Spotlight
A selection of stories from across the Federation

Advances in Sexual and Reproductive Rights and Health: 2024 in Review
Let’s take a leap back in time to the beginning of 2024: In twelve months, what victories has our movement managed to secure in the face of growing opposition and the rise of the far right? These victories for sexual and reproductive rights and health are the result of relentless grassroots work and advocacy by our Member Associations, in partnership with community organizations, allied politicians, and the mobilization of public opinion.
Most Popular This Week

Advances in Sexual and Reproductive Rights and Health: 2024 in Review
Let’s take a leap back in time to the beginning of 2024: In twelve months, what victories has our movement managed to secure in t
Kazakhstan

Kazakhstan's Rising HIV Crisis: A Call for Action
On World AIDS Day, we commemorate the remarkable achievements of IPPF Member Associations in their unwavering commitment to combating the HIV epidemic.

Ensuring SRHR in Humanitarian Crises: What You Need to Know
Over the past two decades, global forced displacement has consistently increased, affecting an estimated 114 million people as of mid-2023.
Estonia, Nepal, Namibia, Japan, Thailand

The Rainbow Wave for Marriage Equality
Love wins! The fight for marriage equality has seen incredible progress worldwide, with a recent surge in legalizations.
France, Germany, Poland, United Kingdom, United States, Colombia, India, Tunisia

Abortion Rights: Latest Decisions and Developments around the World
Over the past 30 years, more than

Palestine

In their own words: The people providing sexual and reproductive health care under bombardment in Gaza
Week after week, heavy Israeli bombardment from air, land, and sea, has continued across most of the Gaza Strip.
Vanuatu

When getting to the hospital is difficult, Vanuatu mobile outreach can save lives
In the mountains of Kumera on Tanna Island, Vanuatu, the village women of Kamahaul normally spend over 10,000 Vatu ($83 USD) to travel to the nearest hospital.
Filter our stories by:
- Afghanistan
- Albania
- Aruba
- Bangladesh
- Benin
- Botswana
- Burundi
- Cambodia
- Cameroon
- Colombia
- Congo, Dem. Rep.
- Cook Islands
- El Salvador
- Estonia
- Ethiopia
- (-) Fiji
- France
- Germany
- Ghana
- Guinea-Conakry
- India
- Ireland
- Jamaica
- Japan
- Kazakhstan
- Kenya
- Kiribati
- Lesotho
- Malawi
- Mali
- Mozambique
- Namibia
- Nepal
- Nigeria
- Pakistan
- Palestine
- Poland
- Senegal
- Somaliland
- Sri Lanka
- Sudan
- Thailand
- Togo
- Tonga
- Trinidad and Tobago
- Tunisia
- (-) Uganda
- United Kingdom
- United States
- Vanuatu
- Zambia


| 05 January 2022
In pictures: The changemaker keeping her community healthy and happy
The Get Up, Speak Out! initiative works with and for young people to overcome barriers such as unequal gender norms, negative attitudes towards sexuality, taboos about sex, menstruation, and abortion. Empowering youth communities - especially girls and young women - with information and knowledge about sexual and reproductive health, and the provision of access to health and contraceptive care, is at the heart of the initiative. Get Up, Speak Out! is an international initiative developed by a consortium of partners including IPPF, Rutgers, CHOICE for Youth & Sexuality, Dance4Life, Simavi, and Aidsfonds, with support from the Dutch Ministry of Foreign Affairs.

| 15 May 2025
In pictures: The changemaker keeping her community healthy and happy
The Get Up, Speak Out! initiative works with and for young people to overcome barriers such as unequal gender norms, negative attitudes towards sexuality, taboos about sex, menstruation, and abortion. Empowering youth communities - especially girls and young women - with information and knowledge about sexual and reproductive health, and the provision of access to health and contraceptive care, is at the heart of the initiative. Get Up, Speak Out! is an international initiative developed by a consortium of partners including IPPF, Rutgers, CHOICE for Youth & Sexuality, Dance4Life, Simavi, and Aidsfonds, with support from the Dutch Ministry of Foreign Affairs.

| 03 March 2021
The response to Tropical Cyclone Yasa: Through the eyes of a humanitarian surge member
Sera Vulavou is the Senior Monitoring and Evaluation Officer with IPPF’s Sub-Regional Office for the Pacific. She was trained as a humanitarian surge roster member in early 2020, to be able to deploy to emergencies to provide technical assistance to Member Associations – here she shares her experience with us. Severe Tropical Cyclone (TC) Yasa was the strongest in the South Pacific since TC Winston in 2016, as well as the fourth most intense TC on record in the basin. The Reproductive and Family Health Association of Fiji (RFHAF) humanitarian response to TC Yasa has reached some of the most difficult and geographically scattered islands and communities, which included the islands of Moala, Totoya, and Matuku. Being part of the IPPF humanitarian surge roster team gave me the opportunity to accompany the RFHAF response team during their humanitarian work. This experience was about putting in action what I could only personally describe as being at the right place at the right time.

| 15 May 2025
The response to Tropical Cyclone Yasa: Through the eyes of a humanitarian surge member
Sera Vulavou is the Senior Monitoring and Evaluation Officer with IPPF’s Sub-Regional Office for the Pacific. She was trained as a humanitarian surge roster member in early 2020, to be able to deploy to emergencies to provide technical assistance to Member Associations – here she shares her experience with us. Severe Tropical Cyclone (TC) Yasa was the strongest in the South Pacific since TC Winston in 2016, as well as the fourth most intense TC on record in the basin. The Reproductive and Family Health Association of Fiji (RFHAF) humanitarian response to TC Yasa has reached some of the most difficult and geographically scattered islands and communities, which included the islands of Moala, Totoya, and Matuku. Being part of the IPPF humanitarian surge roster team gave me the opportunity to accompany the RFHAF response team during their humanitarian work. This experience was about putting in action what I could only personally describe as being at the right place at the right time.

| 13 August 2020
In pictures: Delivering healthcare to remote communities in Fiji
In early April 2020, the all too familiar destruction of a Tropical Cyclone (TC) – Harold – hit the Solomon Islands, Vanuatu, Fiji and Tonga. One of the worst affected areas was the Eastern part of Fiji. Through support by Department of Foreign Affairs and Trade (DFAT), our Member Association, Reproductive and Family Health Association of Fiji (RFHAF), was quick to respond ensuring access to essential sexual and reproductive healthcare for Kadavu’s women, girls, and vulnerable groups. Fiji's vulnerable coastline Fiji’s worst affected area was the Eastern part, with TC Harold bringing destructive storm force winds and storm surge. RFHAF focused its humanitarian response on the local Kadavu population. This remote area proves a challenge to reach for the team with supplies. Share on Twitter Share on Facebook Share via WhatsApp Share via Email RFHAF's humanitarian response team tackle rough terrain National travel restrictions - due to the current COVID-19 pandemic - on all inter island transfers has slowed the response in some areas, including Kadavu. The island of Kadavu is one of the least developed areas of Fiji, the main source of income is substance living (Yaqona). Transport around the island is difficult, with very few roads, no public water system or electricity. The humanitarian team from RFHAF travels by boat and then on foot. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Asenaca, client Kadavu, the biggest island in the Eastern division has the greatest population (10,897). 197 evacuation centres were activated in total, initially hosting over 6,240 people. Many are women of reproductive age, with an estimated 150 currently pregnant. Asenaca learns about breast cancer self-checks from RFHAF’s healthcare provider, Karo. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nasi, RFHAF healthcare provider The medical mobile team deliver a broad range of healthcare including contraception, information and counselling on sexual health, pregnancy, HIV and STI care and testing. RFHAF Team in Kadavu performing general health checks after TC Harold. Nasi administers a HPV shot to a client. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Kate, client Young women and girls are at the heart of RFHAF’s healthcare provision. Kate walks home with her dignity kit after a health check at the mobile clinic. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Karo, RFHAF healthcare worker RFHAF offers sexual and reproductive healthcare as well as counselling, and referrals for follow up care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Alidi, RFHAF healthcare worker The team ensures young people in the community are not forgotten and provide information and education on relationships and sexual health and rights. Alidi conducting a session with a local group of young people at Gasele, Kadavu.Photos ©IPPF/Rob Rickman/Fiji Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 15 May 2025
In pictures: Delivering healthcare to remote communities in Fiji
In early April 2020, the all too familiar destruction of a Tropical Cyclone (TC) – Harold – hit the Solomon Islands, Vanuatu, Fiji and Tonga. One of the worst affected areas was the Eastern part of Fiji. Through support by Department of Foreign Affairs and Trade (DFAT), our Member Association, Reproductive and Family Health Association of Fiji (RFHAF), was quick to respond ensuring access to essential sexual and reproductive healthcare for Kadavu’s women, girls, and vulnerable groups. Fiji's vulnerable coastline Fiji’s worst affected area was the Eastern part, with TC Harold bringing destructive storm force winds and storm surge. RFHAF focused its humanitarian response on the local Kadavu population. This remote area proves a challenge to reach for the team with supplies. Share on Twitter Share on Facebook Share via WhatsApp Share via Email RFHAF's humanitarian response team tackle rough terrain National travel restrictions - due to the current COVID-19 pandemic - on all inter island transfers has slowed the response in some areas, including Kadavu. The island of Kadavu is one of the least developed areas of Fiji, the main source of income is substance living (Yaqona). Transport around the island is difficult, with very few roads, no public water system or electricity. The humanitarian team from RFHAF travels by boat and then on foot. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Asenaca, client Kadavu, the biggest island in the Eastern division has the greatest population (10,897). 197 evacuation centres were activated in total, initially hosting over 6,240 people. Many are women of reproductive age, with an estimated 150 currently pregnant. Asenaca learns about breast cancer self-checks from RFHAF’s healthcare provider, Karo. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nasi, RFHAF healthcare provider The medical mobile team deliver a broad range of healthcare including contraception, information and counselling on sexual health, pregnancy, HIV and STI care and testing. RFHAF Team in Kadavu performing general health checks after TC Harold. Nasi administers a HPV shot to a client. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Kate, client Young women and girls are at the heart of RFHAF’s healthcare provision. Kate walks home with her dignity kit after a health check at the mobile clinic. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Karo, RFHAF healthcare worker RFHAF offers sexual and reproductive healthcare as well as counselling, and referrals for follow up care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Alidi, RFHAF healthcare worker The team ensures young people in the community are not forgotten and provide information and education on relationships and sexual health and rights. Alidi conducting a session with a local group of young people at Gasele, Kadavu.Photos ©IPPF/Rob Rickman/Fiji Share on Twitter Share on Facebook Share via WhatsApp Share via Email
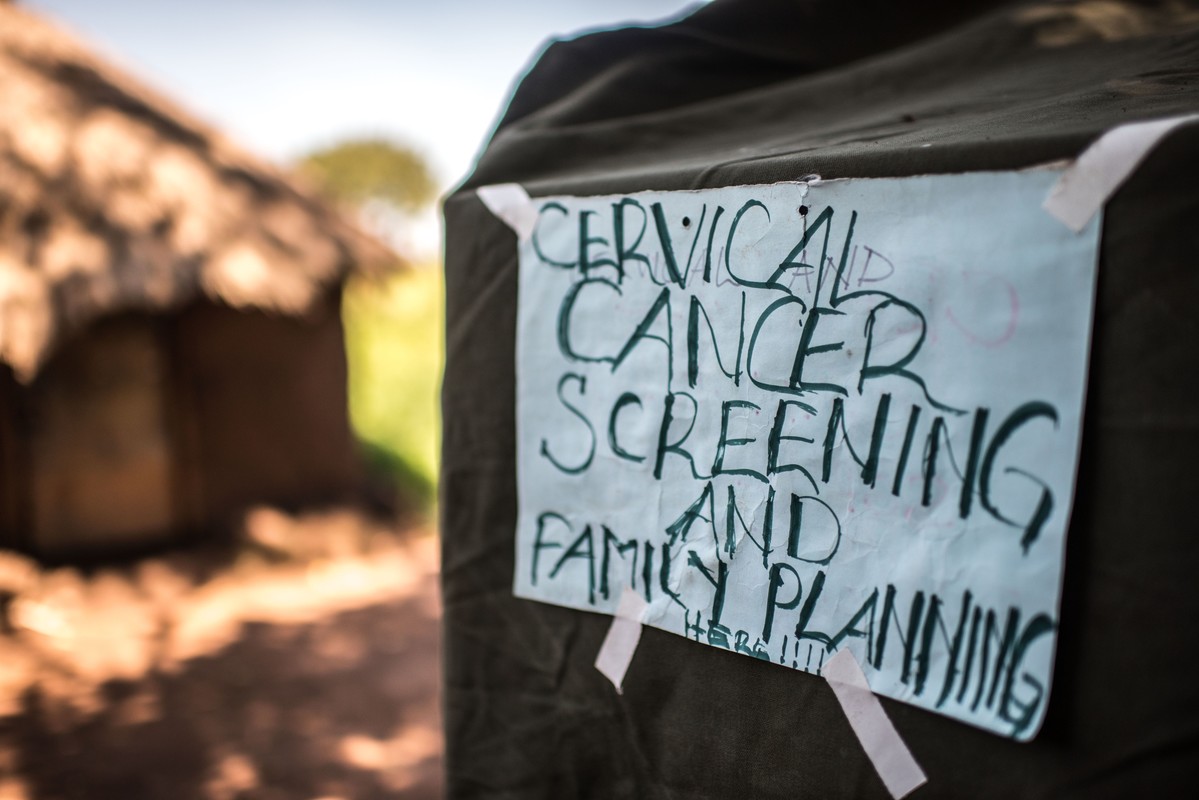
| 22 August 2018
“A radio announcement saved my life” – Gertrude’s story
Gertrude Mugala is a teacher in Fort Portal, a town in Western Uganda. While Gertrude considered herself fairly knowledgeable about cancer, she had never considered taking a screening test or imagined herself ever having the disease. Then one day, she heard an announcement on the radio urging women to go for cervical cancer screenings at a Reproductive Health Uganda (RHU) clinic. “The radio presenter was talking about cervical cancer, and in her message she encouraged all women to get screened. I decided to go and try it out,” she said. Gertrude made her way to RHU's Fort Portal Branch clinic for the free cervical cancer screening. There, she met Ms. Irene Kugonza, an RHU service provider. Ms. Kugonza educated Gertrude and a group of other women about cervical cancer and the importance of routine screening. Gertrude received a type of cervical cancer screening called VIA (visual inspection with acetic acid). "I did not know what was happening" But Gertrude's results were not what she expected; she received a positive result. The good news, however, is that precancerous lesions can be treated if detected early. “I was so shaken when I was told I had pre-cancerous lesions. I did not know what was happening and I didn't believe what I was hearing. I had no idea of my health status. I thought I was healthy, but I was actually harbouring a potential killer disease in me. What would have happened if I didn't go for the screening? If I hadn't heard the radio announcement?” Gertrude was then referred for cryotherapy. “Following cryotherapy, I am now in the process of healing, and I am supposed to go back for review after three months,” said Gertrude. Community screenings Today, Gertrude advocates for cervical cancer screening in her community. She talks to women about cancer, especially cervical cancer, at her workplace, at the market, in meetings, and any other opportunity she gets. “I decided to let women know that cervical cancer is real and it is here with us, and that it kills. At the moment, those are the platforms I have, and I will continue educating women about cancer and encourage them to go for routine testing. I am also happy that I was near my radio that day, where I heard that announcement encouraging all women to get tested for cervical cancer. It might be because of that radio announcement that I am here today,” she said.
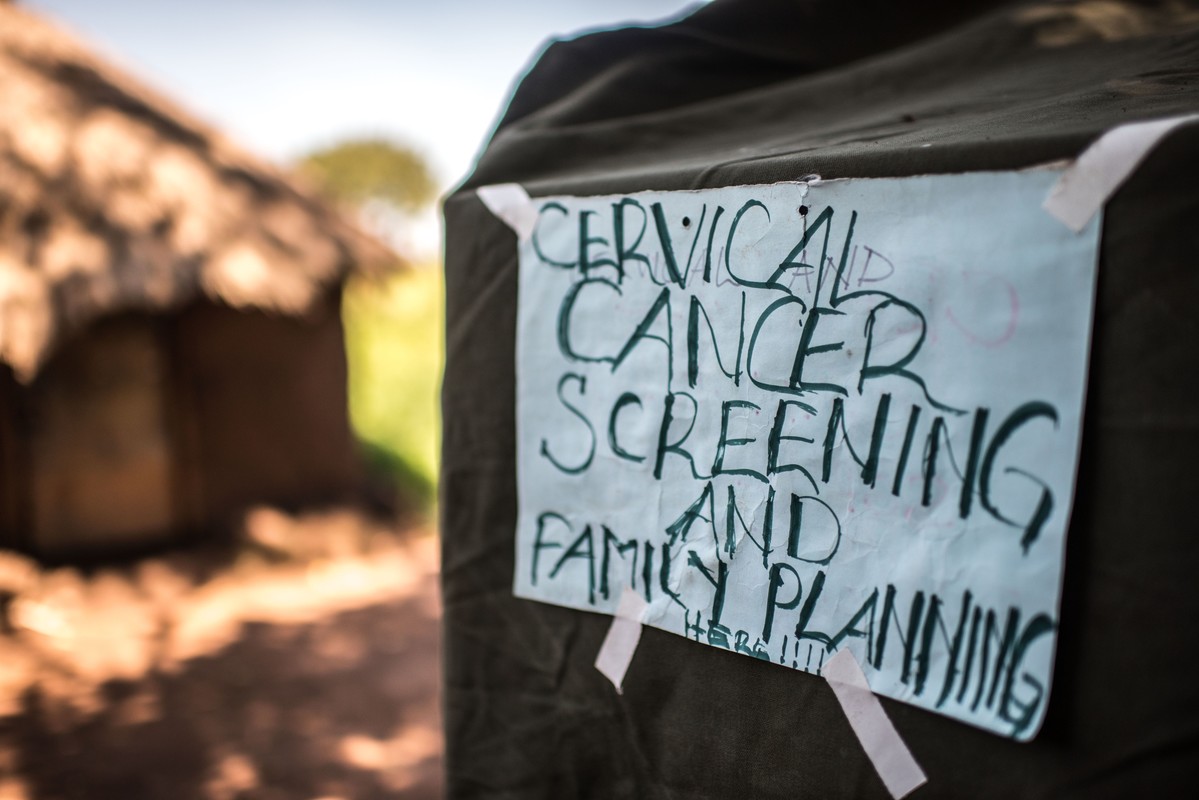
| 15 May 2025
“A radio announcement saved my life” – Gertrude’s story
Gertrude Mugala is a teacher in Fort Portal, a town in Western Uganda. While Gertrude considered herself fairly knowledgeable about cancer, she had never considered taking a screening test or imagined herself ever having the disease. Then one day, she heard an announcement on the radio urging women to go for cervical cancer screenings at a Reproductive Health Uganda (RHU) clinic. “The radio presenter was talking about cervical cancer, and in her message she encouraged all women to get screened. I decided to go and try it out,” she said. Gertrude made her way to RHU's Fort Portal Branch clinic for the free cervical cancer screening. There, she met Ms. Irene Kugonza, an RHU service provider. Ms. Kugonza educated Gertrude and a group of other women about cervical cancer and the importance of routine screening. Gertrude received a type of cervical cancer screening called VIA (visual inspection with acetic acid). "I did not know what was happening" But Gertrude's results were not what she expected; she received a positive result. The good news, however, is that precancerous lesions can be treated if detected early. “I was so shaken when I was told I had pre-cancerous lesions. I did not know what was happening and I didn't believe what I was hearing. I had no idea of my health status. I thought I was healthy, but I was actually harbouring a potential killer disease in me. What would have happened if I didn't go for the screening? If I hadn't heard the radio announcement?” Gertrude was then referred for cryotherapy. “Following cryotherapy, I am now in the process of healing, and I am supposed to go back for review after three months,” said Gertrude. Community screenings Today, Gertrude advocates for cervical cancer screening in her community. She talks to women about cancer, especially cervical cancer, at her workplace, at the market, in meetings, and any other opportunity she gets. “I decided to let women know that cervical cancer is real and it is here with us, and that it kills. At the moment, those are the platforms I have, and I will continue educating women about cancer and encourage them to go for routine testing. I am also happy that I was near my radio that day, where I heard that announcement encouraging all women to get tested for cervical cancer. It might be because of that radio announcement that I am here today,” she said.

