a local school in Tohoun. He also coordinates the ABTEF youth club where they provide information and opportunities for the students to talk about sexual health, pregnancy, contraception. “At the beginning it was difficult for the club. Now teachers have started accepting the ideas and some pupils behave much better so it’s hard for them to keep condemning it. There are three girls who gave birth and who came back to school afterwards. At the beginning it was tough for them but we explained to the students that they shouldn’t be treated differently. The rate of pregnancy has definitely gone down at school.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Emefa Charita Ankouy Youth activist and student “I'm studying for a degree in English and I'm a young activist volunteer with the IPPF youth movement. We promote, we try to help young girls who are in education to have more information about sexual health and reproduction to help them to adopt a method to avoid a pregnancy. They don't have enough information about sexual health and reproduction. I think it's because of that that they've become pregnant. They want to have sex quite early. There is pressure and there's a lack of communication between the students and their parents. Here in Togo sex is taboo for everyone, above all for parents.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Evedoh Worou Community Health Worker, Ilama “The ones who prefer the pill are young students or apprentices. Often, they take it to reduce PMS, and it regulates their period. Sometimes women will forget to take the pill, which means the injection is preferred as it’s just once for three months. The women here have more autonomy and they now have the space to earn money themselves for the household as a result of the programme. At the beginning, there were some reservations among the men in the community but after our awareness campaigns, more and more of them accompany women for family planning.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Photography by Xaume Olleros for IPPF

| 17 May 2025
In pictures: Togo and the rise in contraception use
Félicité Sonhaye ATBEF Regional Coordinator The Association Togolaise pour le Bien-Être Familial (ATBEF), has led a pioneering programme training community health workers to administer contraception in the rural areas where they live. “The injection is used more than any other method. Around 60% of women use it,” said Félicité Sonhaye, ATBEF Regional Coordinator for Togo’s Plateaux region, which covers Ilama. “Women appreciate the reliability and long-lasting effects of the injection, which allow them to stop worrying about unexpected pregnancies”, Sonhaye added. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sossou Sagna Ilama village chief Men like Sossou Sagna, have great influence and respect within Togo’s rural communities. As Ilama’s village chief his approval was required for the ATBEF community project to take root. “I sent my own wife to seek family planning. The lady helped us and it worked really well. I also went with my older brother’s wife and she was very satisfied. Every member of this community is now aware that having a large family drives them towards poverty. Ignorance was the reason why we had so many children per family here before. Now with the family planning advice we have received, spacing births has become a reality and the reduction of the number of children per family.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Abla Abassa Community health worker Abla is a community health worker, and spends her days cycling around Ilama’s dusty streets visiting households that have signed up to an innovative programme providing contraception in hard-to-reach places. “Before, people didn’t have a lot of information about contraception. With the project the community is now able to space their births. I have seen the number of children per family going down. That’s contraception but also the increasing cost of living, and the fact that everyone wants to send their children to school.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Essivi Koutchona Client Facing prohibitive costs of school fees and food prices for six children, Essivi Koutchona, began using the contraceptive injection after deciding with her husband they did not want another child. She has received the injection every three months and has not experienced any side effects. “The community health worker passed by our house one day and explained the method and a bit about the possible side effects. We agreed as a couple that we wanted me to start using the injection.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Edem Badagbo Client 33-year-old Edem is a widowed father of three children. Edem hopes to have a vasectomy within the next month or so. His wife died following the birth of their third child but he is adamant he wants to follow through with a procedure they agreed upon before her death. “My wife agreed with the idea. I was scared when I first heard of it, but that’s because there was so little information available. When I came to the ATBEF clinic I received a lot more detail and that’s when I decided to do it. I have three children. That’s enough.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Yaori Ajossou Vasectomy client Yaori Ajossou, a retired soldier, heard about vasectomy while listening to an ABTEF awareness raising campaign on the radio. It prompted him to take on the responsibility for family planning in his marriage. “Before I had the idea that maybe I'd want to have more children, but after the campaign, and after my wife had talked a little bit about her health problems, I thought, well, maybe it's better to put the brakes on. I was about to retire. Why carry on having children? Six children is already a lot. It's already maybe too many.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Dede Koussawo Client 34-year-old Dede visits the ATBEF clinic in Lomé, Togo with her husband, Edem. “We do this together if his schedule permits it. I asked and he accepted. It's not typical (for men to come). Before the pregnancy, I was taking the pill. Before the first I was taking the pill and I used an IUD after my son's birth and after my daughter's birth as well. We've been really happy with the family planning we've got here so we decided to come here for Prescillia’s birth as well.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Mensah Awity Teacher and ABTEF youth club coordinator in Tohoun Mensah Awity is a teacher at a local school in Tohoun. He also coordinates the ABTEF youth club where they provide information and opportunities for the students to talk about sexual health, pregnancy, contraception. “At the beginning it was difficult for the club. Now teachers have started accepting the ideas and some pupils behave much better so it’s hard for them to keep condemning it. There are three girls who gave birth and who came back to school afterwards. At the beginning it was tough for them but we explained to the students that they shouldn’t be treated differently. The rate of pregnancy has definitely gone down at school.