Spotlight
A selection of stories from across the Federation

Advances in Sexual and Reproductive Rights and Health: 2024 in Review
Let’s take a leap back in time to the beginning of 2024: In twelve months, what victories has our movement managed to secure in the face of growing opposition and the rise of the far right? These victories for sexual and reproductive rights and health are the result of relentless grassroots work and advocacy by our Member Associations, in partnership with community organizations, allied politicians, and the mobilization of public opinion.
Most Popular This Week

Advances in Sexual and Reproductive Rights and Health: 2024 in Review
Let’s take a leap back in time to the beginning of 2024: In twelve months, what victories has our movement managed to secure in t
Kazakhstan

Kazakhstan's Rising HIV Crisis: A Call for Action
On World AIDS Day, we commemorate the remarkable achievements of IPPF Member Associations in their unwavering commitment to combating the HIV epidemic.

Ensuring SRHR in Humanitarian Crises: What You Need to Know
Over the past two decades, global forced displacement has consistently increased, affecting an estimated 114 million people as of mid-2023.
Estonia, Nepal, Namibia, Japan, Thailand

The Rainbow Wave for Marriage Equality
Love wins! The fight for marriage equality has seen incredible progress worldwide, with a recent surge in legalizations.
France, Germany, Poland, United Kingdom, United States, Colombia, India, Tunisia

Abortion Rights: Latest Decisions and Developments around the World
Over the past 30 years, more than

Palestine

In their own words: The people providing sexual and reproductive health care under bombardment in Gaza
Week after week, heavy Israeli bombardment from air, land, and sea, has continued across most of the Gaza Strip.
Vanuatu

When getting to the hospital is difficult, Vanuatu mobile outreach can save lives
In the mountains of Kumera on Tanna Island, Vanuatu, the village women of Kamahaul normally spend over 10,000 Vatu ($83 USD) to travel to the nearest hospital.
Filter our stories by:
- Afghanistan
- Albania
- Aruba
- Bangladesh
- Benin
- Botswana
- Burundi
- Cambodia
- Cameroon
- Colombia
- Congo, Dem. Rep.
- Cook Islands
- El Salvador
- Estonia
- Ethiopia
- Fiji
- France
- Germany
- Ghana
- Guinea-Conakry
- India
- Ireland
- Jamaica
- Japan
- Kazakhstan
- Kenya
- Kiribati
- Lesotho
- Malawi
- (-) Mali
- Mozambique
- Namibia
- Nepal
- Nigeria
- Pakistan
- Palestine
- Poland
- (-) Senegal
- Somaliland
- Sri Lanka
- Sudan
- Thailand
- Togo
- Tonga
- Trinidad and Tobago
- Tunisia
- Uganda
- United Kingdom
- United States
- Vanuatu
- Zambia


| 08 January 2021
"Girls have to know their rights"
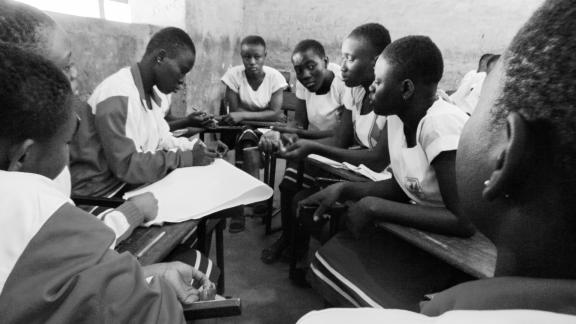
Aminata Sonogo listened intently to the group of young volunteers as they explained different types of contraception, and raised her hand with questions. Sitting at a wooden school desk at 22, Aminata is older than most of her classmates, but she shrugs off the looks and comments. She has fought hard to be here. Aminata is studying in Bamako, the capital of Mali. Just a quarter of Malian girls complete secondary school, according to UNICEF. But even if she will graduate later than most, Aminata is conscious of how far she has come. “I wanted to go to high school but I needed to pass some exams to get here. In the end, it took me three years,” she said. At the start of her final year of collège, or middle school, Aminata got pregnant. She is far from alone: 38% of Malian girls will be pregnant or a mother by the age of 18. Abortion is illegal in Mali except in cases of rape, incest or danger to the mother’s life, and even then it is difficult to obtain, according to medical professionals. Determined to take control of her life “I felt a lot of stigma from my classmates and even my teachers. I tried to ignore them and carry on going to school and studying. But I gave birth to my daughter just before my exams, so I couldn’t take them.” Aminata went through her pregnancy with little support, as the father of her daughter, Fatoumata, distanced himself from her after arguments about their situation. “I have had some problems with the father of the baby. We fought a lot and I didn’t see him for most of the pregnancy, right until the birth,” she recalled. The first year of her daughter’s life was a blur of doctors’ appointments, as Fatoumata was often ill. It seemed Aminata’s chances of finishing school were slipping away. But gradually her family began to take a more active role in caring for her daughter, and she began demanding more help from Fatoumata’s father too. She went back to school in the autumn, 18 months after Fatoumata’s birth and with more determination than ever. She no longer had time to hang out with friends after school, but attended classes, took care of her daughter and then studied more. At the end of the academic year, it paid off. “I did it. I passed my exams and now I am in high school,” Aminata said, smiling and relaxing her shoulders. "Family planning protects girls" Aminata’s next goal is her high school diploma, and obtaining it while trying to navigate the difficult world of relationships and sex. “It’s something you can talk about with your close friends. I would be too ashamed to talk about this with my parents,” she said. She is guided by visits from the young volunteers of the Association Malienne pour la Protection et Promotion de la Famille (AMPPF), and shares her own story with classmates who she sees at risk. “The guys come up to you and tell you that you are beautiful, but if you don’t want to sleep with them they will rape you. That’s the choice. You can accept or you can refuse and they will rape you anyway,” she said. “Girls have to know their rights”. After listening to the volunteers talk about all the different options for contraception, she is reviewing her own choices. “Family planning protects girls,” Aminata said. “It means we can protect ourselves from pregnancies that we don’t want”.