| 21 May 2017
A graduate in need turns to sex work
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Lady Mermaid's Bureau. I am Pretty Lynn, aged 25. I am a sex worker but I went to university. I graduated with a Bachelor's Degree in Tourism in 2013. But now, during the day I’m sleeping and during the night I’m working. That is how my day goes every day. I got into sex work through friends. Okay it is not good but I am earning. I tried to get a job when I graduated. I have been applying since I graduated in 2013. I’m still applying but I’m not getting anywhere. You know to get jobs in Uganda; you have to know someone there and no one knows me there. To be a sex worker is like a curse. People look at you like, I don’t know, as someone that has no use in society. People look at you in a bad way. They even don’t consider why you are selling. They just see you as the worst thing that can happen in the society. So it is not comfortable, it is really hard but we try and survive. The fact sex working is illegal means you have to hide yourself when you are selling so that police cannot take you. And then you get diseases, men don’t want to pay. When the police come and take us, sometimes they even use us and don’t pay. So it is really hard. They want a free service. Like if they come and take you and pay that would be fair. But they say it is illegal to sell yourself. But they still use you yet they are saying it is illegal. You can’t report the police because there is no evidence. Abortion and unwanted pregnancies are really common because men don’t want to use condoms and female condoms are really rare and they are expensive. Though at times we get female condoms from Lady Marmaid’s Bureau (LMB) because there are so many of us they can’t keep on giving you them all the time. At times when we get pregnant we use local methods. You can go and use local herbs but it is not safe. One time I used local herbs and I was successful. Then the other time I used Omo washing powder and tea leaves but it was really hard for me. I almost died. I had a friend who died last year from this. But the good thing is that LMB taught us about safe abortion. I have had a safe abortion too. There are some tabs they are called Miso (misoprostol). It costs about fifty thousand shillings (£10 pounds or $20.) It is a lot of money. But if I’m working and I know I’m pregnant, I can say, "this week I’m working for my safe abortion". So if I’m working for twenty thousand, by the end of the week I will have the money. It is expensive compared to Omo at five hundred shillings but that is risky. So if I say I will work this whole week for Miso (misoprostol) it is better. But I'm working and I'm not eating. A project like this one from Lady Mermaid's can help young girls and women. But to take us from sex work, it would really be hard. They would not have enough money to cater for all of us. So what they have to do is to teach us how to protect ourselves, how to defend ourselves. Safe abortion yes. They will just have to sensitise us more about our lives, protection, female condoms and all that. I don't have a boyfriend but maybe when I get money and leave this job I will. But for now, no man would like a woman who sells. No man will bear the wife selling herself. And that will happen only if I get funds, settle somewhere else and become responsible woman. I don’t want this job. I don’t want to be in this business of sex work all the time. I want be married, with my children happily, not selling myself. Stories Read more stories about the amazing success of SAAF in Uganda

| 15 May 2025
A graduate in need turns to sex work
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Lady Mermaid's Bureau. I am Pretty Lynn, aged 25. I am a sex worker but I went to university. I graduated with a Bachelor's Degree in Tourism in 2013. But now, during the day I’m sleeping and during the night I’m working. That is how my day goes every day. I got into sex work through friends. Okay it is not good but I am earning. I tried to get a job when I graduated. I have been applying since I graduated in 2013. I’m still applying but I’m not getting anywhere. You know to get jobs in Uganda; you have to know someone there and no one knows me there. To be a sex worker is like a curse. People look at you like, I don’t know, as someone that has no use in society. People look at you in a bad way. They even don’t consider why you are selling. They just see you as the worst thing that can happen in the society. So it is not comfortable, it is really hard but we try and survive. The fact sex working is illegal means you have to hide yourself when you are selling so that police cannot take you. And then you get diseases, men don’t want to pay. When the police come and take us, sometimes they even use us and don’t pay. So it is really hard. They want a free service. Like if they come and take you and pay that would be fair. But they say it is illegal to sell yourself. But they still use you yet they are saying it is illegal. You can’t report the police because there is no evidence. Abortion and unwanted pregnancies are really common because men don’t want to use condoms and female condoms are really rare and they are expensive. Though at times we get female condoms from Lady Marmaid’s Bureau (LMB) because there are so many of us they can’t keep on giving you them all the time. At times when we get pregnant we use local methods. You can go and use local herbs but it is not safe. One time I used local herbs and I was successful. Then the other time I used Omo washing powder and tea leaves but it was really hard for me. I almost died. I had a friend who died last year from this. But the good thing is that LMB taught us about safe abortion. I have had a safe abortion too. There are some tabs they are called Miso (misoprostol). It costs about fifty thousand shillings (£10 pounds or $20.) It is a lot of money. But if I’m working and I know I’m pregnant, I can say, "this week I’m working for my safe abortion". So if I’m working for twenty thousand, by the end of the week I will have the money. It is expensive compared to Omo at five hundred shillings but that is risky. So if I say I will work this whole week for Miso (misoprostol) it is better. But I'm working and I'm not eating. A project like this one from Lady Mermaid's can help young girls and women. But to take us from sex work, it would really be hard. They would not have enough money to cater for all of us. So what they have to do is to teach us how to protect ourselves, how to defend ourselves. Safe abortion yes. They will just have to sensitise us more about our lives, protection, female condoms and all that. I don't have a boyfriend but maybe when I get money and leave this job I will. But for now, no man would like a woman who sells. No man will bear the wife selling herself. And that will happen only if I get funds, settle somewhere else and become responsible woman. I don’t want this job. I don’t want to be in this business of sex work all the time. I want be married, with my children happily, not selling myself. Stories Read more stories about the amazing success of SAAF in Uganda

| 20 May 2017
Working to stop unsafe abortion for school girls
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Volunteers for Development Association Uganda (VODA). Unsafe abortion is a huge problem in Uganda with an estimated 400,000 women having an unsafe abortion per year. The law is confusing and unclear, with abortion permitted only under certain circumstances. Post-abortion care is permitted to treat women who have undergone an unsafe abortion, however lack of awareness of the law and stigma surrounding abortion mean that service providers are not always willing to treat patients who arrive seeking care. The VODA project aims to ensure that young women in Uganda are able to lead healthier lives free from unsafe abortion related deaths or complications through reducing abortion stigma in the community, increasing access to abortion-related services and ensuring the providers are trained to provide quality post-abortion care services. I am Helen. I have been a midwife at this small clinic for seven years and I have worked with VODA for four years. Unsafe abortion continues and some schoolgirls are raped. They then go to local herbalists and some of them tell me that they are given emilandira [roots] which they insert inside themselves to rupture the membranes. Some of them even try to induce an abortion by using Omo [douching with detergent or bleach]. At the end of the day they get complications then they land here, so we help them. Unsafe abortion is very common. In one month you can get more than five cases. It is a big problem. We help them, they need to go back to school, and we counsel them. If it is less than 12 weeks, we handle them from here. If they are more than 12 weeks along we refer them to the hospital. Most referrals from VODA are related to unwanted pregnancies, HIV testing, family planning, and youth friendly services. A few parents come for services for their children who are at school. So we counsel them that contraception, other than condoms, will only prevent pregnancy, but you can still get HIV and STIs, so take care. I am Josephine and I work as a midwife at a rural health centre. I deal with pregnant mothers, postnatal mothers, and there are girls who come with problems like unwanted pregnancy. I used to have a negative attitude towards abortion. But then VODA helped us understand the importance of helping someone with the problem because many people were dying in the villages because of unsafe abortion. According to my religion, helping someone to have an abortion was not allowed. But again when you look into it, it’s not good to leave someone to die. So I decided to change my attitude to help people. Post-abortion care has helped many people because these days we don’t have many people in the villages dying because of unsafe abortion. These days I’m proud of what we are doing because before I didn’t know the importance of helping someone with a problem. But these days, since people no longer die, people no longer get problems and I’m proud and happy because we help so many people. My name is Jonathan. I am married with three children. I have a Bachelor of Social Work and Social Administration. I have worked with VODA as a project officer since 2008. Due to the training that we have done about abortion many people have changed their attitudes and we have helped people to talk about the issue. Most people were against abortion before but they are now realising that if it’s done safely it is important because otherwise many people die from unsafe abortion. I have talked to religious leaders, I have talked to local leaders; I have talked to people of different categories. At first when you approach them, they have a different perception. The health workers were difficult to work with at first. However they knew people were approaching them with the problems of unsafe abortion. Due to religion, communities can be hard against this issue. But after some time we have seen that they have changed their perception toward the issue of safe and unsafe abortion. And now many of them know that in some instances, abortion is inevitable but it should be done in a safe way. I’m Stevens and I am nurse. We have some clients who come when they have already attempted an unsafe abortion. You find that it is often inevitable. The only solution you have to help those clients is to provide treatment of incomplete abortion as part of post-abortion care. Because of the VODA project there is a very remarkable change in the community. Now, those people who used to have unsafe abortions locally, know where to go for post-abortion care - unlike in the past. I remember a schoolgirl, she was in a very sorry state because she had tried some local remedies to abort. I attended to her and things went well. She went back to school. I feel so proud because that was a big life rescue. A girl like that could have died but now she is alive and I see her carrying on with her studies, I feel so proud. I praise VODA for that encouragement. This service should be legalised because whether they restrict it or not, there is abortion and it is going on. And if it’s not out in the open, so that our people know where to go for such services, it leads to more deaths. Stories Read more stories about the amazing success of SAAF in Uganda