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Emefa Charita Ankouy Youth activist and student “I'm studying for a degree in English and I'm a young activist volunteer with the IPPF youth movement. We promote, we try to help young girls who are in education to have more information about sexual health and reproduction to help them to adopt a method to avoid a pregnancy. They don't have enough information about sexual health and reproduction. I think it's because of that that they've become pregnant. They want to have sex quite early. There is pressure and there's a lack of communication between the students and their parents. Here in Togo sex is taboo for everyone, above all for parents.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Evedoh Worou Community Health Worker, Ilama “The ones who prefer the pill are young students or apprentices. Often, they take it to reduce PMS, and it regulates their period. Sometimes women will forget to take the pill, which means the injection is preferred as it’s just once for three months. The women here have more autonomy and they now have the space to earn money themselves for the household as a result of the programme. At the beginning, there were some reservations among the men in the community but after our awareness campaigns, more and more of them accompany women for family planning.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Photography by Xaume Olleros for IPPF

| 25 February 2019
“I want to use it for a couple of years and then maybe we will think about having another child”
Every three months, Mawoula Dahide meets a community health worker in her village in central Togo to receive a single contraceptive injection and then carries on with her busy day. Dahide, 20, has a two-and-a-half year old son and a husband living in the capital and juggles an apprenticeship in tailoring with caring for her child. After recovering from the birth, Dahide tried the injection and immediately felt relief, knowing she would decide when she got pregnant again. “I want to use it for a couple of years and then maybe we will think about having another child,” she said. Lack of access Until 2013, Dahide and the other women living in the village of Ilama had no access to regular contraception at all, and its use was sometimes regarded with suspicion, and even fear. In her community, the average age of a mother’s first pregnancy is around 16, and women might bear a total of six or seven children compared to the national average of 4.7, according to local health workers. That trend is changing with a pioneering programme run by the Association Togolaise pour le Bien-Être Familial (ATBEF), which has trained community health workers to administer contraception in the rural areas where they live. ATBEF has focused their distribution of contraceptives within poor and rural communities, and with mobile outreach clinics that go to villages with no trained health workers. The unmet need for contraception in Togo stands at 34% of the population, and in rural communities, this is even higher. The association contributes a fifth of overall contraception cover to couples in Togo, a West Africa nation of 7.8 million people. There is a clear favourite among the methods offered, which include male and female condoms, the pill, and the contraceptive injection. “The injection is more used than any other method. Around 60% of women use it,” said Félicité Sonhaye, ATBEF Regional Coordinator for Togo’s Plateaux region, which covers Ilama. Women appreciate the reliability and long-lasting effects of the injection, Sonhaye added, which allow them to stop worrying about unexpected pregnancies. From client to advocate Dahide has become an advocate for the method among her peers within her community. “My friends are getting the injection as well. I was the first to start using it and it was great, so I told them about it,” she said. Another convert to the injection is Ilama’s village chief, Sossou Sagna. The father of seven agreed with his wife they didn’t want anymore children. “I sent my own wife to seek family planning. The lady helped us and it worked really well. I also went with my older brother’s wife and she was very satisfied,” Sagna noted in the cool of the shade. “My wife chose the three-month injection,” he added. Sagna had not anticipated some of the wider effects of increasing contraceptive use within the community, which have become prevalent over the last couple of years. “Every member of this community is now aware that having a large family drives them towards poverty,” he said. Families have more money to spend feeding and educating their children in an economy where the cost of living keeps rising. Villagers who see Sagna attending family planning sessions are also convinced that rumours about contraception making them ill are untrue. “Ignorance was the reason why we had so many children per family here before. Now with the family planning advice we have received, spacing births has become a reality and the reduction of the number of children per family,” he added. The gains of the ATBEF rural programme will now go even further with the imminent introduction of Sayana Press, a contraceptive injection that women can self-administer. Learn more about some of the most popular contraception methods available and if they are right for you Photography by Xaume Olleros for IPPF

| 17 May 2025
“I want to use it for a couple of years and then maybe we will think about having another child”
Every three months, Mawoula Dahide meets a community health worker in her village in central Togo to receive a single contraceptive injection and then carries on with her busy day. Dahide, 20, has a two-and-a-half year old son and a husband living in the capital and juggles an apprenticeship in tailoring with caring for her child. After recovering from the birth, Dahide tried the injection and immediately felt relief, knowing she would decide when she got pregnant again. “I want to use it for a couple of years and then maybe we will think about having another child,” she said. Lack of access Until 2013, Dahide and the other women living in the village of Ilama had no access to regular contraception at all, and its use was sometimes regarded with suspicion, and even fear. In her community, the average age of a mother’s first pregnancy is around 16, and women might bear a total of six or seven children compared to the national average of 4.7, according to local health workers. That trend is changing with a pioneering programme run by the Association Togolaise pour le Bien-Être Familial (ATBEF), which has trained community health workers to administer contraception in the rural areas where they live. ATBEF has focused their distribution of contraceptives within poor and rural communities, and with mobile outreach clinics that go to villages with no trained health workers. The unmet need for contraception in Togo stands at 34% of the population, and in rural communities, this is even higher. The association contributes a fifth of overall contraception cover to couples in Togo, a West Africa nation of 7.8 million people. There is a clear favourite among the methods offered, which include male and female condoms, the pill, and the contraceptive injection. “The injection is more used than any other method. Around 60% of women use it,” said Félicité Sonhaye, ATBEF Regional Coordinator for Togo’s Plateaux region, which covers Ilama. Women appreciate the reliability and long-lasting effects of the injection, Sonhaye added, which allow them to stop worrying