| 16 May 2025
"Girls have to know their rights"
Aminata Sonogo listened intently to the group of young volunteers as they explained different types of contraception, and raised her hand with questions. Sitting at a wooden school desk at 22, Aminata is older than most of her classmates, but she shrugs off the looks and comments. She has fought hard to be here. Aminata is studying in Bamako, the capital of Mali. Just a quarter of Malian girls complete secondary school, according to UNICEF. But even if she will graduate later than most, Aminata is conscious of how far she has come. “I wanted to go to high school but I needed to pass some exams to get here. In the end, it took me three years,” she said. At the start of her final year of collège, or middle school, Aminata got pregnant. She is far from alone: 38% of Malian girls will be pregnant or a mother by the age of 18. Abortion is illegal in Mali except in cases of rape, incest or danger to the mother’s life, and even then it is difficult to obtain, according to medical professionals. Determined to take control of her life “I felt a lot of stigma from my classmates and even my teachers. I tried to ignore them and carry on going to school and studying. But I gave birth to my daughter just before my exams, so I couldn’t take them.” Aminata went through her pregnancy with little support, as the father of her daughter, Fatoumata, distanced himself from her after arguments about their situation. “I have had some problems with the father of the baby. We fought a lot and I didn’t see him for most of the pregnancy, right until the birth,” she recalled. The first year of her daughter’s life was a blur of doctors’ appointments, as Fatoumata was often ill. It seemed Aminata’s chances of finishing school were slipping away. But gradually her family began to take a more active role in caring for her daughter, and she began demanding more help from Fatoumata’s father too. She went back to school in the autumn, 18 months after Fatoumata’s birth and with more determination than ever. She no longer had time to hang out with friends after school, but attended classes, took care of her daughter and then studied more. At the end of the academic year, it paid off. “I did it. I passed my exams and now I am in high school,” Aminata said, smiling and relaxing her shoulders. "Family planning protects girls" Aminata’s next goal is her high school diploma, and obtaining it while trying to navigate the difficult world of relationships and sex. “It’s something you can talk about with your close friends. I would be too ashamed to talk about this with my parents,” she said. She is guided by visits from the young volunteers of the Association Malienne pour la Protection et Promotion de la Famille (AMPPF), and shares her own story with classmates who she sees at risk. “The guys come up to you and tell you that you are beautiful, but if you don’t want to sleep with them they will rape you. That’s the choice. You can accept or you can refuse and they will rape you anyway,” she said. “Girls have to know their rights”. After listening to the volunteers talk about all the different options for contraception, she is reviewing her own choices. “Family planning protects girls,” Aminata said. “It means we can protect ourselves from pregnancies that we don’t want”.

| 08 January 2021
"We see cases of early pregnancy from 14 years old – occasionally they are younger"
My name is Mariame Doumbia, I am a midwife with the Association Malienne pour la Protection et la Promotion de la Famille (AMPPF), providing family planning and sexual health services to Malians in and around the capital, Bamako. I have worked with AMPPF for almost six years in total, but there was a break two years ago when American funding stopped due to the Global Gag Rule. I was able to come back to work with Canadian funding for the project SheDecides, and they have paid my salary for the last two years. I work at fixed and mobile clinics in Bamako. In the neighbourhood of Kalabancoro, which is on the outskirts of the capital, I receive clients at the clinic who would not be able to afford travel to somewhere farther away. It’s a poor neighbourhood. Providing the correct information The women come with their ideas about sex, sometimes with lots of rumours, but we go through it all with them to explain what sexual health is and how to maintain it. We clarify things for them. More and more they come with their mothers, or their boyfriends or husbands. The youngest ones come to ask about their periods and how they can count their menstrual cycle. Then they start to ask about sex. These days the price of sanitary pads is going down, so they are using bits of fabric less often, which is what I used to see. Seeing the impact of our work We see cases of early pregnancy here in Kalabancoro, but the numbers are definitely going down. Most are from 14 years old upwards, though occasionally they are younger. SheDecides has brought so much to this clinic, starting with the fact that before the project’s arrival there was no one here at all for a prolonged period of time. Now the community has the right to information and I try my best to answer all their questions.

| 16 May 2025
"We see cases of early pregnancy from 14 years old – occasionally they are younger"
My name is Mariame Doumbia, I am a midwife with the Association Malienne pour la Protection et la Promotion de la Famille (AMPPF), providing family planning and sexual health services to Malians in and around the capital, Bamako. I have worked with AMPPF for almost six years in total, but there was a break two years ago when American funding stopped due to the Global Gag Rule. I was able to come back to work with Canadian funding for the project SheDecides, and they have paid my salary for the last two years. I work at fixed and mobile clinics in Bamako. In the neighbourhood of Kalabancoro, which is on the outskirts of the capital, I receive clients at the clinic who would not be able to afford travel to somewhere farther away. It’s a poor neighbourhood. Providing the correct information The women come with their ideas about sex, sometimes with lots of rumours, but we go through it all with them to explain what sexual health is and how to maintain it. We clarify things for them. More and more they come with their mothers, or their boyfriends or husbands. The youngest ones come to ask about their periods and how they can count their menstrual cycle. Then they start to ask about sex. These days the price of sanitary pads is going down, so they are using bits of fabric less often, which is what I used to see. Seeing the impact of our work We see cases of early pregnancy here in Kalabancoro, but the numbers are definitely going down. Most are from 14 years old upwards, though occasionally they are younger. SheDecides has brought so much to this clinic, starting with the fact that before the project’s arrival there was no one here at all for a prolonged period of time. Now the community has the right to information and I try my best to answer all their questions.