| 15 May 2025
Working to stop unsafe abortion for school girls
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Volunteers for Development Association Uganda (VODA). Unsafe abortion is a huge problem in Uganda with an estimated 400,000 women having an unsafe abortion per year. The law is confusing and unclear, with abortion permitted only under certain circumstances. Post-abortion care is permitted to treat women who have undergone an unsafe abortion, however lack of awareness of the law and stigma surrounding abortion mean that service providers are not always willing to treat patients who arrive seeking care. The VODA project aims to ensure that young women in Uganda are able to lead healthier lives free from unsafe abortion related deaths or complications through reducing abortion stigma in the community, increasing access to abortion-related services and ensuring the providers are trained to provide quality post-abortion care services. I am Helen. I have been a midwife at this small clinic for seven years and I have worked with VODA for four years. Unsafe abortion continues and some schoolgirls are raped. They then go to local herbalists and some of them tell me that they are given emilandira [roots] which they insert inside themselves to rupture the membranes. Some of them even try to induce an abortion by using Omo [douching with detergent or bleach]. At the end of the day they get complications then they land here, so we help them. Unsafe abortion is very common. In one month you can get more than five cases. It is a big problem. We help them, they need to go back to school, and we counsel them. If it is less than 12 weeks, we handle them from here. If they are more than 12 weeks along we refer them to the hospital. Most referrals from VODA are related to unwanted pregnancies, HIV testing, family planning, and youth friendly services. A few parents come for services for their children who are at school. So we counsel them that contraception, other than condoms, will only prevent pregnancy, but you can still get HIV and STIs, so take care. I am Josephine and I work as a midwife at a rural health centre. I deal with pregnant mothers, postnatal mothers, and there are girls who come with problems like unwanted pregnancy. I used to have a negative attitude towards abortion. But then VODA helped us understand the importance of helping someone with the problem because many people were dying in the villages because of unsafe abortion. According to my religion, helping someone to have an abortion was not allowed. But again when you look into it, it’s not good to leave someone to die. So I decided to change my attitude to help people. Post-abortion care has helped many people because these days we don’t have many people in the villages dying because of unsafe abortion. These days I’m proud of what we are doing because before I didn’t know the importance of helping someone with a problem. But these days, since people no longer die, people no longer get problems and I’m proud and happy because we help so many people. My name is Jonathan. I am married with three children. I have a Bachelor of Social Work and Social Administration. I have worked with VODA as a project officer since 2008. Due to the training that we have done about abortion many people have changed their attitudes and we have helped people to talk about the issue. Most people were against abortion before but they are now realising that if it’s done safely it is important because otherwise many people die from unsafe abortion. I have talked to religious leaders, I have talked to local leaders; I have talked to people of different categories. At first when you approach them, they have a different perception. The health workers were difficult to work with at first. However they knew people were approaching them with the problems of unsafe abortion. Due to religion, communities can be hard against this issue. But after some time we have seen that they have changed their perception toward the issue of safe and unsafe abortion. And now many of them know that in some instances, abortion is inevitable but it should be done in a safe way. I’m Stevens and I am nurse. We have some clients who come when they have already attempted an unsafe abortion. You find that it is often inevitable. The only solution you have to help those clients is to provide treatment of incomplete abortion as part of post-abortion care. Because of the VODA project there is a very remarkable change in the community. Now, those people who used to have unsafe abortions locally, know where to go for post-abortion care - unlike in the past. I remember a schoolgirl, she was in a very sorry state because she had tried some local remedies to abort. I attended to her and things went well. She went back to school. I feel so proud because that was a big life rescue. A girl like that could have died but now she is alive and I see her carrying on with her studies, I feel so proud. I praise VODA for that encouragement. This service should be legalised because whether they restrict it or not, there is abortion and it is going on. And if it’s not out in the open, so that our people know where to go for such services, it leads to more deaths. Stories Read more stories about the amazing success of SAAF in Uganda

| 20 May 2017
A mother's heart break after losing teen daughter to unsafe abortion
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Volunteers for Development Association Uganda (VODA). Margaret's daughter, Gladys, was raped by a relative as a teenager and became pregnant. She did not tell her mother what had happened and not wanting to have a child at such a young age conceived through incest, Gladys tried to terminate the pregnancy herself using local herbs but got an infection and died. "My name is Margaret and I am a widow." "I lost my daughter in 2011. She was called Gladys and she was 16. I didn’t know that she was pregnant. She tried to use local herbs to abort. I only found out about it three days later when she was bleeding very heavily. I tried to take her to the hospital but unfortunately she died on the way." Despite being the cause of many deaths in the region, the stigma surrounding abortion means that most people do not mention the cause of death publically. However at Gladys' funeral one of her school friends spoke out and said that she had died due to unsafe abortion. This prompted VODA to start working on the issue and when the project started they included Margaret in their training on how to prevent unsafe abortion. "The training made me stronger to talk about it. Now, I continue to tell my remaining two girls about the dangers of unsafe abortion, sexually transmitted infections and unwanted pregnancies. VODA has really helped us. I think my girl wouldn’t have died if VODA was active then like it is now." "I have used VODA's information to carry on with my parental work. That information has been helpful because we are noticing change. I keep on reminding them, 'didn’t you see what happened to your friend here?'. So they have really changed especially with the ongoing help of the people from VODA." "Unsafe abortion was rampant in the past. We had tried to speak to the students, as parents, but it seemed that our information was not enough. But now we have another helping hand from VODA, especially with those seminars targeting the girls." Stories Read more stories about the amazing success of SAAF in Uganda

| 15 May 2025
A mother's heart break after losing teen daughter to unsafe abortion
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Volunteers for Development Association Uganda (VODA). Margaret's daughter, Gladys, was raped by a relative as a teenager and became pregnant. She did not tell her mother what had happened and not wanting to have a child at such a young age conceived through incest, Gladys tried to terminate the pregnancy herself using local herbs but got an infection and died. "My name is Margaret and I am a widow." "I lost my daughter in 2011. She was called Gladys and she was 16. I didn’t know that she was pregnant. She tried to use local herbs to abort. I only found out about it three days later when she was bleeding very heavily. I tried to take her to the hospital but unfortunately she died on the way." Despite being the cause of many deaths in the region, the stigma surrounding abortion means that most people do not mention the cause of death publically. However at Gladys' funeral one of her school friends spoke out and said that she had died due to unsafe abortion. This prompted VODA to start working on the issue and when the project started they included Margaret in their training on how to prevent unsafe abortion. "The training made me stronger to talk about it. Now, I continue to tell my remaining two girls about the dangers of unsafe abortion, sexually transmitted infections and unwanted pregnancies. VODA has really helped us. I think my girl wouldn’t have died if VODA was active then like it is now." "I have used VODA's information to carry on with my parental work. That information has been helpful because we are noticing change. I keep on reminding them, 'didn’t you see what happened to your friend here?'. So they have really changed especially with the ongoing help of the people from VODA." "Unsafe abortion was rampant in the past. We had tried to speak to the students, as parents, but it seemed that our information was not enough. But now we have another helping hand from VODA, especially with those seminars targeting the girls." Stories Read more stories about the amazing success of SAAF in Uganda

| 20 May 2017
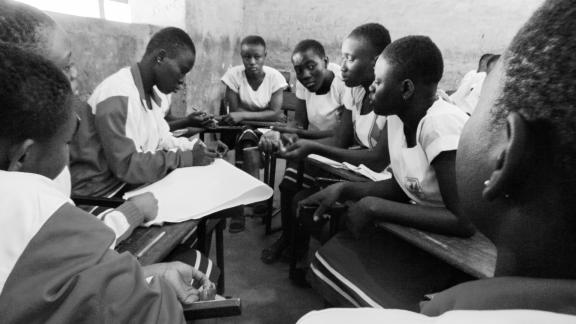
Educating their peers about unsafe abortion
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grassroots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Volunteers for Development Association Uganda (VODA). Peer educators in schools provide counselling and advice to other students, who otherwise would have no one to turn to in times of crisis. Today, we have the largest generation of young people ever, each one with their own unique needs. Peer educators are critical in gaining the trust and confidence of hundreds of young girls each term, and together they help each other gain more knowledge about their sexual and reproductive health. Peer educators themselves also gain a great deal from the training and experience and VODA has been successful in empowering many of these young girls to feel confident and be able to talk out in public, something that they were not able to do before. Poverty, gender inequality, lack of knowledge about sex and relationships and lack of access to sanitary protection mean that girls in rural Uganda are at high risk of sexual exploitation and abuse. All of this coupled with very little access to contraception means that Uganda has high rates of unintended pregnancies among young girls. Despite abortion being legal in Uganda in cases of rape and incest, most girls are not aware of the law and resort to unsafe abortion often using local herbs or washing liquid. The peer educators trained by VODA are able to listen to other young people's issues and provide support and information a range of issues including safe abortion as well as how to access contraception. My name is Mabel. I am in my final year of O'Levels and I am a peer counsellor at a Secondary School in Namuganga. I was selected with two others by VODA and my head teacher, and then trained to be a peer counsellor. We were trained to help our colleagues at school to handle various problems. Girls used to get pregnant and some were dropping out of school. So we counselled many of our colleagues about unwanted pregnancies. We have seen a change because we get free condoms from VODA. We could preach abstinence from sex. For those that could not manage abstinence, we could give them male condoms. Unsafe abortion has been a big problem. Girls were using local herbs and sharp instruments like metallic hangers for abortion. Many would get injured and some would die. I remember last year there was a girl who aborted using those local methods but she died and was buried in Seeta. If VODA wasn't here I think things would be very bad because as students, we did not have access to most of the information that we needed. We would have seen a big number of girls out of school because of unwanted pregnancies or unsafe abortion. I have benefited a lot. I have acquired information which I have used to keep myself safe in terms of unwanted pregnancies. I don’t think I could ever be lured to perform unsafe abortion because I know the risks. In the past, I wasn't able to speak in public but now I can stand and talk freely. I’m Sharon and I’m a student counsellor at a Secondary School in Namuganga. I counsel fellow students, young people in communities and even adults. Before I was selected for VODA training I thought it was just an organisation to promote abortion. But then I realised they were addressing a big problem that was happening at our school and our villages. I have learnt that when someone gets pregnant I don’t have to force her to abort and I don’t encourage her to go for unsafe abortion. If we hear that a certain girl has a boyfriend, we approach her and counsel her on issues like unwanted pregnancy. Many young girls have been lured into early sex because they need money, which is why we end up with unwanted pregnancies. In a bid to fulfil those needs, they get boyfriends or other guys who use them for money, impregnate them and then leave. The girls know about contraceptives like the pill and we have given some of them referral cards for them to access the contraceptives from the health centres. But there has been debate against giving young girls contraceptives. There are restrictions that the government puts in place but that does not mean that girls are not getting pregnant. I remember the girls who died after aborting through unsafe abortion methods and I think about the lives that would have been saved if they had knowledge about contraceptives. I’m Rita and I’m 15-years-old. I was twelve when I was selected to be a VODA counsellor in my primary school. I was lucky because many people wanted to be counsellors but I was chosen. My parents were very happy and they got interested. When I joined this school, I introduced myself to other students because I wanted to continue with my work as a counsellor. I told my colleagues to feel free to share with me their issues. We are lucky here because there are many counsellors. Girls are having unwanted pregnancies because they are lured by men who give them presents and things such as money for sanitary pads that they cannot get from their parents. Before I joined this school, there were many cases of girls terminating pregnancies with unsafe abortions. It was common to hear of or see someone who had aborted. Many would abort so that they would return to school. When I joined this school last year and we intensified the counselling sessions, many came and shared their problems with us. We have learnt that two girls at school gave birth and have since returned to school but we have not had cases of unsafe abortions here since I joined. I wasn’t as serious with studies before I became a counsellor but because I want to maintain my status, I have improved in my studies because I don’t want to feel ashamed in front of my fellow students. VODA gave us T-shirts for identification purposes which has made people in the community respect me as well. In terms of preventing unwanted pregnancies in schools, most of what we see here originates from the girls' homes. Many parents don’t provide for the girls’ necessities (like sanitary towels) so that makes them vulnerable to be lured by men. Stories Read more stories about the amazing success of SAAF in Uganda

