
Every day some 830 women die from causes related to pregnancy or childbirth. Many more have serious injuries or long-lasting consequences.
IPPF works around the world to improve maternal health through our clinics and outreach services and by training health workers, improving the availability of essential medicines and strengthening health systems.
Articles by Maternal Healthcare
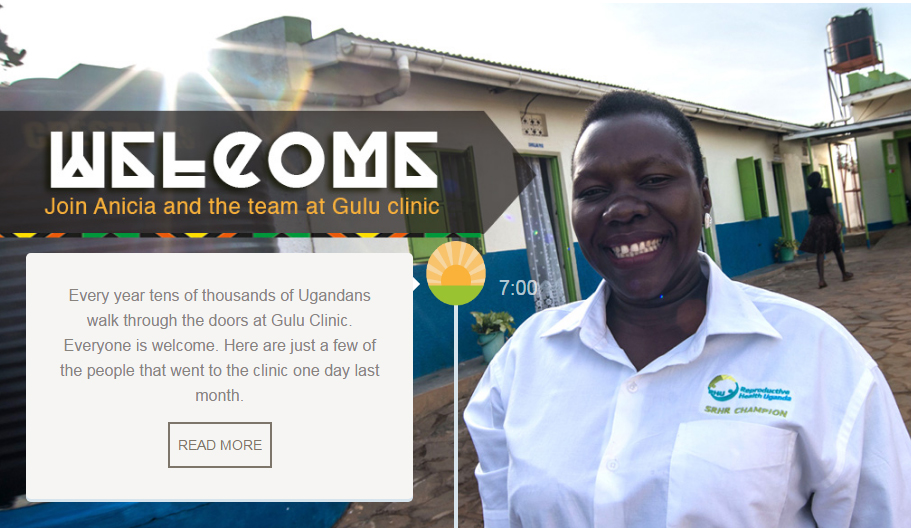
The mother of six struggling with sickle cell
Lillian Lamunu and her husband are both out of work and are struggling to look after their six children who all have Sickle Cell Disease. Lillian is worried that if she doesn’t do something soon she might end up having another baby. She spoke to one of RHU’s clinicians who told her that they saw she had a lot of problems and a lot of children. The clinician suggested that she went and got family planning but Lillian wanted something more permanent. “I want them to remove my tube. Let me remain with these six children. Because my children were all born with Sickle Cell Disease and keeping them is very difficult,” said Lillian. She opted for tubal ligation but her husband was yet to grant her permission to undergo the surgery so that she stops giving birth. “I know that he might be convinced but I don’t know when” Lillian added. One Ugandan commentator said that in Gulu like the rest of Uganda, contraceptive use was still too low and their uptake was still largely driven by male dominated culture and patriarchal values. Lillian said that it was very expensive looking after her six children who all need daily medication. “I don’t have enough money for keeping them,” she said. Much of her time is spent in hospital with her sick children so she says that she is unable to get a job. Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE
Our staff never turn anyone away
At the end of a long day, Anicia, closes the clinic with praise for her colleagues who never turn anyone away. "We open at 8am. From 8am we will be receiving a variety of clients for different services - whether post-abortion care, whether antenatal care - we have to give them all the services. We may end up to 10pm, because we'll never chase our clients, we'll never close the place when we have a client inside. People come when they have no hope. You receive them, and you give them hope by treating them properly and giving them quality services. The client gets better and will never forget you. And follow them up on the phone. "How are you doing?" It's good for us to know that they're doing well. Others even tell us 'The way you handle us, we love it so much'."; Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE

Overview: A one-stop shop providing vital healthcare
Uganda has one of the highest fertility rates in the world, and as a result, it also has one of the most youthful populations - more than half of Ugandans are under the age of 15. Over 78% of the population is below the age of 30. The population is growing at a rate of more than 3% per year. Figures show that women – on average - give birth to two more children than they want. More than half of pregnancies in Uganda are unintended, and nearly a third of these end in abortion according to figures from the Guttmacher Institute. It also says that in Uganda approximately one in every 19 women has an abortion per year and with abortion being highly restricted most of these are unsafe. This rate is far higher than the average for East Africa and reflects the high level of unmet need for contraception in the country. Approximately, 755,000 unintended pregnancies occur annually out of which 297,000 result in unsafe abortions. Unintended pregnancy is common in Uganda, leading to high levels of unplanned births, unsafe abortions, and maternal injury and death. Women in the eastern and north regions had the highest proportions of unplanned births (50–54%) the high levels of unintended pregnancy and unplanned births in Uganda can be attributed primarily to nonuse of contraceptives by women who do not want a child soon. More than 80% of the population lives in rural areas. Millions of people still do not have access to a health clinic, and family planning, especially long term and permanent methods, is not available to the vast majority who live in rural and hard-to-reach areas. IPPF’s Member Association, Reproductive Health Uganda (RHU), is working hard on the ground to tackle these issues. It takes the approach that it offers people as many services as possible at its clinics so you can get your health needs met in the same place. This means you might go to a clinic for an HIV test but leave having being offered a range of contraception plus other