| 08 January 2021
"The movement helps girls to know their rights and their bodies"
My name is Fatoumata Yehiya Maiga. I’m 23-years-old, and I’m an IT specialist. I joined the Youth Action Movement at the end of 2018. The head of the movement in Mali is a friend of mine, and I met her before I knew she was the president. She invited me to their events and over time persuaded me to join. I watched them raising awareness about sexual and reproductive health, using sketches and speeches. I learnt a lot. Overcoming taboos I went home and talked about what I had seen and learnt with my family. In Africa, and even more so in the village where I come from in Gao, northern Mali, people don’t talk about these things. I wanted to take my sisters to the events, but every time I spoke about them my relatives would just say it was to teach girls to have sex, and that it’s taboo. That’s not what I believe. I think the movement helps girls, most of all, to know their sexual rights, their bodies, what to do and what not to do to stay healthy and safe. They don’t understand this concept. My family would say it was just a smokescreen to convince girls to get involved in something dirty. I have had to tell my younger cousins about their periods, for example, when they came from the village to live in the city. One of my cousins was so scared, and told me she was bleeding from her vagina and didn’t know why. We talk about managing periods in the Youth Action Movement, as well as how to manage cramps and feel better. The devastating impact of FGM But there was a much more important reason for me to join the movement. My parents are educated, so me and my sisters were never cut. I learned about female genital mutilation at a conference I attended in 2016. I didn’t know that there were different types of severity and ways that girls could be cut. I hadn’t understood quite how dangerous this practice is. Then, two years ago, I lost my friend Aïssata. She got married young, at 17. She struggled to conceive until she was 23. The day she gave birth, there were complications and she died. The doctors said that the excision was botched and that’s what killed her. From that day on, I decided I needed to teach all the girls in my community about how harmful this practice is for their health. I was so horrified by the way she died. Normally, girls in Mali are cut when they are three or four years old, though for some it’s done at birth. When they are older and get pregnant, I know they face the same challenges as every woman does giving birth, but they also live with the dangerous consequences of this unhealthy practice. The importance of talking openly The problem lies with the families. I want us, as a movement, to talk with the parents and explain to them how they can contribute to their children’s sexual health. I wish it were no longer a taboo between parents and their girls. But if we talk in such direct terms, they only see disobedience, and say that we are encouraging promiscuity. We need to talk to teenagers because they are already parents in many cases. They are the ones who decide to go through with cutting their daughters, or not. A lot of Mali is hard to reach though. We need travelling groups to go to those isolated rural areas and talk to people about sexual health. Pregnancy is the girl’s decision, and girls have a right to be healthy, and to choose their future.

| 16 May 2025
"The movement helps girls to know their rights and their bodies"
My name is Fatoumata Yehiya Maiga. I’m 23-years-old, and I’m an IT specialist. I joined the Youth Action Movement at the end of 2018. The head of the movement in Mali is a friend of mine, and I met her before I knew she was the president. She invited me to their events and over time persuaded me to join. I watched them raising awareness about sexual and reproductive health, using sketches and speeches. I learnt a lot. Overcoming taboos I went home and talked about what I had seen and learnt with my family. In Africa, and even more so in the village where I come from in Gao, northern Mali, people don’t talk about these things. I wanted to take my sisters to the events, but every time I spoke about them my relatives would just say it was to teach girls to have sex, and that it’s taboo. That’s not what I believe. I think the movement helps girls, most of all, to know their sexual rights, their bodies, what to do and what not to do to stay healthy and safe. They don’t understand this concept. My family would say it was just a smokescreen to convince girls to get involved in something dirty. I have had to tell my younger cousins about their periods, for example, when they came from the village to live in the city. One of my cousins was so scared, and told me she was bleeding from her vagina and didn’t know why. We talk about managing periods in the Youth Action Movement, as well as how to manage cramps and feel better. The devastating impact of FGM But there was a much more important reason for me to join the movement. My parents are educated, so me and my sisters were never cut. I learned about female genital mutilation at a conference I attended in 2016. I didn’t know that there were different types of severity and ways that girls could be cut. I hadn’t understood quite how dangerous this practice is. Then, two years ago, I lost my friend Aïssata. She got married young, at 17. She struggled to conceive until she was 23. The day she gave birth, there were complications and she died. The doctors said that the excision was botched and that’s what killed her. From that day on, I decided I needed to teach all the girls in my community about how harmful this practice is for their health. I was so horrified by the way she died. Normally, girls in Mali are cut when they are three or four years old, though for some it’s done at birth. When they are older and get pregnant, I know they face the same challenges as every woman does giving birth, but they also live with the dangerous consequences of this unhealthy practice. The importance of talking openly The problem lies with the families. I want us, as a movement, to talk with the parents and explain to them how they can contribute to their children’s sexual health. I wish it were no longer a taboo between parents and their girls. But if we talk in such direct terms, they only see disobedience, and say that we are encouraging promiscuity. We need to talk to teenagers because they are already parents in many cases. They are the ones who decide to go through with cutting their daughters, or not. A lot of Mali is hard to reach though. We need travelling groups to go to those isolated rural areas and talk to people about sexual health. Pregnancy is the girl’s decision, and girls have a right to be healthy, and to choose their future.