about unexpected pregnancies. From client to advocate Dahide has become an advocate for the method among her peers within her community. “My friends are getting the injection as well. I was the first to start using it and it was great, so I told them about it,” she said. Another convert to the injection is Ilama’s village chief, Sossou Sagna. The father of seven agreed with his wife they didn’t want anymore children. “I sent my own wife to seek family planning. The lady helped us and it worked really well. I also went with my older brother’s wife and she was very satisfied,” Sagna noted in the cool of the shade. “My wife chose the three-month injection,” he added. Sagna had not anticipated some of the wider effects of increasing contraceptive use within the community, which have become prevalent over the last couple of years. “Every member of this community is now aware that having a large family drives them towards poverty,” he said. Families have more money to spend feeding and educating their children in an economy where the cost of living keeps rising. Villagers who see Sagna attending family planning sessions are also convinced that rumours about contraception making them ill are untrue. “Ignorance was the reason why we had so many children per family here before. Now with the family planning advice we have received, spacing births has become a reality and the reduction of the number of children per family,” he added. The gains of the ATBEF rural programme will now go even further with the imminent introduction of Sayana Press, a contraceptive injection that women can self-administer. Learn more about some of the most popular contraception methods available and if they are right for you Photography by Xaume Olleros for IPPF

| 20 February 2019
“I wanted to work with the parents so we can stop marrying off these girls too young”
Komi Agnimavo Amazoun becomes visibly angry when he recalls the phone call telling him a 16-year-old girl was to be married off from his village in central Togo. As the highly respected village chief of Detokpo, a community of a few hundred people, Amazoun had the final say on the union, which later turned out to be the result of an attempted cover-up of a rape. Forced early marriage “I saw that she was being married off too young. The parents came to see me and I said she was not the right age,” the usually softly spoken elder said. “She didn’t yet have an education or a job” and says the girl is now 18 and has started an apprenticeship in tailoring. Such successful interventions by village chiefs in ending forced early marriage reflects the crucial importance of their involvement in sexual health strategies in the country especially in rural areas. Detakpo is one of 870 villages which have signed Village Girl Protection Charters to stop forced transactional sex in rural communities, in an initiative promoted by the Association Togolaise Pour le Bien-Être Familial (ATBEF). The charters outline prevention measures and rules in line with Togolese law to stop the rape and exploitation of underage girls, who are particularly vulnerable outside urban areas where professional advice and protection are more easily reached. Working with parents Amazoun has also received training from ATBEF on the law, which bans marriage under 18 without parental consent, and on the use of contraception to prevent underage pregnancy. “We have started to raise awareness in the village so that similar cases won’t be repeated,” Amazoun said, sitting on a plastic chair outside his home. “I wanted to work with the parents so we can stop marrying off these girls too young,” he adds. Although the official rate of marriage under 18 in Togo stands at 22%, according to UNICEF, the true rate is likely much higher, as many weddings are village ceremonies that are never registered with the authorities. “This is a very traditional place with entrenched customs. The problem of sexual violence runs very deep, which means that we have cases upon cases to deal with,” explained Dopo Kakadji, the Director for Social Action in Haho Prefecture. Kakadji oversees sexual violence cases and child protection in the area, mediating disputes over marriage and providing a link between communities and the police when necessary. The future is looking promising In many households, he said, “the woman cannot make decisions for herself. She is an object that can be used as one likes. A father can exchange a daughter to resolve problems or for money”. However, his interventions, and the creation of youth clubs to inform children of their rights, has seen families increasing willing to denounce rapists publicly. “Today girls go to school. Things have changed in the last five years, because before the priority was to marry off daughters as soon as possible,” Kakadji noted. Photography by Xaume Olleros for IPPF

| 17 May 2025
“I wanted to work with the parents so we can stop marrying off these girls too young”
Komi Agnimavo Amazoun becomes visibly angry when he recalls the phone call telling him a 16-year-old girl was to be married off from his village in central Togo. As the highly respected village chief of Detokpo, a community of a few hundred people, Amazoun had the final say on the union, which later turned out to be the result of an attempted cover-up of a rape. Forced early marriage “I saw that she was being married off too young. The parents came to see me and I said she was not the right age,” the usually softly spoken elder said. “She didn’t yet have an education or a job” and says the girl is now 18 and has started an apprenticeship in tailoring. Such successful interventions by village chiefs in ending forced early marriage reflects the crucial importance of their involvement in sexual health strategies in the country especially in rural areas. Detakpo is one of 870 villages which have signed Village Girl Protection Charters to stop forced transactional sex in rural communities, in an initiative promoted by the Association Togolaise Pour le Bien-Être Familial (ATBEF). The charters outline prevention measures and rules in line with Togolese law to stop the rape and exploitation of underage girls, who are particularly vulnerable outside urban areas where professional advice and protection are more easily reached. Working with parents Amazoun has also received training from ATBEF on the law, which bans marriage under 18 without parental consent, and on the use of contraception to prevent underage pregnancy. “We have started to raise awareness in the village so that similar cases won’t be repeated,” Amazoun said, sitting on a plastic chair outside his home. “I wanted to work with the parents so we can stop marrying off these girls too young,” he adds. Although the official rate of marriage under 18 in Togo stands at 22%, according to UNICEF, the true rate is likely much higher, as many weddings are village ceremonies that are never registered with the authorities. “This is a very traditional place with entrenched customs. The problem of sexual violence runs very deep, which means that we have cases upon cases to deal with,” explained Dopo Kakadji, the Director for Social Action in Haho Prefecture. Kakadji oversees sexual violence cases and child protection in the area, mediating disputes over marriage and providing a link between communities and the police when necessary. The future is looking promising In many households, he said, “the woman cannot make decisions for herself. She is an object that can be used as one likes. A father can exchange a daughter to resolve problems or for money”. However, his interventions, and the creation of youth clubs to inform children of their rights, has seen families increasing willing to denounce rapists publicly. “Today girls go to school. Things have changed in the last five years, because before the priority was to marry off daughters as soon as possible,” Kakadji noted. Photography by Xaume Olleros for IPPF