tests for other sexually transmitted diseases or cancer. RHU has a network of clinics across the country and takes its services out to remote and rural areas through its mobile clinics. No one is left out by RHU. Whether people are poor or vulnerable or hard to reach, RHU makes sure they have access to all of the services they need. We visited one of RHU’s health facilities in northern Uganda to get a better idea of how our work makes a real difference to people and their lives. We wanted to hear stories about what difference getting contraception, counselling and testing meant in reality. For many people it is life-changing. Thousands of people go in and out of Gulu Clinic every year and thousands more get services through Gulu’s mobile clinics. Last year alone Gulu Clinic had 229,812 family planning clients and provided 769,707 sexual health services, 390,488 of those were to young people. It offers a ‘one-stop-shop’ approach which makes it easier for clients to get a range of integrated services. They can go to a clinic for a check-up but end up getting contraception, counselling and a whole range of other tests and treatments. These include family planning, infertility management, cervical cancer screening, cryotherapy, youth friendly services, sexually transmitted infections and general sexual and reproductive health (SRH). Denis Bongonyinge, who has worked at Gulu Clinic for four years, said: “For us our goal is to ensure that this place is just a one stop centre. When a client comes in, he goes out when he has got a very big package of services within the clinic. Even if we go out, we give very many services. Denis said he had come across a range of issues among the clients. Issues like high rates of teenage pregnancies, sexually transmitted infections and gender based violence which could all be dealt with at the centre. He added that he believed Gulu had managed to offer such a range of services because of its willingness to work with other partners interested in scaling up uptake of family planning and generally sexual and reproductive health services. Gulu Clinic is also inclusive to a wide range of people across the community and this includes sex workers and disabled people. Vicky Acora is deaf and has had problems getting services at other hospitals. But, she says about RHU: “They are really most welcoming and they try to communicate even in the little sign language they know. They are really very warm” She says she has since been advising other deaf persons to seek services at Reproductive Health Uganda because of the quick services. “I encourage other people to come here because it is fairer. I encourage other disabled people who use wheelchairs not only the deaf to come and access services here because it is really accessible for those who have a disability.” Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE
Reproductive Health Uganda: A one-stop shop of life-changing services
Reproductive Health Uganda: A one-stop shop of life-changing services" Every year tens of thousands of Ugandans walk through the doors at Gulu Clinic. Everyone is welcome. Here are just a few of the people that went to the clinic one day last month. READ MORE 7:00 "I was suffering…..so my sister decided to bring me here. When she brought me here, I was treated and I got better. I really admired how they do their things and I really wanted to learn more about Reproductive Health." READ MORE 8:00 "I grew up alone. I ended up dropping out of school and I went for sex working. I came purposely here to RHU for Hepatitis B testing and also counselling because I have so many personal problems. I like coming here….they’re so caring." READ MORE 09:00 Fertility treatment remains a sensitive issue for men and women in Uganda but Brenda and her husband, Francis decided to visit Reproductive Health Uganda's clinic in Gulu. “They helped us a lot and we get proper treatment." READ MORE 15:00 "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 16:00 "Our goal is to ensure this Reproductive Health Uganda clinic in Gulu is a 'one-stop-centre'. When a client comes in, she comes out when she has got a very big package of services. And when we go to do outreach in the community we give very many services" READ MORE 17:00 At the end of a long day, Anicia, closes the clinic with praise for her colleagues who never turn anyone away. "We open at 8am…and we may end up sometimes up to 10pm because we never chase out our client. We’ll never close the place when we have a client inside. People come when they have no hope.” READ MORE 22:00

Putting clients first: a one-stop shop of outreach services in Gulu, Uganda