| 07 January 2021
In pictures: Overcoming the impact of the Global Gag Rule in Mali
In 2017, the Association Malienne pour la Protection et la Promotion de la Famille (AMPPF), was hit hard by the reinstatement of the Global Gag Rule (GGR). The impact was swift and devastating – depleted budgets meant that AMPPF had to cut back on key staff and suspend education activities and community healthcare provision. The situation turned around with funding from the Canadian Government supporting the SheDecides project, filling the gap left by GGR. AMPPF has been able to employ staff ensuring their team can reach the most vulnerable clients who would otherwise be left without access to sexual healthcare and increase their outreach to youth. Putting communities first Mama Keita Sy Diallo, midwife The SheDecides project has allowed AMPPF to maintain three mobile clinics, travelling to more remote areas where transportation costs and huge distances separate women from access to health and contraceptive care.“SheDecides has helped us a lot, above all in our work outside our own permanent clinics. When we go out in the community we have a lot of clients, and many women come to us who would otherwise not have the means to obtain advice or contraception,” explained Mama Keita Sy Diallo, a midwife and AMPPF board member. She runs consultations at community health centers in underserved areas of the Malian capital. “Everything is free for the women in these sessions.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email SheDecides projects ensures free access to healthcare and contraception Fatoumata Dramé, client By 9am at the Asaco Sekasi community health center in Bamako, its wooden benches are full of clients waiting their turn at a SheDecides outreach session. Fatoumata Dramé, 30, got here early and has already been fitted for a new implant. “I came here for family planning, and it’s my first time. I’ve just moved to the area so I came because it’s close to home,” she said. Bouncing two-month-old Tiemoko on her knee, Dramé said her main motivation was to space the births of her children. “I am a mum of three now. My first child is 7 years old. I try to leave three years between each child. It helps with my health,” she explained. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Targeting youth Mamadou Bah, Youth Action Movement “After the arrival of SheDecides, we intensified our targeting of vulnerable groups with activities in the evening, when domestic workers and those working during the day could attend,” said Mariam Modibo Tandina, who heads the national committee of the Youth Action Movement in Mali. “That means that young people in precarious situations could learn more about safer sex and family planning. Now they know how to protect themselves against sexually transmitted infections and unwanted pregnancies.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Speaking out against FGM Fatoumata Yehiya Maiga, youth volunteer Fatoumata’s decision to join the Youth Action Movement was fueled by a personal loss. “My parents are educated, so me and my sisters were never cut. I learned about female genital mutilation at a conference I attended in 2016. I didn’t know that there were different types of severity and ways that girls could be cut. I hadn’t understood quite how dangerous this practice is. Two years ago, I lost my friend Aïssata. She got married young, at 17. She struggled to conceive until she was 23. The day she gave birth, there were complications and she died. The doctors said that the excision was botched and that’s what killed her. From that day on, I decided I needed to teach all the girls in my community about how harmful this practice is for their health. I was so horrified by the way she died.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Using dance and comedy to talk about sex Abdoulaye Camara, Head of AMPPF dance troupe Abdoulaye’s moves are not just for fun. He is head of the dance troupe of the AMPPF’s Youth Action Movement, which uses dance and comedy sketches to talk about sex. It’s a canny way to deliver messages about everything from using condoms to taking counterfeit antibiotics, to an audience who are often confused and ashamed about such topics. “We distract them with dance and humour and then we transmit those important messages about sex without offending them,” explained Abdoulaye. “We show them that it’s not to insult them or show them up, but just to explain how these things happen.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Determination to graduate Aminata Sonogo, student Sitting at a wooden school desk at 22, Sonogo is older than most of her classmates, but she shrugs off the looks and comments. She has fought hard to be here. “I wanted to go to high school but I needed to pass some exams to get here. In the end, it took me three years,” she said.At the start of her final year of collège, or middle school, Sonogo got pregnant. She went back to school in the autumn, 18 months after Fatoumata’s birth and with more determination than ever. At the end of the academic year, it paid off. “I did it. I passed my exams and now I am in high school,” Sonogo said, smiling and relaxing her shoulders. She is guided by visits from the AMPPF youth volunteers and shares her own story with classmates who she sees at risk of an unwanted pregnancy. Share on Twitter Share on Facebook Share via WhatsApp Share via Email AMPPF’s mobile clinic offers a lifeline to remote communities Mariame Doumbia, midwife “I work at a mobile clinic. It’s important for accessibility, so that the women living in poorly serviced areas can access sexual and reproductive health services, and reliable information.I like what I do. I like helping people, especially the young ones. They know I am always on call to help them, and even if I don’t know the answer at that moment, I will find out. I like everything about my work. Actually, it’s not just work for me, and I became a midwife for that reason. I’ve always been an educator on these issues in my community.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Trust underpins the relationship between AMPPF’s mobile team and the village of Missala Adama Samaké, village elder and chief of the Missala Health Center Adama Samaké, chief of the Missala Health Center, oversees the proceedings as a village elder with deep trust from his community. When the mobile clinic isn’t around, his center offers maternity services and treats the many cases of malaria that are diagnosed in the community. “Given the distance between here and Bamako, most of the villagers around here rely on us for treatment,” he said. “But when we announce that the mobile clinic is coming, the women make sure they are here.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Contraceptive choice Kadidiatou Sogoba, client Kadidiatou Sogoba, a mother of seven, waited nervously for her turn. “I came today because I keep getting ill and I have felt very weak, just not myself, since I had a Caesarean section three years ago. I lost a lot of blood,” she said. “I have been very afraid since the birth of my last child. We have been using condoms and we were getting a bit tired of them, so I am looking for another longer-term type of contraception.”After emerging half an hour later, Sogoba clutched a packet of the contraceptive pill, and said next time she would go for a cervical screening.Photos ©IPPF/Xaume Olleros/Mali Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 16 May 2025
In pictures: Overcoming the impact of the Global Gag Rule in Mali
In 2017, the Association Malienne pour la Protection et la Promotion de la Famille (AMPPF), was hit hard by the reinstatement of the Global Gag Rule (GGR). The impact was swift and devastating – depleted budgets meant that AMPPF had to cut back on key staff and suspend education activities and community healthcare provision. The situation turned around with funding from the Canadian Government supporting the SheDecides project, filling the gap left by GGR. AMPPF has been able to employ staff ensuring their team can reach the most vulnerable clients who would otherwise be left without access to sexual healthcare and increase their outreach to youth. Putting communities first Mama Keita Sy Diallo, midwife The SheDecides project has allowed AMPPF to maintain three mobile clinics, travelling to more remote areas where transportation costs and huge distances separate women from access to health and contraceptive care.“SheDecides has helped us a lot, above all in our work outside our own permanent clinics. When we go out in the community we have a lot of clients, and many women come to us who would otherwise not have the means to obtain advice or contraception,” explained Mama Keita Sy Diallo, a midwife and AMPPF board member. She runs consultations at community health centers in underserved areas of the Malian capital. “Everything is free for the women in these sessions.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email SheDecides projects ensures free access to healthcare and contraception Fatoumata Dramé, client By 9am at the Asaco Sekasi community health center in Bamako, its wooden benches are full of clients waiting their turn at a SheDecides outreach session. Fatoumata Dramé, 30, got here early and has already been fitted for a new implant. “I came here for family planning, and it’s my first time. I’ve just moved to the area so I came because it’s close to home,” she said. Bouncing two-month-old Tiemoko on her knee, Dramé said her main motivation was to space the births of her children. “I am a mum of three now. My first child is 7 years old. I try to leave three years between each child. It helps with my health,” she explained. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Targeting youth Mamadou Bah, Youth Action Movement “After the arrival of SheDecides, we intensified our targeting of vulnerable groups with activities in the evening, when domestic workers and those working during the day could attend,” said Mariam Modibo Tandina, who heads the national committee of the Youth Action Movement in Mali. “That means that young people in precarious situations could learn more about safer sex and family planning. Now they know how to protect themselves against sexually transmitted infections and unwanted pregnancies.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Speaking out against FGM Fatoumata Yehiya Maiga, youth volunteer Fatoumata’s decision to join the Youth Action Movement was fueled by a personal loss. “My parents are educated, so me and my sisters were never cut. I learned about female genital mutilation at a conference I attended in 2016. I didn’t know that there were different types of severity and ways that girls could be cut. I hadn’t understood quite how dangerous this practice is. Two years ago, I lost my friend Aïssata. She got married young, at 17. She struggled to conceive until she was 23. The day she gave birth, there were complications and she died. The doctors said that the excision was botched and that’s what killed her. From that day on, I decided I needed to teach all the girls in my community about how harmful this practice is for their health. I was so horrified by the way she died.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Using dance and comedy to talk about sex Abdoulaye Camara, Head of AMPPF dance troupe Abdoulaye’s moves are not just for fun. He is head of the dance troupe of the AMPPF’s Youth Action Movement, which uses dance and comedy sketches to talk about sex. It’s a canny way to deliver messages about everything from using condoms to taking counterfeit antibiotics, to an audience who are often confused and ashamed about such topics. “We distract them with dance and humour and then we transmit those important messages about sex without offending them,” explained Abdoulaye. “We show them that it’s not to insult them or show them up, but just to explain how these things happen.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Determination to graduate Aminata Sonogo, student Sitting at a wooden school desk at 22, Sonogo is older than most of her classmates, but she shrugs off the looks and comments. She has fought hard to be here. “I wanted to go to high school but I needed to pass some exams to get here. In the end, it took me three years,” she said.At the start of her final year of collège, or middle school, Sonogo got pregnant. She went back to school in the autumn, 18 months after Fatoumata’s birth and with more determination than ever. At the end of the academic year, it paid off. “I did it. I passed my exams and now I am in high school,” Sonogo said, smiling and relaxing her shoulders. She is guided by visits from the AMPPF youth volunteers and shares her own story with classmates who she sees at risk of an unwanted pregnancy. Share on Twitter Share on Facebook Share via WhatsApp Share via Email AMPPF’s mobile clinic offers a lifeline to remote communities Mariame Doumbia, midwife “I work at a mobile clinic. It’s important for accessibility, so that the women living in poorly serviced areas can access sexual and reproductive health services, and reliable information.I like what I do. I like helping people, especially the young ones. They know I am always on call to help them, and even if I don’t know the answer at that moment, I will find out. I like everything about my work. Actually, it’s not just work for me, and I became a midwife for that reason. I’ve always been an educator on these issues in my community.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Trust underpins the relationship between AMPPF’s mobile team and the village of Missala Adama Samaké, village elder and chief of the Missala Health Center Adama Samaké, chief of the Missala Health Center, oversees the proceedings as a village elder with deep trust from his community. When the mobile clinic isn’t around, his center offers maternity services and treats the many cases of malaria that are diagnosed in the community. “Given the distance between here and Bamako, most of the villagers around here rely on us for treatment,” he said. “But when we announce that the mobile clinic is coming, the women make sure they are here.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Contraceptive choice Kadidiatou Sogoba, client Kadidiatou Sogoba, a mother of seven, waited nervously for her turn. “I came today because I keep getting ill and I have felt very weak, just not myself, since I had a Caesarean section three years ago. I lost a lot of blood,” she said. “I have been very afraid since the birth of my last child. We have been using condoms and we were getting a bit tired of them, so I am looking for another longer-term type of contraception.”After emerging half an hour later, Sogoba clutched a packet of the contraceptive pill, and said next time she would go for a cervical screening.Photos ©IPPF/Xaume Olleros/Mali Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 23 January 2019
“Since the closure of the clinic ... we encounter a lot more problems in our area"
Senegal’s IPPF Member Association, Association Sénégalaise pour le Bien-Etre Familial (ASBEF) ran two clinics in the capital, Dakar, until funding was cut in 2017 due to the reinstatement of the Global Gag Rule (GGR) by the US administration. The ASBEF clinic in the struggling suburb of Guediawaye was forced to close as a result of the GGR, leaving just the main headquarters in the heart of the city. The GGR prohibits foreign non-governmental organizations (NGOs) who receive US assistance from providing abortion care services, even with the NGO’s non-US funds. Abortion is illegal in Senegal except when three doctors agree the procedure is required to save a mother’s life. ASBEF applied for emergency funds and now offers an alternative service to the population of Guediawaye, offering sexual and reproductive health services through pop-up clinics. Asba Hann is the president of the Guediawaye chapter of IPPF’s Africa region youth action movement. She explains how the Global Gag Rule (GGR) cuts have deprived youth of a space to ask questions about their sexuality and seek advice on contraception. “Since the closure of the clinic, the nature of our advocacy has changed. We encounter a lot more problems in our area, above all from young people and women asking for services. ASBEF (Association Sénégalaise pour le Bien-Etre Familial) was a little bit less expensive for them and in this suburb there is a lot of poverty. Our facilities as volunteers also closed. We offer information to young people but since the closure of the clinic and our space they no longer get it in the same way, because they used to come and visit us. We still do activities but it’s difficult to get the information out, so young people worry about their sexual health and can’t get the confirmation needed for their questions. Young people don’t want to be seen going to a pharmacy and getting contraception, at risk of being seen by members of the community. They preferred seeing a midwife, discreetly, and to obtain their contraception privately. Young people often also can’t afford the contraception in the clinics and pharmacies. It would be much easier for us to have a specific place to hold events with the midwives who could then explain things to young people. A lot of the teenagers here still aren’t connected to the internet and active on social media. Others work all day and can’t look at their phones, and announcements get lost when they look at all their messages at night. Being on the ground is the best way for us to connect to young people.”