| 16 July 2020
"Before, there was no safe abortion"
Rewda Kedir works as a midwife in a rural area of the Oromia region in southwest Ethiopia. Only 14% of married women are using any method of contraception here. The government hospital Rewda works in is supported to provide a full range of sexual and reproductive healthcare, which includes providing free contraceptives and comprehensive abortion care. In January 2017, the maternal healthcare clinic faced shortages of contraceptives after the US administration reactivated and expanded the Global Gag Rule, which does not allow any funding to go to organizations associated with providing abortion care. Fortunately in this case, the shortages only lasted a month due to the government of the Netherlands stepping in and matching lost funding. “Before, we had a shortage of contraceptive pills and emergency contraceptives. We would have to give people prescriptions and they would go to private clinics and where they had to pay," Rewda tells us. "When I first came to this clinic, there was a real shortage of people trained in family planning. I was the only one. Now there are many people trained on family planning, and when I’m not here, people can help." "There used to be a shortage of choice and alternatives, and now there are many. And the implant procedures are better because there are newer products that are much smaller so putting them in is less invasive.” Opening a dialogue on contraception The hospital has been providing medical abortions for six years. “Before, there was no safe abortion," says Rewda. She explains how people would go to 'traditional' healers and then come to the clinic with complications like sepsis, bleeding, anaemia and toxic shock. If they had complications or infections above nine weeks, Rewda and her colleagues would send them to Jimma, the regional capital. "Before, it was very difficult to persuade them to use family planning, and we had to have a lot of conversations. Now, they come 45 days after delivery to speak to us about this and get their babies immunised," she explains. "They want contraceptives to space out their children. Sometimes their husbands don’t like them coming to get family planning so we have to lock their appointment cards away. Their husbands want more children and they think that women who do not keep having their children will go with other men." "More kids, more wealth" Rewda tells us that they've used family counselling to try and persuade men to reconsider their ideas about contraception, by explaining to them that continuously giving birth under unsafe circumstances can affect a woman's health and might lead to maternal death, damage the uterus and lead to long-term complications. "Here, people believe that more kids means more wealth, and religion restricts family planning services. Before, they did not have good training on family planning and abortion. Now, women that have abortions get proper care and the counseling and education has improved. There are still unsafe abortions but they have really reduced. We used to see about 40 a year and now it’s one or two." However, problems still exist. "There are some complications, like irregular bleeding from some contraceptives," Rewda says, and that "women still face conflict with their husbands over family planning and sometimes have to go to court to fight this or divorce them.”

| 17 May 2025
"Before, there was no safe abortion"
Rewda Kedir works as a midwife in a rural area of the Oromia region in southwest Ethiopia. Only 14% of married women are using any method of contraception here. The government hospital Rewda works in is supported to provide a full range of sexual and reproductive healthcare, which includes providing free contraceptives and comprehensive abortion care. In January 2017, the maternal healthcare clinic faced shortages of contraceptives after the US administration reactivated and expanded the Global Gag Rule, which does not allow any funding to go to organizations associated with providing abortion care. Fortunately in this case, the shortages only lasted a month due to the government of the Netherlands stepping in and matching lost funding. “Before, we had a shortage of contraceptive pills and emergency contraceptives. We would have to give people prescriptions and they would go to private clinics and where they had to pay," Rewda tells us. "When I first came to this clinic, there was a real shortage of people trained in family planning. I was the only one. Now there are many people trained on family planning, and when I’m not here, people can help." "There used to be a shortage of choice and alternatives, and now there are many. And the implant procedures are better because there are newer products that are much smaller so putting them in is less invasive.” Opening a dialogue on contraception The hospital has been providing medical abortions for six years. “Before, there was no safe abortion," says Rewda. She explains how people would go to 'traditional' healers and then come to the clinic with complications like sepsis, bleeding, anaemia and toxic shock. If they had complications or infections above nine weeks, Rewda and her colleagues would send them to Jimma, the regional capital. "Before, it was very difficult to persuade them to use family planning, and we had to have a lot of conversations. Now, they come 45 days after delivery to speak to us about this and get their babies immunised," she explains. "They want contraceptives to space out their children. Sometimes their husbands don’t like them coming to get family planning so we have to lock their appointment cards away. Their husbands want more children and they think that women who do not keep having their children will go with other men." "More kids, more wealth" Rewda tells us that they've used family counselling to try and persuade men to reconsider their ideas about contraception, by explaining to them that continuously giving birth under unsafe circumstances can affect a woman's health and might lead to maternal death, damage the uterus and lead to long-term complications. "Here, people believe that more kids means more wealth, and religion restricts family planning services. Before, they did not have good training on family planning and abortion. Now, women that have abortions get proper care and the counseling and education has improved. There are still unsafe abortions but they have really reduced. We used to see about 40 a year and now it’s one or two." However, problems still exist. "There are some complications, like irregular bleeding from some contraceptives," Rewda says, and that "women still face conflict with their husbands over family planning and sometimes have to go to court to fight this or divorce them.”