.p { text-align: justify; align: left; } Uganda has one of the highest fertility rates in the world, and as a result, it also has one of the most youthful populations - more than half of Ugandans are under the age of 15. Over 78% of the population is below the age of 30. The population is growing at a rate of more than 3% per year. Figures show that women – on average - give birth to two more children than they want. More than half of pregnancies in Uganda are unintended, and nearly a third of these end in abortion according to figures from the Guttmacher Institute. It also says that in Uganda approximately one in every 19 women has an abortion per year and with abortion being highly restricted most of these are unsafe. This rate is far higher than the average for East Africa and reflects the high level of unmet need for contraception in the country. Approximately, 755,000 unintended pregnancies occur annually out of which 297,000 result in unsafe abortions. Unintended pregnancy is common in Uganda, leading to high levels of unplanned births, unsafe abortions, and maternal injury and death. Women in the eastern and north regions had the highest proportions of unplanned births (50–54%) the high levels of unintended pregnancy and unplanned births in Uganda can be attributed primarily to nonuse of contraceptives by women who do not want a child soon. More than 80% of the population lives in rural areas. Millions of people still do not have access to a health clinic, and family planning, especially long term and permanent methods, is not available to the vast majority who live in rural and hard-to-reach areas. IPPF’s Member Association, Reproductive Health Uganda (RHU), is working hard on the ground to tackle these issues. It takes the approach that it offers people as many services as possible at its clinics so you can get your health needs met in the same place. This means you might go to a clinic for an HIV test but leave having being offered a range of contraception plus other tests for other sexually transmitted diseases or cancer. RHU has a network of clinics across the country and takes its services out to remote and rural areas through its mobile clinics. No one is left out by RHU. Whether people are poor or vulnerable or hard to reach, RHU makes sure they have access to all of the services they need. We visited one of RHU’s health facilities in northern Uganda to get a better idea of how our work makes a real difference to people and their lives. We wanted to hear stories about what difference getting contraception, counselling and testing meant in reality. For many people it is life-changing. Thousands of people go in and out of Gulu Clinic every year and thousands more get services through Gulu’s mobile clinics. Last year alone Gulu Clinic had 229,812 family planning clients and provided 769,707 sexual health services, 390,488 of those were to young people. It offers a ‘one-stop-shop’ approach which makes it easier for clients to get a range of integrated services. They can go to a clinic for a check-up but end up getting contraception, counselling and a whole range of other tests and treatments. These include family planning, infertility management, cervical cancer screening, cryotherapy, youth friendly services, sexually transmitted infections and general sexual and reproductive health (SRH). Denis Bongonyinge, who has worked at Gulu Clinic for four years, said: “For us our goal is to ensure that this place is just a one stop centre. When a client comes in, he goes out when he has got a very big package of services within the clinic. Even if we go out, we give very many services. Denis said he had come across a range of issues among the clients. Issues like high rates of teenage pregnancies, sexually transmitted infections and gender based violence which could all be dealt with at the centre. He added that he believed Gulu had managed to offer such a range of services because of its willingness to work with other partners interested in scaling up uptake of family planning and generally sexual and reproductive health services. Gulu Clinic is also inclusive to a wide range of people across the community and this includes sex workers and disabled people. Vicky Acora is deaf and has had problems getting services at other hospitals. But, she says about RHU: “They are really most welcoming and they try to communicate even in the little sign language they know. They are really very warm” She says she has since been advising other deaf persons to seek services at Reproductive Health Uganda because of the quick services. “I encourage other people to come here because it is fairer. I encourage other disabled people who use wheelchairs not only the deaf to come and access services here because it is really accessible for those who have a disability.” Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE
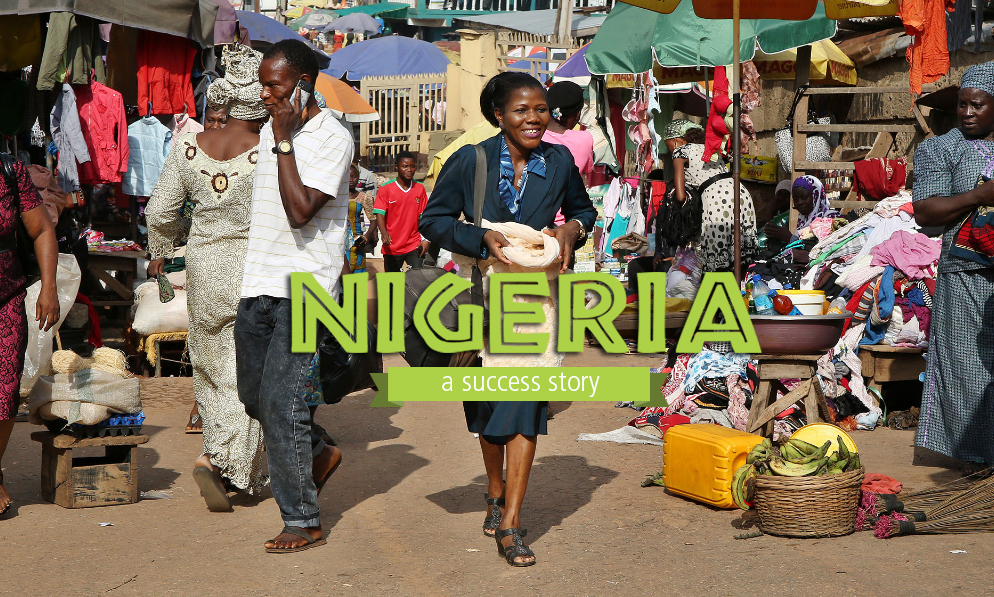
Changing lives in Nigeria
Nigeria has Africa’s biggest population. And it’s still growing at 3% a year. A lack of family planning is one reason – many women and girls want contraception – but like millions around the world – can’t get it. But that could be about to change, thanks to a pilot project run by Planned Parenthood Federation of Nigeria (PPFN), IPPF’s national member. It’s proving a huge success. This is its story, told by the women whose lives it has changed and the people working to change them. LAUNCH THE INTERACTIVE STORY
Gulu clinic: A one stop shop of services in rural Uganda
Uganda has one of the highest fertility rates in the world, and as a result, it also has one of the most youthful populations - more than half of Ugandans are under the age of 15. Approximately, 755,000 unintended pregnancies occur annually out of which 297,000 result in unsafe abortions. We are working hard on the ground to tackle these issues. Our Member takes the approach of offering people as many services as possible to get all health needs met in the same place. See a day in the life of the staff and clients of Gulu clinic, Uganda.

The story behind changing lives in Nigeria
SIZE defines many things about Nigeria. Being Africa’s most populous country ensures that plenty of the issues it faces are big. Nigeria’s population is around 188 million, and growing at more than 3% a year. Around a quarter of young women will be mothers or pregnant by the age of 19. One reason is a historically low use of contraception – at around 10%. One estimate suggests 35% of 15-24-year-olds who want access to contraception can’t get it – creating a huge unmet need for family planning. Nigeria’s Government has pledged to do something about that gap. It wants to increase the use of contraception to 36% by 2018 - its part in the global effort to give women around the world equal access to contraception. And a pilot programme run in Oyo State by the Planned Parenthood Federation of Nigeria (PPFN), IPPF’s national member, has offered startling progress. ClusterPLUS is something of a hybrid. It was built on the foundation of PPFN’s previous work but added new thinking, including ideas developed by IPPF member associations in Kenya and Uganda, who helped PPFN adapt them for Nigeria. At its heart is a simple concept - partnership. The closer you can get to local communities, the better you work with national and local government and more you try to build local ownership, the better. The project used PPFN’s earlier development of “clusters” of clinics, pharmacies and other outlets, as a base. The original cluster project, introduced in 2009, was funded in part by the UK Department for International Development. One ClusterPLUS innovation was a tireless approach to community outreach. In villages without permanent centres, clinics would set-up for three days at a time in schools, churches, markets or mosques. But to make sure everyone who could benefit from them knew they were coming, workers armed with enthusiasm and megaphones would go around drumming-up interest first. These CHEWS (Community Health Extension Workers), lent from Nigeria’s Ministry, did far more than generate publicity though. They also lived in the communities and were trained to supply forms of contraception themselves. Women unable to get to a clinic, perhaps because of work, could visit a CHEW at home in the evening. Often they might bring a friend too. Greater accessibility boosted the numbers of women using contraception. Sherifat Adelke is a 32-year-old CHEW with the Joy Hospital in Ibadan. She thinks her Islamic faith helped one fellow Muslim to end his opposition to his wife using contraception. “He was furious at me and kept looking at my Hijab. Then he asked me if I was a Muslim at all. I told him the Quran didn’t instruct Muslims not to use Family Planning. After enough lecture, he agreed. That was a victory for me.” Male opposition wasn’t anything new. PPFN was already using “male motivators” to combat men’s ignorance about contraception. Owolabi Temidayo is one male motivator in Ibadan. “Some men believe that when their wives start using family planning they will become promiscuous. Others believe if their wives have implants they won’t be able to enjoy intercourse. The religious ones believe family planning is a sin. "I go places to educate men. I go to motor parks, markets, town hall meetings, speaking on the need for family planning. It goes a long way in clearing the misinformation out there.” One