| 16 May 2025
“Since the closure of the clinic ... we encounter a lot more problems in our area"
Senegal’s IPPF Member Association, Association Sénégalaise pour le Bien-Etre Familial (ASBEF) ran two clinics in the capital, Dakar, until funding was cut in 2017 due to the reinstatement of the Global Gag Rule (GGR) by the US administration. The ASBEF clinic in the struggling suburb of Guediawaye was forced to close as a result of the GGR, leaving just the main headquarters in the heart of the city. The GGR prohibits foreign non-governmental organizations (NGOs) who receive US assistance from providing abortion care services, even with the NGO’s non-US funds. Abortion is illegal in Senegal except when three doctors agree the procedure is required to save a mother’s life. ASBEF applied for emergency funds and now offers an alternative service to the population of Guediawaye, offering sexual and reproductive health services through pop-up clinics. Asba Hann is the president of the Guediawaye chapter of IPPF’s Africa region youth action movement. She explains how the Global Gag Rule (GGR) cuts have deprived youth of a space to ask questions about their sexuality and seek advice on contraception. “Since the closure of the clinic, the nature of our advocacy has changed. We encounter a lot more problems in our area, above all from young people and women asking for services. ASBEF (Association Sénégalaise pour le Bien-Etre Familial) was a little bit less expensive for them and in this suburb there is a lot of poverty. Our facilities as volunteers also closed. We offer information to young people but since the closure of the clinic and our space they no longer get it in the same way, because they used to come and visit us. We still do activities but it’s difficult to get the information out, so young people worry about their sexual health and can’t get the confirmation needed for their questions. Young people don’t want to be seen going to a pharmacy and getting contraception, at risk of being seen by members of the community. They preferred seeing a midwife, discreetly, and to obtain their contraception privately. Young people often also can’t afford the contraception in the clinics and pharmacies. It would be much easier for us to have a specific place to hold events with the midwives who could then explain things to young people. A lot of the teenagers here still aren’t connected to the internet and active on social media. Others work all day and can’t look at their phones, and announcements get lost when they look at all their messages at night. Being on the ground is the best way for us to connect to young people.”