| 01 July 2020
In pictures: Ensuring confidentiality, safety, and care for sex workers
Meseret* and Melat*, volunteers Known in their local community as demand creators, Meseret and Melat, from the Family Guidance Association of Ethiopia’s (FGAE) confidential clinic head out to visit sex workers in Jimma town. This group of volunteers are former, or current, sex workers teaching others how to protect themselves from sexually transmitted infections (STIs) and unintended pregnancy. Their work is challenging, and they travel in pairs for safety - their messages are not always welcome. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Meseret* and Melat*, volunteers Meseret and Melat from the Jimma clinic talk to sex workers in their local community about sexual health concerns, as well as provide contraception. “It’s very difficult to convince sex workers to come to the clinic. Some sex workers tend to have no knowledge, even about how to use a condom.” says Meseret. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Melat, volunteer It can be challenging persuading women that the staff at the confidential clinic are friendly towards sex workers and will keep their information private. “When we try to tell people about HIV we can be insulted and told: ‘You are just working for yourself and earn money if you bring us in.’ They sometimes throw stones and sticks at us,” said 25-year-old Melat. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Fantaye, sex worker Getting information and contraception to women often involves going out to find them, such as Fantaye, a sex worker currently living in a rental space in Mekelle. Peer educators focus on areas populated with hotels and bars and broker's houses, where sex workers find clients. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sister Mahader, FGAE Sister Mahader from FGAEs' youth centre talks to sex workers in Mekelle, about sexual health, wellbeing, and various methods of contraception. This outreach takes place weekly where information and advice is given to groups of women, and contraception is provided free of charge. Under threat from the loss of funding from the US Administration, the Jimma clinic has been forced to reduce the range of commodities available to its clients such as sanitary products, soap and water purification tablets. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Hiwot Abera*, sex worker Hiwot* after her appointment at FGAEs confidential clinic in Jimma. The clinic offers free and bespoke healthcare including HIV and STI testing, treatment and counselling, contraceptives and safe abortion care. Many sex workers have experienced stigma and discrimination at other clinics. In contrast, ensuring confidentiality and a safe environment for the women to talk openly is at the heart of FGAEs’ healthcare provision at its clinics.*pseudonymPhotos: ©IPPF/Zacharias Abubeker Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 17 May 2025
In pictures: Ensuring confidentiality, safety, and care for sex workers
Meseret* and Melat*, volunteers Known in their local community as demand creators, Meseret and Melat, from the Family Guidance Association of Ethiopia’s (FGAE) confidential clinic head out to visit sex workers in Jimma town. This group of volunteers are former, or current, sex workers teaching others how to protect themselves from sexually transmitted infections (STIs) and unintended pregnancy. Their work is challenging, and they travel in pairs for safety - their messages are not always welcome. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Meseret* and Melat*, volunteers Meseret and Melat from the Jimma clinic talk to sex workers in their local community about sexual health concerns, as well as provide contraception. “It’s very difficult to convince sex workers to come to the clinic. Some sex workers tend to have no knowledge, even about how to use a condom.” says Meseret. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Melat, volunteer It can be challenging persuading women that the staff at the confidential clinic are friendly towards sex workers and will keep their information private. “When we try to tell people about HIV we can be insulted and told: ‘You are just working for yourself and earn money if you bring us in.’ They sometimes throw stones and sticks at us,” said 25-year-old Melat. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Fantaye, sex worker Getting information and contraception to women often involves going out to find them, such as Fantaye, a sex worker currently living in a rental space in Mekelle. Peer educators focus on areas populated with hotels and bars and broker's houses, where sex workers find clients. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sister Mahader, FGAE Sister Mahader from FGAEs' youth centre talks to sex workers in Mekelle, about sexual health, wellbeing, and various methods of contraception. This outreach takes place weekly where information and advice is given to groups of women, and contraception is provided free of charge. Under threat from the loss of funding from the US Administration, the Jimma clinic has been forced to reduce the range of commodities available to its clients such as sanitary products, soap and water purification tablets. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Hiwot Abera*, sex worker Hiwot* after her appointment at FGAEs confidential clinic in Jimma. The clinic offers free and bespoke healthcare including HIV and STI testing, treatment and counselling, contraceptives and safe abortion care. Many sex workers have experienced stigma and discrimination at other clinics. In contrast, ensuring confidentiality and a safe environment for the women to talk openly is at the heart of FGAEs’ healthcare provision at its clinics.*pseudonymPhotos: ©IPPF/Zacharias Abubeker Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 25 February 2019
In pictures: Togo and the rise in contraception use
Félicité Sonhaye ATBEF Regional Coordinator The Association Togolaise pour le Bien-Être Familial (ATBEF), has led a pioneering programme training community health workers to administer contraception in the rural areas where they live. “The injection is used more than any other method. Around 60% of women use it,” said Félicité Sonhaye, ATBEF Regional Coordinator for Togo’s Plateaux region, which covers Ilama. “Women appreciate the reliability and long-lasting effects of the injection, which allow them to stop worrying about unexpected pregnancies”, Sonhaye added. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sossou Sagna Ilama village chief Men like Sossou Sagna, have great influence and respect within Togo’s rural communities. As Ilama’s village chief his approval was required for the ATBEF community project to take root. “I sent my own wife to seek family planning. The lady helped us and it worked really well. I also went with my older brother’s wife and she was very satisfied. Every member of this community is now aware that having a large family drives them towards poverty. Ignorance was the reason why we had so many children per family here before. Now with the family planning advice we have received, spacing births has become a reality and the reduction of the number of children per family.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Abla Abassa Community health worker Abla is a community health worker, and spends her days cycling around Ilama’s dusty streets visiting households that have signed up to an innovative programme providing contraception in hard-to-reach places. “Before, people didn’t have a lot of information about contraception. With the project the community is now able to space their births. I have seen the number of children per family going down. That’s contraception but also the increasing cost of living, and the fact that everyone wants to send their children to school.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Essivi Koutchona Client Facing prohibitive costs of school fees and food prices for six children, Essivi Koutchona, began using the contraceptive injection after deciding with her husband they did not want another child. She has received the injection every three months and has not experienced any side effects. “The community health worker passed by our house one day and explained the method and a bit about the possible side effects. We agreed as a couple that we wanted me to start using the injection.