| 15 May 2025
Educating their peers about unsafe abortion
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grassroots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Volunteers for Development Association Uganda (VODA). Peer educators in schools provide counselling and advice to other students, who otherwise would have no one to turn to in times of crisis. Today, we have the largest generation of young people ever, each one with their own unique needs. Peer educators are critical in gaining the trust and confidence of hundreds of young girls each term, and together they help each other gain more knowledge about their sexual and reproductive health. Peer educators themselves also gain a great deal from the training and experience and VODA has been successful in empowering many of these young girls to feel confident and be able to talk out in public, something that they were not able to do before. Poverty, gender inequality, lack of knowledge about sex and relationships and lack of access to sanitary protection mean that girls in rural Uganda are at high risk of sexual exploitation and abuse. All of this coupled with very little access to contraception means that Uganda has high rates of unintended pregnancies among young girls. Despite abortion being legal in Uganda in cases of rape and incest, most girls are not aware of the law and resort to unsafe abortion often using local herbs or washing liquid. The peer educators trained by VODA are able to listen to other young people's issues and provide support and information a range of issues including safe abortion as well as how to access contraception. My name is Mabel. I am in my final year of O'Levels and I am a peer counsellor at a Secondary School in Namuganga. I was selected with two others by VODA and my head teacher, and then trained to be a peer counsellor. We were trained to help our colleagues at school to handle various problems. Girls used to get pregnant and some were dropping out of school. So we counselled many of our colleagues about unwanted pregnancies. We have seen a change because we get free condoms from VODA. We could preach abstinence from sex. For those that could not manage abstinence, we could give them male condoms. Unsafe abortion has been a big problem. Girls were using local herbs and sharp instruments like metallic hangers for abortion. Many would get injured and some would die. I remember last year there was a girl who aborted using those local methods but she died and was buried in Seeta. If VODA wasn't here I think things would be very bad because as students, we did not have access to most of the information that we needed. We would have seen a big number of girls out of school because of unwanted pregnancies or unsafe abortion. I have benefited a lot. I have acquired information which I have used to keep myself safe in terms of unwanted pregnancies. I don’t think I could ever be lured to perform unsafe abortion because I know the risks. In the past, I wasn't able to speak in public but now I can stand and talk freely. I’m Sharon and I’m a student counsellor at a Secondary School in Namuganga. I counsel fellow students, young people in communities and even adults. Before I was selected for VODA training I thought it was just an organisation to promote abortion. But then I realised they were addressing a big problem that was happening at our school and our villages. I have learnt that when someone gets pregnant I don’t have to force her to abort and I don’t encourage her to go for unsafe abortion. If we hear that a certain girl has a boyfriend, we approach her and counsel her on issues like unwanted pregnancy. Many young girls have been lured into early sex because they need money, which is why we end up with unwanted pregnancies. In a bid to fulfil those needs, they get boyfriends or other guys who use them for money, impregnate them and then leave. The girls know about contraceptives like the pill and we have given some of them referral cards for them to access the contraceptives from the health centres. But there has been debate against giving young girls contraceptives. There are restrictions that the government puts in place but that does not mean that girls are not getting pregnant. I remember the girls who died after aborting through unsafe abortion methods and I think about the lives that would have been saved if they had knowledge about contraceptives. I’m Rita and I’m 15-years-old. I was twelve when I was selected to be a VODA counsellor in my primary school. I was lucky because many people wanted to be counsellors but I was chosen. My parents were very happy and they got interested. When I joined this school, I introduced myself to other students because I wanted to continue with my work as a counsellor. I told my colleagues to feel free to share with me their issues. We are lucky here because there are many counsellors. Girls are having unwanted pregnancies because they are lured by men who give them presents and things such as money for sanitary pads that they cannot get from their parents. Before I joined this school, there were many cases of girls terminating pregnancies with unsafe abortions. It was common to hear of or see someone who had aborted. Many would abort so that they would return to school. When I joined this school last year and we intensified the counselling sessions, many came and shared their problems with us. We have learnt that two girls at school gave birth and have since returned to school but we have not had cases of unsafe abortions here since I joined. I wasn’t as serious with studies before I became a counsellor but because I want to maintain my status, I have improved in my studies because I don’t want to feel ashamed in front of my fellow students. VODA gave us T-shirts for identification purposes which has made people in the community respect me as well. In terms of preventing unwanted pregnancies in schools, most of what we see here originates from the girls' homes. Many parents don’t provide for the girls’ necessities (like sanitary towels) so that makes them vulnerable to be lured by men. Stories Read more stories about the amazing success of SAAF in Uganda

| 20 May 2017
Post-abortion care for straight-A student
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was a fund set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such project which received funding is called Volunteers for Development Association Uganda (VODA). My name is Anne*, I am 14-years-old, I am a student at one of the local schools near my (rural) village. I recently went to the health centre for post-abortion care. I was referred there by VODA and I was helped by the mid-wife, her name was Grace. The VODA community volunteers, they found me at my grandmother's house. They brought me to the health centre. I was on my way to visit my grandmother. A man just caught me. After he finished with me he told me to go back home and never to tell anyone about it. I went back home to my parents, in Luwero District. There is no VODA there. I realised I was pregnant because I found out I had missed my periods. Then I told my mother. My mother said we should try to do something about the pregnancy, but not in our home district, otherwise my father would not longer pay my school fees. I had just finished my Primary Leaving Examinations and I was looking forward to joining secondary. So then I had to go back to my grandmother's house. She said we were going to the hospital but it wasn't like the one where Grace works, where I finally got my post-abortion treatment. She took me to a place where a woman gave me some herbs. Then we went home and the thing came out. I was bleeding. Then the VODA counsellor came to my home and suggested to my grandmother that I should be taken for treatment. I had learnt about how girls can get pregnant but I didn't know anything about safe abortion. In Luwero, where I come from, many girls I hear they use herbs to abort but I had not tried it because I had not had any sex until that man forced me. I am telling my friends about safe abortion and contraceptive services but I also need to be given more information about it because I was not taught about most of what Grace the midwife was telling me. I know that women can take precautions for family planning like pills but my mum told me it's only for married people. I am very thankful to VODA, I maybe could have died if the counsellors from VODA hadn't asked to rush me to the health centre for post-abortion care. *Not her real name Stories Read more stories about the amazing success of SAAF in Uganda

| 15 May 2025
Post-abortion care for straight-A student
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was a fund set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such project which received funding is called Volunteers for Development Association Uganda (VODA). My name is Anne*, I am 14-years-old, I am a student at one of the local schools near my (rural) village. I recently went to the health centre for post-abortion care. I was referred there by VODA and I was helped by the mid-wife, her name was Grace. The VODA community volunteers, they found me at my grandmother's house. They brought me to the health centre. I was on my way to visit my grandmother. A man just caught me. After he finished with me he told me to go back home and never to tell anyone about it. I went back home to my parents, in Luwero District. There is no VODA there. I realised I was pregnant because I found out I had missed my periods. Then I told my mother. My mother said we should try to do something about the pregnancy, but not in our home district, otherwise my father would not longer pay my school fees. I had just finished my Primary Leaving Examinations and I was looking forward to joining secondary. So then I had to go back to my grandmother's house. She said we were going to the hospital but it wasn't like the one where Grace works, where I finally got my post-abortion treatment. She took me to a place where a woman gave me some herbs. Then we went home and the thing came out. I was bleeding. Then the VODA counsellor came to my home and suggested to my grandmother that I should be taken for treatment. I had learnt about how girls can get pregnant but I didn't know anything about safe abortion. In Luwero, where I come from, many girls I hear they use herbs to abort but I had not tried it because I had not had any sex until that man forced me. I am telling my friends about safe abortion and contraceptive services but I also need to be given more information about it because I was not taught about most of what Grace the midwife was telling me. I know that women can take precautions for family planning like pills but my mum told me it's only for married people. I am very thankful to VODA, I maybe could have died if the counsellors from VODA hadn't asked to rush me to the health centre for post-abortion care. *Not her real name Stories Read more stories about the amazing success of SAAF in Uganda

| 20 May 2017
Tackling taboos about abortion
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Volunteers for Development Association Uganda (VODA). Teachers and community volunteers provide support for young people in schools. They are critical in reshaping the social norms and stigma surrounding teen pregnancies. For many young girls, an unwanted pregnancy can limit their education and significantly restrict their life options. In Uganda, teachers are now helping to provide counselling for girls on contraception and safe abortion. Prior to VODA working with schools to provide teachers with training, the rate of deaths from unsafe abortion was significantly high. This was even the case in primary schools. Now the prevalence of unwanted pregnancies has dropped and girls are more aware of their sexual and reproductive health. I’m Deborah. I’m 27-years-old and I'm a teacher as well as being a community volunteer with VODA Uganda. There is a problem with unsafe abortion and teenage pregnancies in this area. Young girls have been getting pregnant and some of them have been dropping out of school. Some have even died because of unsafe abortions. When VODA came in, they taught us about teenage pregnancies and unsafe abortion. So we came in to teach young people in the villages so that they can be aware of these issues. Many girls secretly use injectable contraceptives after being told to do so by their parents. When these parents realise that their daughters are sexually active, they fear that they could get pregnant before they complete school. They do it secretly because they fear stigma. They do it that way to avoid rumours that may circulate if they know that one’s daughter was taken for family planning while she is still at school. Many people in our community think that a teenager who is on contraceptives is spoilt. When I had just come to this area, incidents of unsafe abortion were high. But when I began working here and the girls came to know about me, I began counselling them about safe sex, contraceptives and condoms. I told them that if you think you cannot have protected sex, then you need to use contraceptives. But we also warned them against sexually transmitted infections. Using contraception has reduced the number of girls engaging in unsafe abortion. There are different local methods used to abort. Some of them would get complications that needed medical attention after trying these methods. Some would also secretly try to go to health centres after the abortion had gone wrongly or they had even nearly died. Now some of those that have unwanted pregnancies do approach me and I counsel them. In the past, if one talked about abortion or unwanted pregnancies, I would harshly judge her saying that she wanted it. But having become a volunteer with VODA I have learned sometimes the pregnancies are due to defilement or rape, so I came to understand that not all those that get pregnant want to have a child. Sometimes abortion is inevitable. For example, when a girl has been raped by her father, uncle, brothers or close relatives. How would a girl carry that baby? It is very important to educate young people about unsafe abortion, especially when they have reached that stage when they can get pregnant. That will help them to prevent having unwanted pregnancies and also to avoid unsafe abortion. It is important to give young girls contraceptives because some will have premarital sex. So such girls must have contraceptives if they are to avoid getting pregnant. I am Mily and I am 38-years-old. I am a volunteer for VODA Uganda and a teacher at a primary school in Kasawo. I have been teaching here for eight years. Before VODA was here, there were a lot of school dropouts from girls. They were getting unwanted pregnancies whereby they were forced to leave school. There was no one to counsel them. They were using local medicines for unsafe abortion. But when VODA came in they started to advise about unsafe abortion. We are working together with doctors and nurses from various hospitals so girls could get good care. VODA workers approached us and explained how it could help our children to stay in school. Then we had a workshop and our head teacher selected who would manage this. Before VODA came in unsafe abortion was rampant. Many of the girls were dying. Here at this school we had a girl in P4 - we were not even expecting that girl could be pregnant. Unfortunately, we heard about it when the girl was already dead. She was trying to have an unsafe abortion. Before VODA came, there was no sexuality education or counselling to do with STIs. That is why our children were dying because they feared to tell their parents. We thought that pregnant girls should leave school without further assistance. But as a volunteer, I thank VODA because now I know that that girls can be helped and they can continue with their studies. I am Frida and I'm 18-years-old. I am a peer counsellor at school and have counselled many girls about unsafe abortion. I came to know about VODA on a careers day at school and by attending training workshops on unsafe abortion. At our school, I’m very well-known as a youth counsellor. I help other girls who are sexually active with unwanted pregnancies. The training I received from VODA has given me self-confidence. Before, I couldn’t stand in public. But now I can stand in the presence of even one thousand people and I can talk. I’m not shy anymore. The problems are that girls can't access services like post-abortion care and family planning, like the pill. Girls are poor. Some services need money yet some girls don’t have money. They are getting pregnant because they have less information about unprotected sex and they are sexually active. To help them there needs to be places where they can find such services. From my training with VODA I now want to be a social worker so that I can work with people. I have realised that I can handle people well. Stories Read more stories about the amazing success of SAAF in Uganda

| 15 May 2025
Tackling taboos about abortion
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Volunteers for Development Association Uganda (VODA). Teachers and community volunteers provide support for young people in schools. They are critical in reshaping the social norms and stigma surrounding teen pregnancies. For many young girls, an unwanted pregnancy can limit their education and significantly restrict their life options. In Uganda, teachers are now helping to provide counselling for girls on contraception and safe abortion. Prior to VODA working with schools to provide teachers with training, the rate of deaths from unsafe abortion was significantly high. This was even the case in primary schools. Now the prevalence of unwanted pregnancies has dropped and girls are more aware of their sexual and reproductive health. I’m Deborah. I’m 27-years-old and I'm a teacher as well as being a community volunteer with VODA Uganda. There is a problem with unsafe abortion and teenage pregnancies in this area. Young girls have been getting pregnant and some of them have been dropping out of school. Some have even died because of unsafe abortions. When VODA came in, they taught us about teenage pregnancies and unsafe abortion. So we came in to teach young people in the villages so that they can be aware of these issues. Many girls secretly use injectable contraceptives after being told to do so by their parents. When these parents realise that their daughters are sexually active, they fear that they could get pregnant before they complete school. They do it secretly because they fear stigma. They do it that way to avoid rumours that may circulate if they know that one’s daughter was taken for family planning while she is still at school. Many people in our community think that a teenager who is on contraceptives is spoilt. When I had just come to this area, incidents of unsafe abortion were high. But when I began working here and the girls came to know about me, I began counselling them about safe sex, contraceptives and condoms. I told them that if you think you cannot have protected sex, then you need to use contraceptives. But we also warned them against sexually transmitted infections. Using contraception has reduced the number of girls engaging in unsafe abortion. There are different local methods used to abort. Some of them would get complications that needed medical attention after trying these methods. Some would also secretly try to go to health centres after the abortion had gone wrongly or they had even nearly died. Now some of those that have unwanted pregnancies do approach me and I counsel them. In the past, if one talked about abortion or unwanted pregnancies, I would harshly judge her saying that she wanted it. But having become a volunteer with VODA I have learned sometimes the pregnancies are due to defilement or rape, so I came to understand that not all those that get pregnant want to have a child. Sometimes abortion is inevitable. For example, when a girl has been raped by her father, uncle, brothers or close relatives. How would a girl carry that baby? It is very important to educate young people about unsafe abortion, especially when they have reached that stage when they can get pregnant. That will help them to prevent having unwanted pregnancies and also to avoid unsafe abortion. It is important to give young girls contraceptives because some will have premarital sex. So such girls must have contraceptives if they are to avoid getting pregnant. I am Mily and I am 38-years-old. I am a volunteer for VODA Uganda and a teacher at a primary school in Kasawo. I have been teaching here for eight years. Before VODA was here, there were a lot of school dropouts from girls. They were getting unwanted pregnancies whereby they were forced to leave school. There was no one to counsel them. They were using local medicines for unsafe abortion. But when VODA came in they started to advise about unsafe abortion. We are working together with doctors and nurses from various hospitals so girls could get good care. VODA workers approached us and explained how it could help our children to stay in school. Then we had a workshop and our head teacher selected who would manage this. Before VODA came in unsafe abortion was rampant. Many of the girls were dying. Here at this school we had a girl in P4 - we were not even expecting that girl could be pregnant. Unfortunately, we heard about it when the girl was already dead. She was trying to have an unsafe abortion. Before VODA came, there was no sexuality education or counselling to do with STIs. That is why our children were dying because they feared to tell their parents. We thought that pregnant girls should leave school without further assistance. But as a volunteer, I thank VODA because now I know that that girls can be helped and they can continue with their studies. I am Frida and I'm 18-years-old. I am a peer counsellor at school and have counselled many girls about unsafe abortion. I came to know about VODA on a careers day at school and by attending training workshops on unsafe abortion. At our school, I’m very well-known as a youth counsellor. I help other girls who are sexually active with unwanted pregnancies. The training I received from VODA has given me self-confidence. Before, I couldn’t stand in public. But now I can stand in the presence of even one thousand people and I can talk. I’m not shy anymore. The problems are that girls can't access services like post-abortion care and family planning, like the pill. Girls are poor. Some services need money yet some girls don’t have money. They are getting pregnant because they have less information about unprotected sex and they are sexually active. To help them there needs to be places where they can find such services. From my training with VODA I now want to be a social worker so that I can work with people. I have realised that I can handle people well. Stories Read more stories about the amazing success of SAAF in Uganda