| 23 January 2019
“Since the clinic closed in this town everything has been very difficult"
Senegal’s IPPF Member Association, Association Sénégalaise pour le Bien-Etre Familial (ASBEF) ran two clinics in the capital, Dakar, until funding was cut in 2017 due to the reinstatement of the Global Gag Rule (GGR) by the US administration. The ASBEF clinic in the struggling suburb of Guediawaye was forced to close as a result of the GGR, leaving just the main headquarters in the heart of the city. The GGR prohibits foreign non-governmental organizations (NGOs) who receive US assistance from providing abortion care services, even with the NGO’s non-US funds. Abortion is illegal in Senegal except when three doctors agree the procedure is required to save a mother’s life. ASBEF applied for emergency funds and now offers an alternative service to the population of Guediawaye, offering sexual and reproductive health services through pop-up clinics. Betty Guèye is a midwife who used to live in Guediawaye but moved to Dakar after the closure of the clinic in the suburb of Senegal’s capital following global gag rule (GGR) funding cuts. She describes the effects of the closure and how Association Sénégalaise pour le Bien-Etre Familial (ASBEF) staff try to maximise the reduced service they still offer. “Since the clinic closed in this town everything has been very difficult. The majority of Senegalese are poor and we are losing clients because they cannot access the main clinic in Dakar. If they have an appointment on a Monday, after the weekend they won’t have the 200 francs (35 US cents) needed for the bus, and they will wait until Tuesday or Wednesday to come even though they are in pain. The clinic was of huge benefit to the community of Guediawaye and the surrounding suburbs as well. What we see now is that women wait until pain or infections are at a more advanced stage before they visit us in Dakar. Another effect is that if they need to update their contraception they will exceed the date required for the new injection or pill and then get pregnant as a result. In addition, raising awareness of sexual health in schools and neighbourhoods is a key part of our work. Religion and the lack of openness in the parent-child relationship inhibit these conversations in Senegal, and so young people don’t tell their parents when they have sexual health problems. We were very present in this area and now we only appear much more rarely in their lives, which has had negative consequences for the health of our young people. If we were still there as before, there would be fewer teenage pregnancies as well, with the advice and contraception that we provide. However, we hand out medication, we care for the community and we educate them when we can, when we are here and we have the money to do so. Our prices remain the same and they are competitive compared with the private clinics and pharmacies in the area. Young people will tell you that they are closer to the midwives and nurses here than to their parents. They can tell them anything. If a girl tells me she has had sex I can give her the morning after pill, but if she goes to the local health center she may feel she is being watched by her neighbours.” Ndeye Yacine Touré is a midwife who regularly fields calls from young women in Guediawaye seeking advice on their sexual health, and who no longer know where to turn. The closure of the Association Sénégalaise pour le Bien-Etre Familial (ASBEF) clinic in their area has left them seeking often desperate solutions to the taboo of having a child outside of marriage. “Many of our colleagues lost their jobs, and these were people who were supporting their families. It was a loss for the area as a whole, because this is a very poor neighbourhood where people don’t have many options in life. ASBEF Guediawaye was their main source of help because they came here for consultations but also for confidential advice. The services we offer at ASBEF are special, in a way, especially in the area of family planning. Women were at ease at the clinic, but since then there is a gap in their lives. The patients call us day and night wanting advice, asking how to find the main clinic in Dakar. Some say they no longer get check-ups or seek help because they lack the money to go elsewhere. Others say they miss certain midwives or nurses. We make use of emergency funds in several ways. We do pop-up events. I also give them my number and tell them how to get to the clinic in central Dakar, and reassure them that it will all be confidential and that they can seek treatment there. In Senegal, a girl having sex outside marriage isn’t accepted. Some young women were taking contraception secretly, but since the closure of the clinic it’s no longer possible. Some of them got pregnant as a result. They don’t want to bump into their mother at the public clinic so they just stop taking contraception. In Senegal, a girl having sex outside marriage isn’t accepted. The impact on young people is particularly serious. Some tell me they know they have a sexually transmitted infection but they are too afraid to go to the hospital and get it treated. Before they could talk to us and tell us that they had sex, and we could help them. They have to hide now and some seek unsafe abortions. ”