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Edem Badagbo Client 33-year-old Edem is a widowed father of three children. Edem hopes to have a vasectomy within the next month or so. His wife died following the birth of their third child but he is adamant he wants to follow through with a procedure they agreed upon before her death. “My wife agreed with the idea. I was scared when I first heard of it, but that’s because there was so little information available. When I came to the ATBEF clinic I received a lot more detail and that’s when I decided to do it. I have three children. That’s enough.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Yaori Ajossou Vasectomy client Yaori Ajossou, a retired soldier, heard about vasectomy while listening to an ABTEF awareness raising campaign on the radio. It prompted him to take on the responsibility for family planning in his marriage. “Before I had the idea that maybe I'd want to have more children, but after the campaign, and after my wife had talked a little bit about her health problems, I thought, well, maybe it's better to put the brakes on. I was about to retire. Why carry on having children? Six children is already a lot. It's already maybe too many.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Dede Koussawo Client 34-year-old Dede visits the ATBEF clinic in Lomé, Togo with her husband, Edem. “We do this together if his schedule permits it. I asked and he accepted. It's not typical (for men to come). Before the pregnancy, I was taking the pill. Before the first I was taking the pill and I used an IUD after my son's birth and after my daughter's birth as well. We've been really happy with the family planning we've got here so we decided to come here for Prescillia’s birth as well.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Mensah Awity Teacher and ABTEF youth club coordinator in Tohoun Mensah Awity is a teacher at a local school in Tohoun. He also coordinates the ABTEF youth club where they provide information and opportunities for the students to talk about sexual health, pregnancy, contraception. “At the beginning it was difficult for the club. Now teachers have started accepting the ideas and some pupils behave much better so it’s hard for them to keep condemning it. There are three girls who gave birth and who came back to school afterwards. At the beginning it was tough for them but we explained to the students that they shouldn’t be treated differently. The rate of pregnancy has definitely gone down at school.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Emefa Charita Ankouy Youth activist and student “I'm studying for a degree in English and I'm a young activist volunteer with the IPPF youth movement. We promote, we try to help young girls who are in education to have more information about sexual health and reproduction to help them to adopt a method to avoid a pregnancy. They don't have enough information about sexual health and reproduction. I think it's because of that that they've become pregnant. They want to have sex quite early. There is pressure and there's a lack of communication between the students and their parents. Here in Togo sex is taboo for everyone, above all for parents.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Evedoh Worou Community Health Worker, Ilama “The ones who prefer the pill are young students or apprentices. Often, they take it to reduce PMS, and it regulates their period. Sometimes women will forget to take the pill, which means the injection is preferred as it’s just once for three months. The women here have more autonomy and they now have the space to earn money themselves for the household as a result of the programme. At the beginning, there were some reservations among the men in the community but after our awareness campaigns, more and more of them accompany women for family planning.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Photography by Xaume Olleros for IPPF

| 17 May 2025
In pictures: Togo and the rise in contraception use
Félicité Sonhaye ATBEF Regional Coordinator The Association Togolaise pour le Bien-Être Familial (ATBEF), has led a pioneering programme training community health workers to administer contraception in the rural areas where they live. “The injection is used more than any other method. Around 60% of women use it,” said Félicité Sonhaye, ATBEF Regional Coordinator for Togo’s Plateaux region, which covers Ilama. “Women appreciate the reliability and long-lasting effects of the injection, which allow them to stop worrying about unexpected pregnancies”, Sonhaye added. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Sossou Sagna Ilama village chief Men like Sossou Sagna, have great influence and respect within Togo’s rural communities. As Ilama’s village chief his approval was required for the ATBEF community project to take root. “I sent my own wife to seek family planning. The lady helped us and it worked really well. I also went with my older brother’s wife and she was very satisfied. Every member of this community is now aware that having a large family drives them towards poverty. Ignorance was the reason why we had so many children per family here before. Now with the family planning advice we have received, spacing births has become a reality and the reduction of the number of children per family.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Abla Abassa Community health worker Abla is a community health worker, and spends her days cycling around Ilama’s dusty streets visiting households that have signed up to an innovative programme providing contraception in hard-to-reach places. “Before, people didn’t have a lot of information about contraception. With the project the community is now able to space their births. I have seen the number of children per family going down. That’s contraception but also the increasing cost of living, and the fact that everyone wants to send their children to school.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Essivi Koutchona Client Facing prohibitive costs of school fees and food prices for six children, Essivi Koutchona, began using the contraceptive injection after deciding with her husband they did not want another child. She has received the injection every three months and has not experienced any side effects. “The community health worker passed by our house one day and explained the method and a bit about the possible side effects. We agreed as a couple that we wanted me to start using the injection.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Edem Badagbo Client 33-year-old Edem is a widowed father of three children. Edem hopes to have a vasectomy within the next month or so. His wife died following the birth of their third child but he is adamant he wants to follow through with a procedure they agreed upon before her death. “My wife agreed with the idea. I was scared when I first heard of it, but that’s because there was so little information available. When I came to the ATBEF clinic I received a lot more detail and that’s when I decided to do it. I have three children. That’s enough.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Yaori Ajossou Vasectomy client Yaori Ajossou, a retired soldier, heard about vasectomy while listening to an ABTEF awareness raising campaign on the radio. It prompted him to take on the responsibility for family planning in his marriage. “Before I had the idea that maybe I'd want to have more children, but after the campaign, and after my wife had talked a little bit about her health problems, I thought, well, maybe it's better to put the brakes on. I was about to retire. Why carry on having children? Six children is already a lot. It's already maybe too many.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Dede Koussawo Client 34-year-old Dede visits the ATBEF clinic in Lomé, Togo with her husband, Edem. “We do this together if his schedule permits it. I asked and he accepted. It's not typical (for men to come). Before the pregnancy, I was taking the pill. Before the first I was taking the pill and I used an IUD after my son's birth and after my daughter's birth as well. We've been really happy with the family planning we've got here so we decided to come here for Prescillia’s birth as well.