| 05 January 2022
In pictures: The changemaker keeping her community healthy and happy
The Get Up, Speak Out! initiative works with and for young people to overcome barriers such as unequal gender norms, negative attitudes towards sexuality, taboos about sex, menstruation, and abortion. Empowering youth communities - especially girls and young women - with information and knowledge about sexual and reproductive health, and the provision of access to health and contraceptive care, is at the heart of the initiative. Get Up, Speak Out! is an international initiative developed by a consortium of partners including IPPF, Rutgers, CHOICE for Youth & Sexuality, Dance4Life, Simavi, and Aidsfonds, with support from the Dutch Ministry of Foreign Affairs.

| 15 May 2025
In pictures: The changemaker keeping her community healthy and happy
The Get Up, Speak Out! initiative works with and for young people to overcome barriers such as unequal gender norms, negative attitudes towards sexuality, taboos about sex, menstruation, and abortion. Empowering youth communities - especially girls and young women - with information and knowledge about sexual and reproductive health, and the provision of access to health and contraceptive care, is at the heart of the initiative. Get Up, Speak Out! is an international initiative developed by a consortium of partners including IPPF, Rutgers, CHOICE for Youth & Sexuality, Dance4Life, Simavi, and Aidsfonds, with support from the Dutch Ministry of Foreign Affairs.

| 03 March 2021
The response to Tropical Cyclone Yasa: Through the eyes of a humanitarian surge member
Sera Vulavou is the Senior Monitoring and Evaluation Officer with IPPF’s Sub-Regional Office for the Pacific. She was trained as a humanitarian surge roster member in early 2020, to be able to deploy to emergencies to provide technical assistance to Member Associations – here she shares her experience with us. Severe Tropical Cyclone (TC) Yasa was the strongest in the South Pacific since TC Winston in 2016, as well as the fourth most intense TC on record in the basin. The Reproductive and Family Health Association of Fiji (RFHAF) humanitarian response to TC Yasa has reached some of the most difficult and geographically scattered islands and communities, which included the islands of Moala, Totoya, and Matuku. Being part of the IPPF humanitarian surge roster team gave me the opportunity to accompany the RFHAF response team during their humanitarian work. This experience was about putting in action what I could only personally describe as being at the right place at the right time.

| 15 May 2025
The response to Tropical Cyclone Yasa: Through the eyes of a humanitarian surge member
Sera Vulavou is the Senior Monitoring and Evaluation Officer with IPPF’s Sub-Regional Office for the Pacific. She was trained as a humanitarian surge roster member in early 2020, to be able to deploy to emergencies to provide technical assistance to Member Associations – here she shares her experience with us. Severe Tropical Cyclone (TC) Yasa was the strongest in the South Pacific since TC Winston in 2016, as well as the fourth most intense TC on record in the basin. The Reproductive and Family Health Association of Fiji (RFHAF) humanitarian response to TC Yasa has reached some of the most difficult and geographically scattered islands and communities, which included the islands of Moala, Totoya, and Matuku. Being part of the IPPF humanitarian surge roster team gave me the opportunity to accompany the RFHAF response team during their humanitarian work. This experience was about putting in action what I could only personally describe as being at the right place at the right time.

| 13 August 2020
In pictures: Delivering healthcare to remote communities in Fiji
In early April 2020, the all too familiar destruction of a Tropical Cyclone (TC) – Harold – hit the Solomon Islands, Vanuatu, Fiji and Tonga. One of the worst affected areas was the Eastern part of Fiji. Through support by Department of Foreign Affairs and Trade (DFAT), our Member Association, Reproductive and Family Health Association of Fiji (RFHAF), was quick to respond ensuring access to essential sexual and reproductive healthcare for Kadavu’s women, girls, and vulnerable groups. Fiji's vulnerable coastline Fiji’s worst affected area was the Eastern part, with TC Harold bringing destructive storm force winds and storm surge. RFHAF focused its humanitarian response on the local Kadavu population. This remote area proves a challenge to reach for the team with supplies. Share on Twitter Share on Facebook Share via WhatsApp Share via Email RFHAF's humanitarian response team tackle rough terrain National travel restrictions - due to the current COVID-19 pandemic - on all inter island transfers has slowed the response in some areas, including Kadavu. The island of Kadavu is one of the least developed areas of Fiji, the main source of income is substance living (Yaqona). Transport around the island is difficult, with very few roads, no public water system or electricity. The humanitarian team from RFHAF travels by boat and then on foot. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Asenaca, client Kadavu, the biggest island in the Eastern division has the greatest population (10,897). 197 evacuation centres were activated in total, initially hosting over 6,240 people. Many are women of reproductive age, with an estimated 150 currently pregnant. Asenaca learns about breast cancer self-checks from RFHAF’s healthcare provider, Karo. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nasi, RFHAF healthcare provider The medical mobile team deliver a broad range of healthcare including contraception, information and counselling on sexual health, pregnancy, HIV and STI care and testing. RFHAF Team in Kadavu performing general health checks after TC Harold. Nasi administers a HPV shot to a client. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Kate, client Young women and girls are at the heart of RFHAF’s healthcare provision. Kate walks home with her dignity kit after a health check at the mobile clinic. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Karo, RFHAF healthcare worker RFHAF offers sexual and reproductive healthcare as well as counselling, and referrals for follow up care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Alidi, RFHAF healthcare worker The team ensures young people in the community are not forgotten and provide information and education on relationships and sexual health and rights. Alidi conducting a session with a local group of young people at Gasele, Kadavu.Photos ©IPPF/Rob Rickman/Fiji Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 15 May 2025
In pictures: Delivering healthcare to remote communities in Fiji
In early April 2020, the all too familiar destruction of a Tropical Cyclone (TC) – Harold – hit the Solomon Islands, Vanuatu, Fiji and Tonga. One of the worst affected areas was the Eastern part of Fiji. Through support by Department of Foreign Affairs and Trade (DFAT), our Member Association, Reproductive and Family Health Association of Fiji (RFHAF), was quick to respond ensuring access to essential sexual and reproductive healthcare for Kadavu’s women, girls, and vulnerable groups. Fiji's vulnerable coastline Fiji’s worst affected area was the Eastern part, with TC Harold bringing destructive storm force winds and storm surge. RFHAF focused its humanitarian response on the local Kadavu population. This remote area proves a challenge to reach for the team with supplies. Share on Twitter Share on Facebook Share via WhatsApp Share via Email RFHAF's humanitarian response team tackle rough terrain National travel restrictions - due to the current COVID-19 pandemic - on all inter island transfers has slowed the response in some areas, including Kadavu. The island of Kadavu is one of the least developed areas of Fiji, the main source of income is substance living (Yaqona). Transport around the island is difficult, with very few roads, no public water system or electricity. The humanitarian team from RFHAF travels by boat and then on foot. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Asenaca, client Kadavu, the biggest island in the Eastern division has the greatest population (10,897). 197 evacuation centres were activated in total, initially hosting over 6,240 people. Many are women of reproductive age, with an estimated 150 currently pregnant. Asenaca learns about breast cancer self-checks from RFHAF’s healthcare provider, Karo. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Nasi, RFHAF healthcare provider The medical mobile team deliver a broad range of healthcare including contraception, information and counselling on sexual health, pregnancy, HIV and STI care and testing. RFHAF Team in Kadavu performing general health checks after TC Harold. Nasi administers a HPV shot to a client. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Kate, client Young women and girls are at the heart of RFHAF’s healthcare provision. Kate walks home with her dignity kit after a health check at the mobile clinic. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Karo, RFHAF healthcare worker RFHAF offers sexual and reproductive healthcare as well as counselling, and referrals for follow up care. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Alidi, RFHAF healthcare worker The team ensures young people in the community are not forgotten and provide information and education on relationships and sexual health and rights. Alidi conducting a session with a local group of young people at Gasele, Kadavu.Photos ©IPPF/Rob Rickman/Fiji Share on Twitter Share on Facebook Share via WhatsApp Share via Email
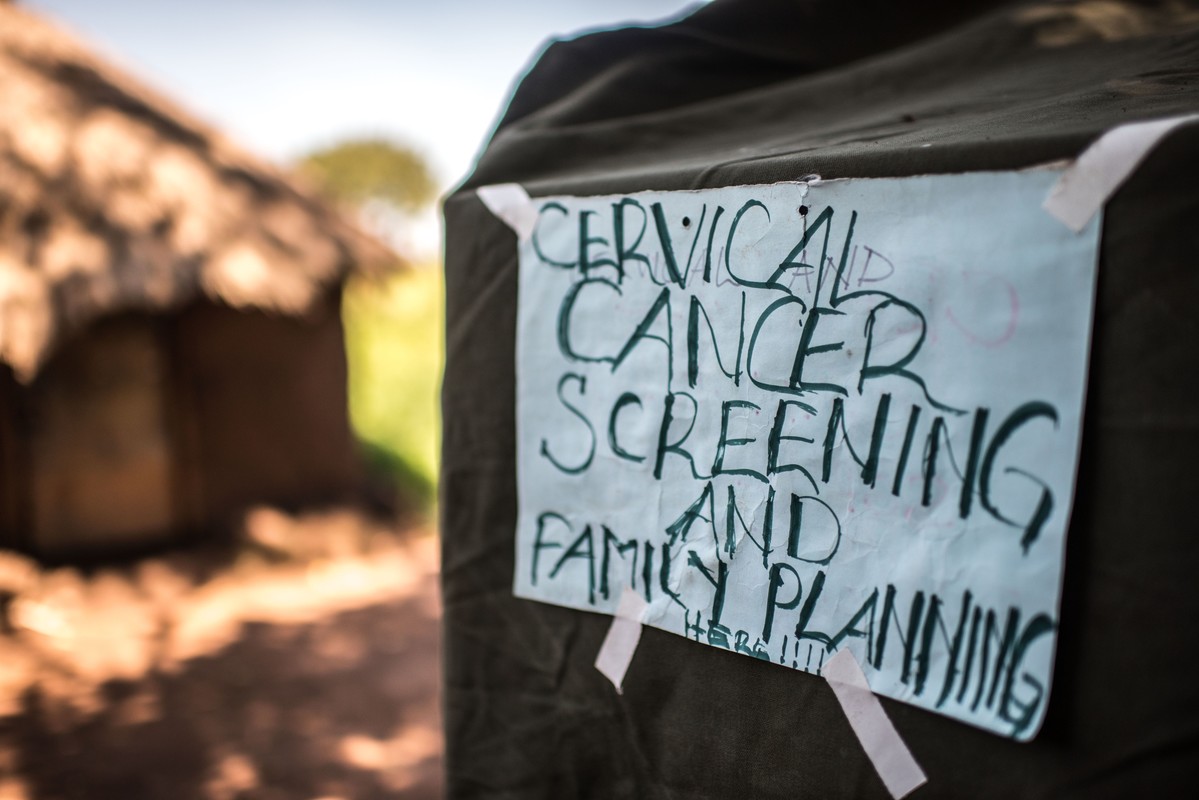
| 22 August 2018
“A radio announcement saved my life” – Gertrude’s story
Gertrude Mugala is a teacher in Fort Portal, a town in Western Uganda. While Gertrude considered herself fairly knowledgeable about cancer, she had never considered taking a screening test or imagined herself ever having the disease. Then one day, she heard an announcement on the radio urging women to go for cervical cancer screenings at a Reproductive Health Uganda (RHU) clinic. “The radio presenter was talking about cervical cancer, and in her message she encouraged all women to get screened. I decided to go and try it out,” she said. Gertrude made her way to RHU's Fort Portal Branch clinic for the free cervical cancer screening. There, she met Ms. Irene Kugonza, an RHU service provider. Ms. Kugonza educated Gertrude and a group of other women about cervical cancer and the importance of routine screening. Gertrude received a type of cervical cancer screening called VIA (visual inspection with acetic acid). "I did not know what was happening" But Gertrude's results were not what she expected; she received a positive result. The good news, however, is that precancerous lesions can be treated if detected early. “I was so shaken when I was told I had pre-cancerous lesions. I did not know what was happening and I didn't believe what I was hearing. I had no idea of my health status. I thought I was healthy, but I was actually harbouring a potential killer disease in me. What would have happened if I didn't go for the screening? If I hadn't heard the radio announcement?” Gertrude was then referred for cryotherapy. “Following cryotherapy, I am now in the process of healing, and I am supposed to go back for review after three months,” said Gertrude. Community screenings Today, Gertrude advocates for cervical cancer screening in her community. She talks to women about cancer, especially cervical cancer, at her workplace, at the market, in meetings, and any other opportunity she gets. “I decided to let women know that cervical cancer is real and it is here with us, and that it kills. At the moment, those are the platforms I have, and I will continue educating women about cancer and encourage them to go for routine testing. I am also happy that I was near my radio that day, where I heard that announcement encouraging all women to get tested for cervical cancer. It might be because of that radio announcement that I am here today,” she said.
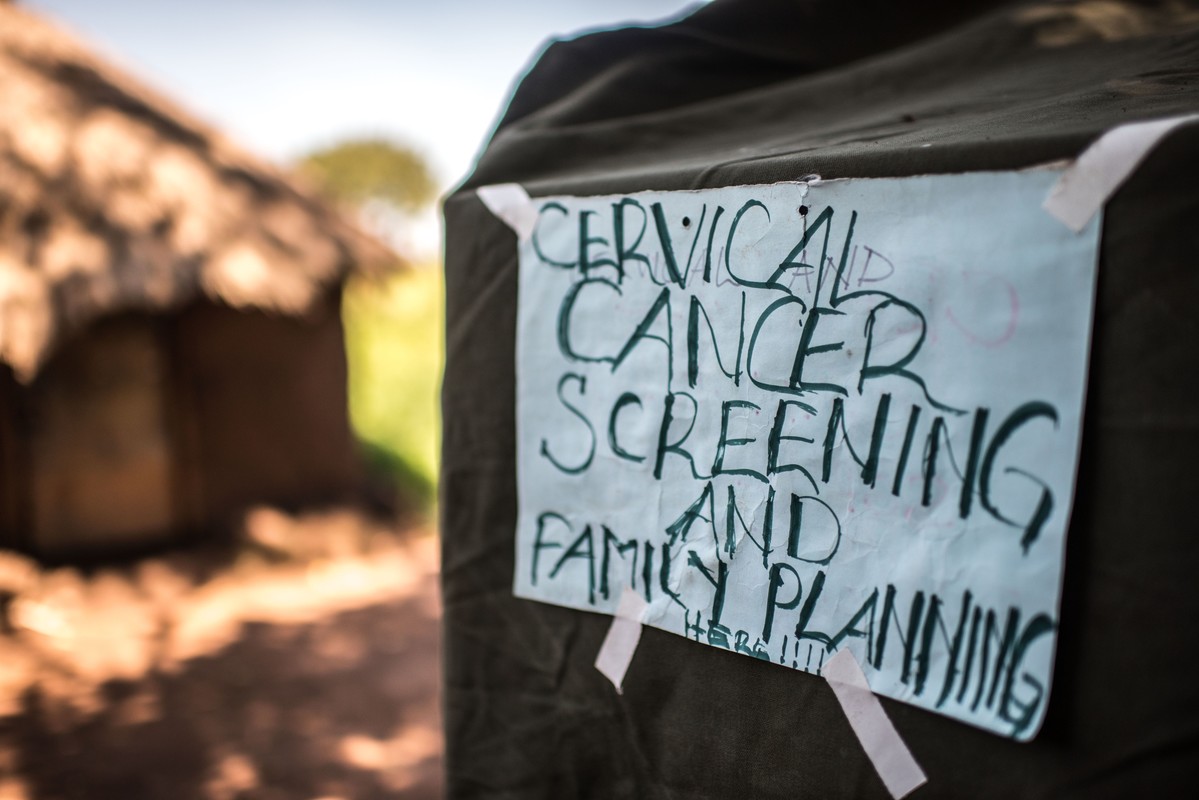
| 15 May 2025
“A radio announcement saved my life” – Gertrude’s story
Gertrude Mugala is a teacher in Fort Portal, a town in Western Uganda. While Gertrude considered herself fairly knowledgeable about cancer, she had never considered taking a screening test or imagined herself ever having the disease. Then one day, she heard an announcement on the radio urging women to go for cervical cancer screenings at a Reproductive Health Uganda (RHU) clinic. “The radio presenter was talking about cervical cancer, and in her message she encouraged all women to get screened. I decided to go and try it out,” she said. Gertrude made her way to RHU's Fort Portal Branch clinic for the free cervical cancer screening. There, she met Ms. Irene Kugonza, an RHU service provider. Ms. Kugonza educated Gertrude and a group of other women about cervical cancer and the importance of routine screening. Gertrude received a type of cervical cancer screening called VIA (visual inspection with acetic acid). "I did not know what was happening" But Gertrude's results were not what she expected; she received a positive result. The good news, however, is that precancerous lesions can be treated if detected early. “I was so shaken when I was told I had pre-cancerous lesions. I did not know what was happening and I didn't believe what I was hearing. I had no idea of my health status. I thought I was healthy, but I was actually harbouring a potential killer disease in me. What would have happened if I didn't go for the screening? If I hadn't heard the radio announcement?” Gertrude was then referred for cryotherapy. “Following cryotherapy, I am now in the process of healing, and I am supposed to go back for review after three months,” said Gertrude. Community screenings Today, Gertrude advocates for cervical cancer screening in her community. She talks to women about cancer, especially cervical cancer, at her workplace, at the market, in meetings, and any other opportunity she gets. “I decided to let women know that cervical cancer is real and it is here with us, and that it kills. At the moment, those are the platforms I have, and I will continue educating women about cancer and encourage them to go for routine testing. I am also happy that I was near my radio that day, where I heard that announcement encouraging all women to get tested for cervical cancer. It might be because of that radio announcement that I am here today,” she said.