| 16 May 2025
“Since the clinic closed in this town everything has been very difficult"
Senegal’s IPPF Member Association, Association Sénégalaise pour le Bien-Etre Familial (ASBEF) ran two clinics in the capital, Dakar, until funding was cut in 2017 due to the reinstatement of the Global Gag Rule (GGR) by the US administration. The ASBEF clinic in the struggling suburb of Guediawaye was forced to close as a result of the GGR, leaving just the main headquarters in the heart of the city. The GGR prohibits foreign non-governmental organizations (NGOs) who receive US assistance from providing abortion care services, even with the NGO’s non-US funds. Abortion is illegal in Senegal except when three doctors agree the procedure is required to save a mother’s life. ASBEF applied for emergency funds and now offers an alternative service to the population of Guediawaye, offering sexual and reproductive health services through pop-up clinics. Betty Guèye is a midwife who used to live in Guediawaye but moved to Dakar after the closure of the clinic in the suburb of Senegal’s capital following global gag rule (GGR) funding cuts. She describes the effects of the closure and how Association Sénégalaise pour le Bien-Etre Familial (ASBEF) staff try to maximise the reduced service they still offer. “Since the clinic closed in this town everything has been very difficult. The majority of Senegalese are poor and we are losing clients because they cannot access the main clinic in Dakar. If they have an appointment on a Monday, after the weekend they won’t have the 200 francs (35 US cents) needed for the bus, and they will wait until Tuesday or Wednesday to come even though they are in pain. The clinic was of huge benefit to the community of Guediawaye and the surrounding suburbs as well. What we see now is that women wait until pain or infections are at a more advanced stage before they visit us in Dakar. Another effect is that if they need to update their contraception they will exceed the date required for the new injection or pill and then get pregnant as a result. In addition, raising awareness of sexual health in schools and neighbourhoods is a key part of our work. Religion and the lack of openness in the parent-child relationship inhibit these conversations in Senegal, and so young people don’t tell their parents when they have sexual health problems. We were very present in this area and now we only appear much more rarely in their lives, which has had negative consequences for the health of our young people. If we were still there as before, there would be fewer teenage pregnancies as well, with the advice and contraception that we provide. However, we hand out medication, we care for the community and we educate them when we can, when we are here and we have the money to do so. Our prices remain the same and they are competitive compared with the private clinics and pharmacies in the area. Young people will tell you that they are closer to the midwives and nurses here than to their parents. They can tell them anything. If a girl tells me she has had sex I can give her the morning after pill, but if she goes to the local health center she may feel she is being watched by her neighbours.” Ndeye Yacine Touré is a midwife who regularly fields calls from young women in Guediawaye seeking advice on their sexual health, and who no longer know where to turn. The closure of the Association Sénégalaise pour le Bien-Etre Familial (ASBEF) clinic in their area has left them seeking often desperate solutions to the taboo of having a child outside of marriage. “Many of our colleagues lost their jobs, and these were people who were supporting their families. It was a loss for the area as a whole, because this is a very poor neighbourhood where people don’t have many options in life. ASBEF Guediawaye was their main source of help because they came here for consultations but also for confidential advice. The services we offer at ASBEF are special, in a way, especially in the area of family planning. Women were at ease at the clinic, but since then there is a gap in their lives. The patients call us day and night wanting advice, asking how to find the main clinic in Dakar. Some say they no longer get check-ups or seek help because they lack the money to go elsewhere. Others say they miss certain midwives or nurses. We make use of emergency funds in several ways. We do pop-up events. I also give them my number and tell them how to get to the clinic in central Dakar, and reassure them that it will all be confidential and that they can seek treatment there. In Senegal, a girl having sex outside marriage isn’t accepted. Some young women were taking contraception secretly, but since the closure of the clinic it’s no longer possible. Some of them got pregnant as a result. They don’t want to bump into their mother at the public clinic so they just stop taking contraception. In Senegal, a girl having sex outside marriage isn’t accepted. The impact on young people is particularly serious. Some tell me they know they have a sexually transmitted infection but they are too afraid to go to the hospital and get it treated. Before they could talk to us and tell us that they had sex, and we could help them. They have to hide now and some seek unsafe abortions. ”