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Mensah Awity Teacher and ABTEF youth club coordinator in Tohoun Mensah Awity is a teacher at a local school in Tohoun. He also coordinates the ABTEF youth club where they provide information and opportunities for the students to talk about sexual health, pregnancy, contraception. “At the beginning it was difficult for the club. Now teachers have started accepting the ideas and some pupils behave much better so it’s hard for them to keep condemning it. There are three girls who gave birth and who came back to school afterwards. At the beginning it was tough for them but we explained to the students that they shouldn’t be treated differently. The rate of pregnancy has definitely gone down at school.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Emefa Charita Ankouy Youth activist and student “I'm studying for a degree in English and I'm a young activist volunteer with the IPPF youth movement. We promote, we try to help young girls who are in education to have more information about sexual health and reproduction to help them to adopt a method to avoid a pregnancy. They don't have enough information about sexual health and reproduction. I think it's because of that that they've become pregnant. They want to have sex quite early. There is pressure and there's a lack of communication between the students and their parents. Here in Togo sex is taboo for everyone, above all for parents.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Evedoh Worou Community Health Worker, Ilama “The ones who prefer the pill are young students or apprentices. Often, they take it to reduce PMS, and it regulates their period. Sometimes women will forget to take the pill, which means the injection is preferred as it’s just once for three months. The women here have more autonomy and they now have the space to earn money themselves for the household as a result of the programme. At the beginning, there were some reservations among the men in the community but after our awareness campaigns, more and more of them accompany women for family planning.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Photography by Xaume Olleros for IPPF

| 25 February 2019
“I want to use it for a couple of years and then maybe we will think about having another child”
Every three months, Mawoula Dahide meets a community health worker in her village in central Togo to receive a single contraceptive injection and then carries on with her busy day. Dahide, 20, has a two-and-a-half year old son and a husband living in the capital and juggles an apprenticeship in tailoring with caring for her child. After recovering from the birth, Dahide tried the injection and immediately felt relief, knowing she would decide when she got pregnant again. “I want to use it for a couple of years and then maybe we will think about having another child,” she said. Lack of access Until 2013, Dahide and the other women living in the village of Ilama had no access to regular contraception at all, and its use was sometimes regarded with suspicion, and even fear. In her community, the average age of a mother’s first pregnancy is around 16, and women might bear a total of six or seven children compared to the national average of 4.7, according to local health workers. That trend is changing with a pioneering programme run by the Association Togolaise pour le Bien-Être Familial (ATBEF), which has trained community health workers to administer contraception in the rural areas where they live. ATBEF has focused their distribution of contraceptives within poor and rural communities, and with mobile outreach clinics that go to villages with no trained health workers. The unmet need for contraception in Togo stands at 34% of the population, and in rural communities, this is even higher. The association contributes a fifth of overall contraception cover to couples in Togo, a West Africa nation of 7.8 million people. There is a clear favourite among the methods offered, which include male and female condoms, the pill, and the contraceptive injection. “The injection is more used than any other method. Around 60% of women use it,” said Félicité Sonhaye, ATBEF Regional Coordinator for Togo’s Plateaux region, which covers Ilama. Women appreciate the reliability and long-lasting effects of the injection, Sonhaye added, which allow them to stop worrying about unexpected pregnancies. From client to advocate Dahide has become an advocate for the method among her peers within her community. “My friends are getting the injection as well. I was the first to start using it and it was great, so I told them about it,” she said. Another convert to the injection is Ilama’s village chief, Sossou Sagna. The father of seven agreed with his wife they didn’t want anymore children. “I sent my own wife to seek family planning. The lady helped us and it worked really well. I also went with my older brother’s wife and she was very satisfied,” Sagna noted in the cool of the shade. “My wife chose the three-month injection,” he added. Sagna had not anticipated some of the wider effects of increasing contraceptive use within the community, which have become prevalent over the last couple of years. “Every member of this community is now aware that having a large family drives them towards poverty,” he said. Families have more money to spend feeding and educating their children in an economy where the cost of living keeps rising. Villagers who see Sagna attending family planning sessions are also convinced that rumours about contraception making them ill are untrue. “Ignorance was the reason why we had so many children per family here before. Now with the family planning advice we have received, spacing births has become a reality and the reduction of the number of children per family,” he added. The gains of the ATBEF rural programme will now go even further with the imminent introduction of Sayana Press, a contraceptive injection that women can self-administer. Learn more about some of the most popular contraception methods available and if they are right for you Photography by Xaume Olleros for IPPF

| 17 May 2025
“I want to use it for a couple of years and then maybe we will think about having another child”
Every three months, Mawoula Dahide meets a community health worker in her village in central Togo to receive a single contraceptive injection and then carries on with her busy day. Dahide, 20, has a two-and-a-half year old son and a husband living in the capital and juggles an apprenticeship in tailoring with caring for her child. After recovering from the birth, Dahide tried the injection and immediately felt relief, knowing she would decide when she got pregnant again. “I want to use it for a couple of years and then maybe we will think about having another child,” she said. Lack of access Until 2013, Dahide and the other women living in the village of Ilama had no access to regular contraception at all, and its use was sometimes regarded with suspicion, and even fear. In her community, the average age of a mother’s first pregnancy is around 16, and women might bear a total of six or seven children compared to the national average of 4.7, according to local health workers. That trend is changing with a pioneering programme run by the Association Togolaise pour le Bien-Être Familial (ATBEF), which has trained community health workers to administer contraception in the rural areas where they live. ATBEF has focused their distribution of contraceptives within poor and rural communities, and with mobile outreach clinics that go to villages with no trained health workers. The unmet need for contraception in Togo stands at 34% of the population, and in rural communities, this is even higher. The association contributes a fifth of overall contraception cover to couples in Togo, a West Africa nation of 7.8 million people. There is a clear favourite among the methods offered, which include male and female condoms, the pill, and the contraceptive