| 21 May 2017
A graduate in need turns to sex work
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Lady Mermaid's Bureau. I am Pretty Lynn, aged 25. I am a sex worker but I went to university. I graduated with a Bachelor's Degree in Tourism in 2013. But now, during the day I’m sleeping and during the night I’m working. That is how my day goes every day. I got into sex work through friends. Okay it is not good but I am earning. I tried to get a job when I graduated. I have been applying since I graduated in 2013. I’m still applying but I’m not getting anywhere. You know to get jobs in Uganda; you have to know someone there and no one knows me there. To be a sex worker is like a curse. People look at you like, I don’t know, as someone that has no use in society. People look at you in a bad way. They even don’t consider why you are selling. They just see you as the worst thing that can happen in the society. So it is not comfortable, it is really hard but we try and survive. The fact sex working is illegal means you have to hide yourself when you are selling so that police cannot take you. And then you get diseases, men don’t want to pay. When the police come and take us, sometimes they even use us and don’t pay. So it is really hard. They want a free service. Like if they come and take you and pay that would be fair. But they say it is illegal to sell yourself. But they still use you yet they are saying it is illegal. You can’t report the police because there is no evidence. Abortion and unwanted pregnancies are really common because men don’t want to use condoms and female condoms are really rare and they are expensive. Though at times we get female condoms from Lady Marmaid’s Bureau (LMB) because there are so many of us they can’t keep on giving you them all the time. At times when we get pregnant we use local methods. You can go and use local herbs but it is not safe. One time I used local herbs and I was successful. Then the other time I used Omo washing powder and tea leaves but it was really hard for me. I almost died. I had a friend who died last year from this. But the good thing is that LMB taught us about safe abortion. I have had a safe abortion too. There are some tabs they are called Miso (misoprostol). It costs about fifty thousand shillings (£10 pounds or $20.) It is a lot of money. But if I’m working and I know I’m pregnant, I can say, "this week I’m working for my safe abortion". So if I’m working for twenty thousand, by the end of the week I will have the money. It is expensive compared to Omo at five hundred shillings but that is risky. So if I say I will work this whole week for Miso (misoprostol) it is better. But I'm working and I'm not eating. A project like this one from Lady Mermaid's can help young girls and women. But to take us from sex work, it would really be hard. They would not have enough money to cater for all of us. So what they have to do is to teach us how to protect ourselves, how to defend ourselves. Safe abortion yes. They will just have to sensitise us more about our lives, protection, female condoms and all that. I don't have a boyfriend but maybe when I get money and leave this job I will. But for now, no man would like a woman who sells. No man will bear the wife selling herself. And that will happen only if I get funds, settle somewhere else and become responsible woman. I don’t want this job. I don’t want to be in this business of sex work all the time. I want be married, with my children happily, not selling myself. Stories Read more stories about the amazing success of SAAF in Uganda

| 15 May 2025
A graduate in need turns to sex work
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Lady Mermaid's Bureau. I am Pretty Lynn, aged 25. I am a sex worker but I went to university. I graduated with a Bachelor's Degree in Tourism in 2013. But now, during the day I’m sleeping and during the night I’m working. That is how my day goes every day. I got into sex work through friends. Okay it is not good but I am earning. I tried to get a job when I graduated. I have been applying since I graduated in 2013. I’m still applying but I’m not getting anywhere. You know to get jobs in Uganda; you have to know someone there and no one knows me there. To be a sex worker is like a curse. People look at you like, I don’t know, as someone that has no use in society. People look at you in a bad way. They even don’t consider why you are selling. They just see you as the worst thing that can happen in the society. So it is not comfortable, it is really hard but we try and survive. The fact sex working is illegal means you have to hide yourself when you are selling so that police cannot take you. And then you get diseases, men don’t want to pay. When the police come and take us, sometimes they even use us and don’t pay. So it is really hard. They want a free service. Like if they come and take you and pay that would be fair. But they say it is illegal to sell yourself. But they still use you yet they are saying it is illegal. You can’t report the police because there is no evidence. Abortion and unwanted pregnancies are really common because men don’t want to use condoms and female condoms are really rare and they are expensive. Though at times we get female condoms from Lady Marmaid’s Bureau (LMB) because there are so many of us they can’t keep on giving you them all the time. At times when we get pregnant we use local methods. You can go and use local herbs but it is not safe. One time I used local herbs and I was successful. Then the other time I used Omo washing powder and tea leaves but it was really hard for me. I almost died. I had a friend who died last year from this. But the good thing is that LMB taught us about safe abortion. I have had a safe abortion too. There are some tabs they are called Miso (misoprostol). It costs about fifty thousand shillings (£10 pounds or $20.) It is a lot of money. But if I’m working and I know I’m pregnant, I can say, "this week I’m working for my safe abortion". So if I’m working for twenty thousand, by the end of the week I will have the money. It is expensive compared to Omo at five hundred shillings but that is risky. So if I say I will work this whole week for Miso (misoprostol) it is better. But I'm working and I'm not eating. A project like this one from Lady Mermaid's can help young girls and women. But to take us from sex work, it would really be hard. They would not have enough money to cater for all of us. So what they have to do is to teach us how to protect ourselves, how to defend ourselves. Safe abortion yes. They will just have to sensitise us more about our lives, protection, female condoms and all that. I don't have a boyfriend but maybe when I get money and leave this job I will. But for now, no man would like a woman who sells. No man will bear the wife selling herself. And that will happen only if I get funds, settle somewhere else and become responsible woman. I don’t want this job. I don’t want to be in this business of sex work all the time. I want be married, with my children happily, not selling myself. Stories Read more stories about the amazing success of SAAF in Uganda

| 20 May 2017
Working to stop unsafe abortion for school girls
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Volunteers for Development Association Uganda (VODA). Unsafe abortion is a huge problem in Uganda with an estimated 400,000 women having an unsafe abortion per year. The law is confusing and unclear, with abortion permitted only under certain circumstances. Post-abortion care is permitted to treat women who have undergone an unsafe abortion, however lack of awareness of the law and stigma surrounding abortion mean that service providers are not always willing to treat patients who arrive seeking care. The VODA project aims to ensure that young women in Uganda are able to lead healthier lives free from unsafe abortion related deaths or complications through reducing abortion stigma in the community, increasing access to abortion-related services and ensuring the providers are trained to provide quality post-abortion care services. I am Helen. I have been a midwife at this small clinic for seven years and I have worked with VODA for four years. Unsafe abortion continues and some schoolgirls are raped. They then go to local herbalists and some of them tell me that they are given emilandira [roots] which they insert inside themselves to rupture the membranes. Some of them even try to induce an abortion by using Omo [douching with detergent or bleach]. At the end of the day they get complications then they land here, so we help them. Unsafe abortion is very common. In one month you can get more than five cases. It is a big problem. We help them, they need to go back to school, and we counsel them. If it is less than 12 weeks, we handle them from here. If they are more than 12 weeks along we refer them to the hospital. Most referrals from VODA are related to unwanted pregnancies, HIV testing, family planning, and youth friendly services. A few parents come for services for their children who are at school. So we counsel them that contraception, other than condoms, will only prevent pregnancy, but you can still get HIV and STIs, so take care. I am Josephine and I work as a midwife at a rural health centre. I deal with pregnant mothers, postnatal mothers, and there are girls who come with problems like unwanted pregnancy. I used to have a negative attitude towards abortion. But then VODA helped us understand the importance of helping someone with the problem because many people were dying in the villages because of unsafe abortion. According to my religion, helping someone to have an abortion was not allowed. But again when you look into it, it’s not good to leave someone to die. So I decided to change my attitude to help people. Post-abortion care has helped many people because these days we don’t have many people in the villages dying because of unsafe abortion. These days I’m proud of what we are doing because before I didn’t know the importance of helping someone with a problem. But these days, since people no longer die, people no longer get problems and I’m proud and happy because we help so many people. My name is Jonathan. I am married with three children. I have a Bachelor of Social Work and Social Administration. I have worked with VODA as a project officer since 2008. Due to the training that we have done about abortion many people have changed their attitudes and we have helped people to talk about the issue. Most people were against abortion before but they are now realising that if it’s done safely it is important because otherwise many people die from unsafe abortion. I have talked to religious leaders, I have talked to local leaders; I have talked to people of different categories. At first when you approach them, they have a different perception. The health workers were difficult to work with at first. However they knew people were approaching them with the problems of unsafe abortion. Due to religion, communities can be hard against this issue. But after some time we have seen that they have changed their perception toward the issue of safe and unsafe abortion. And now many of them know that in some instances, abortion is inevitable but it should be done in a safe way. I’m Stevens and I am nurse. We have some clients who come when they have already attempted an unsafe abortion. You find that it is often inevitable. The only solution you have to help those clients is to provide treatment of incomplete abortion as part of post-abortion care. Because of the VODA project there is a very remarkable change in the community. Now, those people who used to have unsafe abortions locally, know where to go for post-abortion care - unlike in the past. I remember a schoolgirl, she was in a very sorry state because she had tried some local remedies to abort. I attended to her and things went well. She went back to school. I feel so proud because that was a big life rescue. A girl like that could have died but now she is alive and I see her carrying on with her studies, I feel so proud. I praise VODA for that encouragement. This service should be legalised because whether they restrict it or not, there is abortion and it is going on. And if it’s not out in the open, so that our people know where to go for such services, it leads to more deaths. Stories Read more stories about the amazing success of SAAF in Uganda