partnership which proved critical to ClusterPLUS was between PPFN and local government in Oyo State – it helped to galvanise local leadership and create buy-in from officials. And the support was concrete. As well as providing three clinical staff, local authorities supplied the contraceptives and places for training, for meetings and for clinics. ClusterPLUS also set out to emphasize the benefit of long acting forms of contraception such as implants and IUCDs. And their provision was integrated with other services. Someone coming to a clinic for breast or cervical cancer screening or a test for HIV or a sexual transmitted infection would find family planning available there and then. Reaching those in poorer communities was also a priority. 28-year-old Tawa Agungbaide was responsible for making sure that one group of 63 women who couldn’t afford to pay for contraception gain access to it nevertheless. “We realized finance was a huge challenge. In some instances, it wasn’t a question of paying for services, but also of not even having enough money to pay for their transport to a clinic.” The solution, says Tawa, was a voucher scheme, funding transport and contraception for women who simply couldn’t fund it themselves. It helped her group and many others. “With eligibility criteria, we were able to single women who really couldn’t afford family planning. The voucher scheme was able to solve that. I feel fulfilled helping these women.” And new technology has played a major part too. An app on tablets and smartphones allowed health workers to input what they’d handed out every day – quickly and in real time. The supply team could then make sure that a delivery point never ran out of supplies – avoiding the dreaded stock-out. How well has it worked? The figures are impressive. The project aimed to reach 20,200 people in its nine months. It actually got to 53,152 clients. But as well as reaching more people, with more family planning services, it also gave women wider choice about the form of contraception they wanted. Two thirds of new users chose long-acting forms of contraception, more than double the rate outside of the project. The aim for PPFN now is to roll out the same approach across Nigeria, reaching more young people, especially poorer women. ClusterPLUS is already running in three other states in Nigeria – and if it proves as successful as in Oyo State, Nigeria’s Government will be making big progress towards its family planning pledge. See this full interactive success story from Nigeria
Girls Decide
This programme addresses critical challenges faced by young women around sexual health and sexuality. It has produced a range of advocacy, education and informational materials to support research, awareness-raising, advocacy and service delivery. Girls Decide is about the sexual and reproductive health and rights of girls and young women. Around the world, girls aged 10 to 19 account for 23% of all disease associated with pregnancy and childbirth. An estimated 2.5 million have unsafe abortions every year. Worldwide, young women account for 60% of the 5.5 million young people living with HIV and/or AIDS. Girls Decide has produced a range of advocacy, education and informational materials to support work to improve sexual health and rights for girls and young women. These include a series of films on sexual and reproductive health decisions faced by 6 young women in 6 different countries. The films won the prestigious International Video and Communications Award (IVCA). When girls and young women have access to critical lifesaving services and information, and when they are able to make meaningful choices about their life path, they are empowered. Their quality of life improves, as does the well-being of their families and the communities in which they live. Their collective ability to achieve internationally agreed development goals is strengthened. Almost all IPPF Member Associations provide services to young people and 1 in every 3 clients is a young person below the age of 25. All young women and girls are rights-holders and are entitled to sexual and reproductive rights. As a matter of principle, the IPPF Secretariat and Member Associations stand by girls by respecting and fulfilling their right to high quality services; they stand up for girls by supporting them in making their own decisions related to sexuality and pregnancy; they stand for sexual and reproductive rights by addressing the challenges faced by young women and girls at local, national and international levels.
At a Glance 2015
Key facts and figures highlighting IPPF's achievements in 2015.
Pagination
- Previous page
- Page 4
- Next page