injection. “The injection is more used than any other method. Around 60% of women use it,” said Félicité Sonhaye, ATBEF Regional Coordinator for Togo’s Plateaux region, which covers Ilama. Women appreciate the reliability and long-lasting effects of the injection, Sonhaye added, which allow them to stop worrying about unexpected pregnancies. From client to advocate Dahide has become an advocate for the method among her peers within her community. “My friends are getting the injection as well. I was the first to start using it and it was great, so I told them about it,” she said. Another convert to the injection is Ilama’s village chief, Sossou Sagna. The father of seven agreed with his wife they didn’t want anymore children. “I sent my own wife to seek family planning. The lady helped us and it worked really well. I also went with my older brother’s wife and she was very satisfied,” Sagna noted in the cool of the shade. “My wife chose the three-month injection,” he added. Sagna had not anticipated some of the wider effects of increasing contraceptive use within the community, which have become prevalent over the last couple of years. “Every member of this community is now aware that having a large family drives them towards poverty,” he said. Families have more money to spend feeding and educating their children in an economy where the cost of living keeps rising. Villagers who see Sagna attending family planning sessions are also convinced that rumours about contraception making them ill are untrue. “Ignorance was the reason why we had so many children per family here before. Now with the family planning advice we have received, spacing births has become a reality and the reduction of the number of children per family,” he added. The gains of the ATBEF rural programme will now go even further with the imminent introduction of Sayana Press, a contraceptive injection that women can self-administer. Learn more about some of the most popular contraception methods available and if they are right for you Photography by Xaume Olleros for IPPF

| 20 February 2019
“I wanted to work with the parents so we can stop marrying off these girls too young”
Komi Agnimavo Amazoun becomes visibly angry when he recalls the phone call telling him a 16-year-old girl was to be married off from his village in central Togo. As the highly respected village chief of Detokpo, a community of a few hundred people, Amazoun had the final say on the union, which later turned out to be the result of an attempted cover-up of a rape. Forced early marriage “I saw that she was being married off too young. The parents came to see me and I said she was not the right age,” the usually softly spoken elder said. “She didn’t yet have an education or a job” and says the girl is now 18 and has started an apprenticeship in tailoring. Such successful interventions by village chiefs in ending forced early marriage reflects the crucial importance of their involvement in sexual health strategies in the country especially in rural areas. Detakpo is one of 870 villages which have signed Village Girl Protection Charters to stop forced transactional sex in rural communities, in an initiative promoted by the Association Togolaise Pour le Bien-Être Familial (ATBEF). The charters outline prevention measures and rules in line with Togolese law to stop the rape and exploitation of underage girls, who are particularly vulnerable outside urban areas where professional advice and protection are more easily reached. Working with parents Amazoun has also received training from ATBEF on the law, which bans marriage under 18 without parental consent, and on the use of contraception to prevent underage pregnancy. “We have started to raise awareness in the village so that similar cases won’t be repeated,” Amazoun said, sitting on a plastic chair outside his home. “I wanted to work with the parents so we can stop marrying off these girls too young,” he adds. Although the official rate of marriage under 18 in Togo stands at 22%, according to UNICEF, the true rate is likely much higher, as many weddings are village ceremonies that are never registered with the authorities. “This is a very traditional place with entrenched customs. The problem of sexual violence runs very deep, which means that we have cases upon cases to deal with,” explained Dopo Kakadji, the Director for Social Action in Haho Prefecture. Kakadji oversees sexual violence cases and child protection in the area, mediating disputes over marriage and providing a link between communities and the police when necessary. The future is looking promising In many households, he said, “the woman cannot make decisions for herself. She is an object that can be used as one likes. A father can exchange a daughter to resolve problems or for money”. However, his interventions, and the creation of youth clubs to inform children of their rights, has seen families increasing willing to denounce rapists publicly. “Today girls go to school. Things have changed in the last five years, because before the priority was to marry off daughters as soon as possible,” Kakadji noted. Photography by Xaume Olleros for IPPF

| 17 May 2025
“I wanted to work with the parents so we can stop marrying off these girls too young”
Komi Agnimavo Amazoun becomes visibly angry when he recalls the phone call telling him a 16-year-old girl was to be married off from his village in central Togo. As the highly respected village chief of Detokpo, a community of a few hundred people, Amazoun had the final say on the union, which later turned out to be the result of an attempted cover-up of a rape. Forced early marriage “I saw that she was being married off too young. The parents came to see me and I said she was not the right age,” the usually softly spoken elder said. “She didn’t yet have an education or a job” and says the girl is now 18 and has started an apprenticeship in tailoring. Such successful interventions by village chiefs in ending forced early marriage reflects the crucial importance of their involvement in sexual health strategies in the country especially in rural areas. Detakpo is one of 870 villages which have signed Village Girl Protection Charters to stop forced transactional sex in rural communities, in an initiative promoted by the Association Togolaise Pour le Bien-Être Familial (ATBEF). The charters outline prevention measures and rules in line with Togolese law to stop the rape and exploitation of underage girls, who are particularly vulnerable outside urban areas where professional advice and protection are more easily reached. Working with parents Amazoun has also received training from ATBEF on the law, which bans marriage under 18 without parental consent, and on the use of contraception to prevent underage pregnancy. “We have started to raise awareness in the village so that similar cases won’t be repeated,” Amazoun said, sitting on a plastic chair outside his home. “I wanted to work with the parents so we can stop marrying off these girls too young,” he adds. Although the official rate of marriage under 18 in Togo stands at 22%, according to UNICEF, the true rate is likely much higher, as many weddings are village ceremonies that are never registered with the authorities. “This is a very traditional place with entrenched customs. The problem of sexual violence runs very deep, which means that we have cases upon cases to deal with,” explained Dopo Kakadji, the Director for Social Action in Haho Prefecture. Kakadji oversees sexual violence cases and child protection in the area, mediating disputes over marriage and providing a link between communities and the police when necessary. The future is looking promising In many households, he said, “the woman cannot make decisions for herself. She is an object that can be used as one likes. A father can exchange a daughter to resolve problems or for money”. However, his interventions, and the creation of youth clubs to inform children of their rights, has seen families increasing willing to denounce rapists publicly. “Today girls go to school. Things have changed in the last five years, because before the priority was to marry off daughters as soon as possible,” Kakadji noted. Photography by Xaume Olleros for IPPF