| 15 May 2025
Working to stop unsafe abortion for school girls
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Volunteers for Development Association Uganda (VODA). Unsafe abortion is a huge problem in Uganda with an estimated 400,000 women having an unsafe abortion per year. The law is confusing and unclear, with abortion permitted only under certain circumstances. Post-abortion care is permitted to treat women who have undergone an unsafe abortion, however lack of awareness of the law and stigma surrounding abortion mean that service providers are not always willing to treat patients who arrive seeking care. The VODA project aims to ensure that young women in Uganda are able to lead healthier lives free from unsafe abortion related deaths or complications through reducing abortion stigma in the community, increasing access to abortion-related services and ensuring the providers are trained to provide quality post-abortion care services. I am Helen. I have been a midwife at this small clinic for seven years and I have worked with VODA for four years. Unsafe abortion continues and some schoolgirls are raped. They then go to local herbalists and some of them tell me that they are given emilandira [roots] which they insert inside themselves to rupture the membranes. Some of them even try to induce an abortion by using Omo [douching with detergent or bleach]. At the end of the day they get complications then they land here, so we help them. Unsafe abortion is very common. In one month you can get more than five cases. It is a big problem. We help them, they need to go back to school, and we counsel them. If it is less than 12 weeks, we handle them from here. If they are more than 12 weeks along we refer them to the hospital. Most referrals from VODA are related to unwanted pregnancies, HIV testing, family planning, and youth friendly services. A few parents come for services for their children who are at school. So we counsel them that contraception, other than condoms, will only prevent pregnancy, but you can still get HIV and STIs, so take care. I am Josephine and I work as a midwife at a rural health centre. I deal with pregnant mothers, postnatal mothers, and there are girls who come with problems like unwanted pregnancy. I used to have a negative attitude towards abortion. But then VODA helped us understand the importance of helping someone with the problem because many people were dying in the villages because of unsafe abortion. According to my religion, helping someone to have an abortion was not allowed. But again when you look into it, it’s not good to leave someone to die. So I decided to change my attitude to help people. Post-abortion care has helped many people because these days we don’t have many people in the villages dying because of unsafe abortion. These days I’m proud of what we are doing because before I didn’t know the importance of helping someone with a problem. But these days, since people no longer die, people no longer get problems and I’m proud and happy because we help so many people. My name is Jonathan. I am married with three children. I have a Bachelor of Social Work and Social Administration. I have worked with VODA as a project officer since 2008. Due to the training that we have done about abortion many people have changed their attitudes and we have helped people to talk about the issue. Most people were against abortion before but they are now realising that if it’s done safely it is important because otherwise many people die from unsafe abortion. I have talked to religious leaders, I have talked to local leaders; I have talked to people of different categories. At first when you approach them, they have a different perception. The health workers were difficult to work with at first. However they knew people were approaching them with the problems of unsafe abortion. Due to religion, communities can be hard against this issue. But after some time we have seen that they have changed their perception toward the issue of safe and unsafe abortion. And now many of them know that in some instances, abortion is inevitable but it should be done in a safe way. I’m Stevens and I am nurse. We have some clients who come when they have already attempted an unsafe abortion. You find that it is often inevitable. The only solution you have to help those clients is to provide treatment of incomplete abortion as part of post-abortion care. Because of the VODA project there is a very remarkable change in the community. Now, those people who used to have unsafe abortions locally, know where to go for post-abortion care - unlike in the past. I remember a schoolgirl, she was in a very sorry state because she had tried some local remedies to abort. I attended to her and things went well. She went back to school. I feel so proud because that was a big life rescue. A girl like that could have died but now she is alive and I see her carrying on with her studies, I feel so proud. I praise VODA for that encouragement. This service should be legalised because whether they restrict it or not, there is abortion and it is going on. And if it’s not out in the open, so that our people know where to go for such services, it leads to more deaths. Stories Read more stories about the amazing success of SAAF in Uganda

| 20 May 2017
A mother's heart break after losing teen daughter to unsafe abortion
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Volunteers for Development Association Uganda (VODA). Margaret's daughter, Gladys, was raped by a relative as a teenager and became pregnant. She did not tell her mother what had happened and not wanting to have a child at such a young age conceived through incest, Gladys tried to terminate the pregnancy herself using local herbs but got an infection and died. "My name is Margaret and I am a widow." "I lost my daughter in 2011. She was called Gladys and she was 16. I didn’t know that she was pregnant. She tried to use local herbs to abort. I only found out about it three days later when she was bleeding very heavily. I tried to take her to the hospital but unfortunately she died on the way." Despite being the cause of many deaths in the region, the stigma surrounding abortion means that most people do not mention the cause of death publically. However at Gladys' funeral one of her school friends spoke out and said that she had died due to unsafe abortion. This prompted VODA to start working on the issue and when the project started they included Margaret in their training on how to prevent unsafe abortion. "The training made me stronger to talk about it. Now, I continue to tell my remaining two girls about the dangers of unsafe abortion, sexually transmitted infections and unwanted pregnancies. VODA has really helped us. I think my girl wouldn’t have died if VODA was active then like it is now." "I have used VODA's information to carry on with my parental work. That information has been helpful because we are noticing change. I keep on reminding them, 'didn’t you see what happened to your friend here?'. So they have really changed especially with the ongoing help of the people from VODA." "Unsafe abortion was rampant in the past. We had tried to speak to the students, as parents, but it seemed that our information was not enough. But now we have another helping hand from VODA, especially with those seminars targeting the girls." Stories Read more stories about the amazing success of SAAF in Uganda

| 15 May 2025
A mother's heart break after losing teen daughter to unsafe abortion
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Volunteers for Development Association Uganda (VODA). Margaret's daughter, Gladys, was raped by a relative as a teenager and became pregnant. She did not tell her mother what had happened and not wanting to have a child at such a young age conceived through incest, Gladys tried to terminate the pregnancy herself using local herbs but got an infection and died. "My name is Margaret and I am a widow." "I lost my daughter in 2011. She was called Gladys and she was 16. I didn’t know that she was pregnant. She tried to use local herbs to abort. I only found out about it three days later when she was bleeding very heavily. I tried to take her to the hospital but unfortunately she died on the way." Despite being the cause of many deaths in the region, the stigma surrounding abortion means that most people do not mention the cause of death publically. However at Gladys' funeral one of her school friends spoke out and said that she had died due to unsafe abortion. This prompted VODA to start working on the issue and when the project started they included Margaret in their training on how to prevent unsafe abortion. "The training made me stronger to talk about it. Now, I continue to tell my remaining two girls about the dangers of unsafe abortion, sexually transmitted infections and unwanted pregnancies. VODA has really helped us. I think my girl wouldn’t have died if VODA was active then like it is now." "I have used VODA's information to carry on with my parental work. That information has been helpful because we are noticing change. I keep on reminding them, 'didn’t you see what happened to your friend here?'. So they have really changed especially with the ongoing help of the people from VODA." "Unsafe abortion was rampant in the past. We had tried to speak to the students, as parents, but it seemed that our information was not enough. But now we have another helping hand from VODA, especially with those seminars targeting the girls." Stories Read more stories about the amazing success of SAAF in Uganda

| 20 May 2017
Educating their peers about unsafe abortion
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grassroots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Volunteers for Development Association Uganda (VODA). Peer educators in schools provide counselling and advice to other students, who otherwise would have no one to turn to in times of crisis. Today, we have the largest generation of young people ever, each one with their own unique needs. Peer educators are critical in gaining the trust and confidence of hundreds of young girls each term, and together they help each other gain more knowledge about their sexual and reproductive health. Peer educators themselves also gain a great deal from the training and experience and VODA has been successful in empowering many of these young girls to feel confident and be able to talk out in public, something that they were not able to do before. Poverty, gender inequality, lack of knowledge about sex and relationships and lack of access to sanitary protection mean that girls in rural Uganda are at high risk of sexual exploitation and abuse. All of this coupled with very little access to contraception means that Uganda has high rates of unintended pregnancies among young girls. Despite abortion being legal in Uganda in cases of rape and incest, most girls are not aware of the law and resort to unsafe abortion often using local herbs or washing liquid. The peer educators trained by VODA are able to listen to other young people's issues and provide support and information a range of issues including safe abortion as well as how to access contraception. My name is Mabel. I am in my final year of O'Levels and I am a peer counsellor at a Secondary School in Namuganga. I was selected with two others by VODA and my head teacher, and then trained to be a peer counsellor. We were trained to help our colleagues at school to handle various problems. Girls used to get pregnant and some were dropping out of school. So we counselled many of our colleagues about unwanted pregnancies. We have seen a change because we get free condoms from VODA. We could preach abstinence from sex. For those that could not manage abstinence, we could give them male condoms. Unsafe abortion has been a big problem. Girls were using local herbs and sharp instruments like metallic hangers for abortion. Many would get injured and some would die. I remember last year there was a girl who aborted using those local methods but she died and was buried in Seeta. If VODA wasn't here I think things would be very bad because as students, we did not have access to most of the information that we needed. We would have seen a big number of girls out of school because of unwanted pregnancies or unsafe abortion. I have benefited a lot. I have acquired information which I have used to keep myself safe in terms of unwanted pregnancies. I don’t think I could ever be lured to perform unsafe abortion because I know the risks. In the past, I wasn't able to speak in public but now I can stand and talk freely. I’m Sharon and I’m a student counsellor at a Secondary School in Namuganga. I counsel fellow students, young people in communities and even adults. Before I was selected for VODA training I thought it was just an organisation to promote abortion. But then I realised they were addressing a big problem that was happening at our school and our villages. I have learnt that when someone gets pregnant I don’t have to force her to abort and I don’t encourage her to go for unsafe abortion. If we hear that a certain girl has a boyfriend, we approach her and counsel her on issues like unwanted pregnancy. Many young girls have been lured into early sex because they need money, which is why we end up with unwanted pregnancies. In a bid to fulfil those needs, they get boyfriends or other guys who use them for money, impregnate them and then leave. The girls know about contraceptives like the pill and we have given some of them referral cards for them to access the contraceptives from the health centres. But there has been debate against giving young girls contraceptives. There are restrictions that the government puts in place but that does not mean that girls are not getting pregnant. I remember the girls who died after aborting through unsafe abortion methods and I think about the lives that would have been saved if they had knowledge about contraceptives. I’m Rita and I’m 15-years-old. I was twelve when I was selected to be a VODA counsellor in my primary school. I was lucky because many people wanted to be counsellors but I was chosen. My parents were very happy and they got interested. When I joined this school, I introduced myself to other students because I wanted to continue with my work as a counsellor. I told my colleagues to feel free to share with me their issues. We are lucky here because there are many counsellors. Girls are having unwanted pregnancies because they are lured by men who give them presents and things such as money for sanitary pads that they cannot get from their parents. Before I joined this school, there were many cases of girls terminating pregnancies with unsafe abortions. It was common to hear of or see someone who had aborted. Many would abort so that they would return to school. When I joined this school last year and we intensified the counselling sessions, many came and shared their problems with us. We have learnt that two girls at school gave birth and have since returned to school but we have not had cases of unsafe abortions here since I joined. I wasn’t as serious with studies before I became a counsellor but because I want to maintain my status, I have improved in my studies because I don’t want to feel ashamed in front of my fellow students. VODA gave us T-shirts for identification purposes which has made people in the community respect me as well. In terms of preventing unwanted pregnancies in schools, most of what we see here originates from the girls' homes. Many parents don’t provide for the girls’ necessities (like sanitary towels) so that makes them vulnerable to be lured by men. Stories Read more stories about the amazing success of SAAF in Uganda

| 15 May 2025
Educating their peers about unsafe abortion
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grassroots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Volunteers for Development Association Uganda (VODA). Peer educators in schools provide counselling and advice to other students, who otherwise would have no one to turn to in times of crisis. Today, we have the largest generation of young people ever, each one with their own unique needs. Peer educators are critical in gaining the trust and confidence of hundreds of young girls each term, and together they help each other gain more knowledge about their sexual and reproductive health. Peer educators themselves also gain a great deal from the training and experience and VODA has been successful in empowering many of these young girls to feel confident and be able to talk out in public, something that they were not able to do before. Poverty, gender inequality, lack of knowledge about sex and relationships and lack of access to sanitary protection mean that girls in rural Uganda are at high risk of sexual exploitation and abuse. All of this coupled with very little access to contraception means that Uganda has high rates of unintended pregnancies among young girls. Despite abortion being legal in Uganda in cases of rape and incest, most girls are not aware of the law and resort to unsafe abortion often using local herbs or washing liquid. The peer educators trained by VODA are able to listen to other young people's issues and provide support and information a range of issues including safe abortion as well as how to access contraception. My name is Mabel. I am in my final year of O'Levels and I am a peer counsellor at a Secondary School in Namuganga. I was selected with two others by VODA and my head teacher, and then trained to be a peer counsellor. We were trained to help our colleagues at school to handle various problems. Girls used to get pregnant and some were dropping out of school. So we counselled many of our colleagues about unwanted pregnancies. We have seen a change because we get free condoms from VODA. We could preach abstinence from sex. For those that could not manage abstinence, we could give them male condoms. Unsafe abortion has been a big problem. Girls were using local herbs and sharp instruments like metallic hangers for abortion. Many would get injured and some would die. I remember last year there was a girl who aborted using those local methods but she died and was buried in Seeta. If VODA wasn't here I think things would be very bad because as students, we did not have access to most of the information that we needed. We would have seen a big number of girls out of school because of unwanted pregnancies or unsafe abortion. I have benefited a lot. I have acquired information which I have used to keep myself safe in terms of unwanted pregnancies. I don’t think I could ever be lured to perform unsafe abortion because I know the risks. In the past, I wasn't able to speak in public but now I can stand and talk freely. I’m Sharon and I’m a student counsellor at a Secondary School in Namuganga. I counsel fellow students, young people in communities and even adults. Before I was selected for VODA training I thought it was just an organisation to promote abortion. But then I realised they were addressing a big problem that was happening at our school and our villages. I have learnt that when someone gets pregnant I don’t have to force her to abort and I don’t encourage her to go for unsafe abortion. If we hear that a certain girl has a boyfriend, we approach her and counsel her on issues like unwanted pregnancy. Many young girls have been lured into early sex because they need money, which is why we end up with unwanted pregnancies. In a bid to fulfil those needs, they get boyfriends or other guys who use them for money, impregnate them and then leave. The girls know about contraceptives like the pill and we have given some of them referral cards for them to access the contraceptives from the health centres. But there has been debate against giving young girls contraceptives. There are restrictions that the government puts in place but that does not mean that girls are not getting pregnant. I remember the girls who died after aborting through unsafe abortion methods and I think about the lives that would have been saved if they had knowledge about contraceptives. I’m Rita and I’m 15-years-old. I was twelve when I was selected to be a VODA counsellor in my primary school. I was lucky because many people wanted to be counsellors but I was chosen. My parents were very happy and they got interested. When I joined this school, I introduced myself to other students because I wanted to continue with my work as a counsellor. I told my colleagues to feel free to share with me their issues. We are lucky here because there are many counsellors. Girls are having unwanted pregnancies because they are lured by men who give them presents and things such as money for sanitary pads that they cannot get from their parents. Before I joined this school, there were many cases of girls terminating pregnancies with unsafe abortions. It was common to hear of or see someone who had aborted. Many would abort so that they would return to school. When I joined this school last year and we intensified the counselling sessions, many came and shared their problems with us. We have learnt that two girls at school gave birth and have since returned to school but we have not had cases of unsafe abortions here since I joined. I wasn’t as serious with studies before I became a counsellor but because I want to maintain my status, I have improved in my studies because I don’t want to feel ashamed in front of my fellow students. VODA gave us T-shirts for identification purposes which has made people in the community respect me as well. In terms of preventing unwanted pregnancies in schools, most of what we see here originates from the girls' homes. Many parents don’t provide for the girls’ necessities (like sanitary towels) so that makes them vulnerable to be lured by men. Stories Read more stories about the amazing success of SAAF in Uganda

| 20 May 2017
Post-abortion care for straight-A student
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was a fund set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such project which received funding is called Volunteers for Development Association Uganda (VODA). My name is Anne*, I am 14-years-old, I am a student at one of the local schools near my (rural) village. I recently went to the health centre for post-abortion care. I was referred there by VODA and I was helped by the mid-wife, her name was Grace. The VODA community volunteers, they found me at my grandmother's house. They brought me to the health centre. I was on my way to visit my grandmother. A man just caught me. After he finished with me he told me to go back home and never to tell anyone about it. I went back home to my parents, in Luwero District. There is no VODA there. I realised I was pregnant because I found out I had missed my periods. Then I told my mother. My mother said we should try to do something about the pregnancy, but not in our home district, otherwise my father would not longer pay my school fees. I had just finished my Primary Leaving Examinations and I was looking forward to joining secondary. So then I had to go back to my grandmother's house. She said we were going to the hospital but it wasn't like the one where Grace works, where I finally got my post-abortion treatment. She took me to a place where a woman gave me some herbs. Then we went home and the thing came out. I was bleeding. Then the VODA counsellor came to my home and suggested to my grandmother that I should be taken for treatment. I had learnt about how girls can get pregnant but I didn't know anything about safe abortion. In Luwero, where I come from, many girls I hear they use herbs to abort but I had not tried it because I had not had any sex until that man forced me. I am telling my friends about safe abortion and contraceptive services but I also need to be given more information about it because I was not taught about most of what Grace the midwife was telling me. I know that women can take precautions for family planning like pills but my mum told me it's only for married people. I am very thankful to VODA, I maybe could have died if the counsellors from VODA hadn't asked to rush me to the health centre for post-abortion care. *Not her real name Stories Read more stories about the amazing success of SAAF in Uganda

| 15 May 2025
Post-abortion care for straight-A student
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was a fund set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such project which received funding is called Volunteers for Development Association Uganda (VODA). My name is Anne*, I am 14-years-old, I am a student at one of the local schools near my (rural) village. I recently went to the health centre for post-abortion care. I was referred there by VODA and I was helped by the mid-wife, her name was Grace. The VODA community volunteers, they found me at my grandmother's house. They brought me to the health centre. I was on my way to visit my grandmother. A man just caught me. After he finished with me he told me to go back home and never to tell anyone about it. I went back home to my parents, in Luwero District. There is no VODA there. I realised I was pregnant because I found out I had missed my periods. Then I told my mother. My mother said we should try to do something about the pregnancy, but not in our home district, otherwise my father would not longer pay my school fees. I had just finished my Primary Leaving Examinations and I was looking forward to joining secondary. So then I had to go back to my grandmother's house. She said we were going to the hospital but it wasn't like the one where Grace works, where I finally got my post-abortion treatment. She took me to a place where a woman gave me some herbs. Then we went home and the thing came out. I was bleeding. Then the VODA counsellor came to my home and suggested to my grandmother that I should be taken for treatment. I had learnt about how girls can get pregnant but I didn't know anything about safe abortion. In Luwero, where I come from, many girls I hear they use herbs to abort but I had not tried it because I had not had any sex until that man forced me. I am telling my friends about safe abortion and contraceptive services but I also need to be given more information about it because I was not taught about most of what Grace the midwife was telling me. I know that women can take precautions for family planning like pills but my mum told me it's only for married people. I am very thankful to VODA, I maybe could have died if the counsellors from VODA hadn't asked to rush me to the health centre for post-abortion care. *Not her real name Stories Read more stories about the amazing success of SAAF in Uganda

| 20 May 2017
Tackling taboos about abortion
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Volunteers for Development Association Uganda (VODA). Teachers and community volunteers provide support for young people in schools. They are critical in reshaping the social norms and stigma surrounding teen pregnancies. For many young girls, an unwanted pregnancy can limit their education and significantly restrict their life options. In Uganda, teachers are now helping to provide counselling for girls on contraception and safe abortion. Prior to VODA working with schools to provide teachers with training, the rate of deaths from unsafe abortion was significantly high. This was even the case in primary schools. Now the prevalence of unwanted pregnancies has dropped and girls are more aware of their sexual and reproductive health. I’m Deborah. I’m 27-years-old and I'm a teacher as well as being a community volunteer with VODA Uganda. There is a problem with unsafe abortion and teenage pregnancies in this area. Young girls have been getting pregnant and some of them have been dropping out of school. Some have even died because of unsafe abortions. When VODA came in, they taught us about teenage pregnancies and unsafe abortion. So we came in to teach young people in the villages so that they can be aware of these issues. Many girls secretly use injectable contraceptives after being told to do so by their parents. When these parents realise that their daughters are sexually active, they fear that they could get pregnant before they complete school. They do it secretly because they fear stigma. They do it that way to avoid rumours that may circulate if they know that one’s daughter was taken for family planning while she is still at school. Many people in our community think that a teenager who is on contraceptives is spoilt. When I had just come to this area, incidents of unsafe abortion were high. But when I began working here and the girls came to know about me, I began counselling them about safe sex, contraceptives and condoms. I told them that if you think you cannot have protected sex, then you need to use contraceptives. But we also warned them against sexually transmitted infections. Using contraception has reduced the number of girls engaging in unsafe abortion. There are different local methods used to abort. Some of them would get complications that needed medical attention after trying these methods. Some would also secretly try to go to health centres after the abortion had gone wrongly or they had even nearly died. Now some of those that have unwanted pregnancies do approach me and I counsel them. In the past, if one talked about abortion or unwanted pregnancies, I would harshly judge her saying that she wanted it. But having become a volunteer with VODA I have learned sometimes the pregnancies are due to defilement or rape, so I came to understand that not all those that get pregnant want to have a child. Sometimes abortion is inevitable. For example, when a girl has been raped by her father, uncle, brothers or close relatives. How would a girl carry that baby? It is very important to educate young people about unsafe abortion, especially when they have reached that stage when they can get pregnant. That will help them to prevent having unwanted pregnancies and also to avoid unsafe abortion. It is important to give young girls contraceptives because some will have premarital sex. So such girls must have contraceptives if they are to avoid getting pregnant. I am Mily and I am 38-years-old. I am a volunteer for VODA Uganda and a teacher at a primary school in Kasawo. I have been teaching here for eight years. Before VODA was here, there were a lot of school dropouts from girls. They were getting unwanted pregnancies whereby they were forced to leave school. There was no one to counsel them. They were using local medicines for unsafe abortion. But when VODA came in they started to advise about unsafe abortion. We are working together with doctors and nurses from various hospitals so girls could get good care. VODA workers approached us and explained how it could help our children to stay in school. Then we had a workshop and our head teacher selected who would manage this. Before VODA came in unsafe abortion was rampant. Many of the girls were dying. Here at this school we had a girl in P4 - we were not even expecting that girl could be pregnant. Unfortunately, we heard about it when the girl was already dead. She was trying to have an unsafe abortion. Before VODA came, there was no sexuality education or counselling to do with STIs. That is why our children were dying because they feared to tell their parents. We thought that pregnant girls should leave school without further assistance. But as a volunteer, I thank VODA because now I know that that girls can be helped and they can continue with their studies. I am Frida and I'm 18-years-old. I am a peer counsellor at school and have counselled many girls about unsafe abortion. I came to know about VODA on a careers day at school and by attending training workshops on unsafe abortion. At our school, I’m very well-known as a youth counsellor. I help other girls who are sexually active with unwanted pregnancies. The training I received from VODA has given me self-confidence. Before, I couldn’t stand in public. But now I can stand in the presence of even one thousand people and I can talk. I’m not shy anymore. The problems are that girls can't access services like post-abortion care and family planning, like the pill. Girls are poor. Some services need money yet some girls don’t have money. They are getting pregnant because they have less information about unprotected sex and they are sexually active. To help them there needs to be places where they can find such services. From my training with VODA I now want to be a social worker so that I can work with people. I have realised that I can handle people well. Stories Read more stories about the amazing success of SAAF in Uganda

| 15 May 2025
Tackling taboos about abortion
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Volunteers for Development Association Uganda (VODA). Teachers and community volunteers provide support for young people in schools. They are critical in reshaping the social norms and stigma surrounding teen pregnancies. For many young girls, an unwanted pregnancy can limit their education and significantly restrict their life options. In Uganda, teachers are now helping to provide counselling for girls on contraception and safe abortion. Prior to VODA working with schools to provide teachers with training, the rate of deaths from unsafe abortion was significantly high. This was even the case in primary schools. Now the prevalence of unwanted pregnancies has dropped and girls are more aware of their sexual and reproductive health. I’m Deborah. I’m 27-years-old and I'm a teacher as well as being a community volunteer with VODA Uganda. There is a problem with unsafe abortion and teenage pregnancies in this area. Young girls have been getting pregnant and some of them have been dropping out of school. Some have even died because of unsafe abortions. When VODA came in, they taught us about teenage pregnancies and unsafe abortion. So we came in to teach young people in the villages so that they can be aware of these issues. Many girls secretly use injectable contraceptives after being told to do so by their parents. When these parents realise that their daughters are sexually active, they fear that they could get pregnant before they complete school. They do it secretly because they fear stigma. They do it that way to avoid rumours that may circulate if they know that one’s daughter was taken for family planning while she is still at school. Many people in our community think that a teenager who is on contraceptives is spoilt. When I had just come to this area, incidents of unsafe abortion were high. But when I began working here and the girls came to know about me, I began counselling them about safe sex, contraceptives and condoms. I told them that if you think you cannot have protected sex, then you need to use contraceptives. But we also warned them against sexually transmitted infections. Using contraception has reduced the number of girls engaging in unsafe abortion. There are different local methods used to abort. Some of them would get complications that needed medical attention after trying these methods. Some would also secretly try to go to health centres after the abortion had gone wrongly or they had even nearly died. Now some of those that have unwanted pregnancies do approach me and I counsel them. In the past, if one talked about abortion or unwanted pregnancies, I would harshly judge her saying that she wanted it. But having become a volunteer with VODA I have learned sometimes the pregnancies are due to defilement or rape, so I came to understand that not all those that get pregnant want to have a child. Sometimes abortion is inevitable. For example, when a girl has been raped by her father, uncle, brothers or close relatives. How would a girl carry that baby? It is very important to educate young people about unsafe abortion, especially when they have reached that stage when they can get pregnant. That will help them to prevent having unwanted pregnancies and also to avoid unsafe abortion. It is important to give young girls contraceptives because some will have premarital sex. So such girls must have contraceptives if they are to avoid getting pregnant. I am Mily and I am 38-years-old. I am a volunteer for VODA Uganda and a teacher at a primary school in Kasawo. I have been teaching here for eight years. Before VODA was here, there were a lot of school dropouts from girls. They were getting unwanted pregnancies whereby they were forced to leave school. There was no one to counsel them. They were using local medicines for unsafe abortion. But when VODA came in they started to advise about unsafe abortion. We are working together with doctors and nurses from various hospitals so girls could get good care. VODA workers approached us and explained how it could help our children to stay in school. Then we had a workshop and our head teacher selected who would manage this. Before VODA came in unsafe abortion was rampant. Many of the girls were dying. Here at this school we had a girl in P4 - we were not even expecting that girl could be pregnant. Unfortunately, we heard about it when the girl was already dead. She was trying to have an unsafe abortion. Before VODA came, there was no sexuality education or counselling to do with STIs. That is why our children were dying because they feared to tell their parents. We thought that pregnant girls should leave school without further assistance. But as a volunteer, I thank VODA because now I know that that girls can be helped and they can continue with their studies. I am Frida and I'm 18-years-old. I am a peer counsellor at school and have counselled many girls about unsafe abortion. I came to know about VODA on a careers day at school and by attending training workshops on unsafe abortion. At our school, I’m very well-known as a youth counsellor. I help other girls who are sexually active with unwanted pregnancies. The training I received from VODA has given me self-confidence. Before, I couldn’t stand in public. But now I can stand in the presence of even one thousand people and I can talk. I’m not shy anymore. The problems are that girls can't access services like post-abortion care and family planning, like the pill. Girls are poor. Some services need money yet some girls don’t have money. They are getting pregnant because they have less information about unprotected sex and they are sexually active. To help them there needs to be places where they can find such services. From my training with VODA I now want to be a social worker so that I can work with people. I have realised that I can handle people well. Stories Read more stories about the amazing success of SAAF in Uganda