| 22 January 2019
“I used to attend the clinic regularly and then one day I didn’t know what happened. The clinic just shut down"
Senegal’s IPPF Member Association, Association Sénégalaise pour le Bien-Etre Familial (ASBEF) ran two clinics in the capital, Dakar, until funding was cut in 2017 due to the reinstatement of the Global Gag Rule (GGR) by the US administration. The ASBEF clinic in the struggling suburb of Guediawaye was forced to close as a result of the GGR, leaving just the main headquarters in the heart of the city. The GGR prohibits foreign non-governmental organizations (NGOs) who receive US assistance from providing abortion care services, even with the NGO’s non-US funds. Abortion is illegal in Senegal except when three doctors agree the procedure is required to save a mother’s life. ASBEF applied for emergency funds and now offers an alternative service to the population of Guediawaye, offering sexual and reproductive health services through pop-up clinics. Maguette Mbow, a 33-year-old homemaker, describes how the closure of Association Sénégalaise pour le Bien-Etre Familial clinic in Guediawaye, a suburb of Dakar, has affected her, and explains the difficulties with the alternative providers available. She spoke about how the closure of her local clinic has impacted her life at a pop-up clinic set up for the day at a school in Guediawaye. “I heard that ASBEF (Association Sénégalaise pour le Bien-Etre Familial), was doing consultations here today and I dropped everything at home to come. There was a clinic here in Guediawaye but we don’t have it anymore. I’m here for family planning because that’s what I used to get at the clinic; it was their strong point. I take the Pill and I came to change the type I take, but the midwife advised me today to keep taking the same one. I’ve used the pill between my pregnancies. I have two children aged 2 and 6, but for now I’m not sure if I want a third child. When the clinic closed, I started going to the public facilities instead. There is always an enormous queue. You can get there in the morning and wait until 3pm for a consultation. (The closure) has affected everyone here very seriously. All my friends and family went to ASBEF Guediawaye, but now we are in the other public and private clinics receiving a really poor service. I had all of my pre-natal care at ASBEF and when I was younger I used the services for young people as well. They helped me take the morning after pill a few times and that really left its mark on me. They are great with young people; they are knowledgeable and really good with teenagers. There are still taboos surrounding sexuality in Senegal but they know how to handle them. These days, when ASBEF come to Guediawaye they have to set up in different places each time. It’s a bit annoying because if you know a place well and it’s full of well-trained people who you know personally, you feel more at ease. I would like things to go back to how they were before, and for the clinic to reopen. I would also have liked to send my children there one day when the time came, to benefit from the same service. Sometimes I travel right into Dakar for a consultation at the ASBEF headquarters, but often I don’t have the money.” Fatou Bimtou Diop, 20, is a final year student at Lycée Seydina Limamou Laye in Guediawaye. She explains why the closure of the Association Sénégalaise pour le Bien-Etre Familial clinic in her area in 2017 means she no longer regularly seeks advice on her sexual health. “I came here today for a consultation. I haven’t been for two years because the clinic closed. I don’t know why that happened but I would really like that decision to be reversed. Yes, there are other clinics here but I don’t feel as relaxed as with ASBEF (Association Sénégalaise pour le Bien-Etre Familial). I used to feel really at ease because there were other young people like me there. In the other clinics I know I might see someone’s mother or my aunties and it worries me too much. They explained things well and the set-up felt secure. We could talk about the intimate problems that were affecting us to the ASBEF staff. I went because I have really painful periods, for example. Sometimes I wouldn’t have the nerve to ask certain questions but my friends who went to the ASBEF clinic would ask and then tell me the responses that they got. These days we end up talking a lot about girls who are 14,15 years old who are pregnant. When the ASBEF clinic was there it was really rare to see a girl that young with a baby but now it happens very frequently. A friend’s younger sister has a little boy now and she had to have a caesarian section because she’s younger than us. The clinic in Dakar is too far away. I have to go to school during the day so I can’t take the time off. I came to the session today at school and it was good to discuss my problems, but it took quite a long time to get seen by a midwife.” Ngouye Cissé, a 30-year-old woman who gave birth to her first child in her early teens, but who has since used regular contraception provided by ASBEF (Association Sénégalaise pour le Bien-Etre Familial). She visits the association’s pop-up clinics whenever they are in Guediawaye. “I used to attend the clinic regularly and then one day I didn’t know what happened. The clinic just shut down. Senegal’s economic situation is difficult and we don’t have a lot of money. The fees for a consultation are quite expensive, but when ASBEF does come into the community it’s free. I most recently visited the pop-up clinic because I was having some vaginal discharge and I didn’t know why. The midwife took care of me and gave me some advice and medication. Before I came here for my check-up, the public hospital was asking me to do a lot of tests and I was afraid I had some kind of terrible disease. But when I came to the ASBEF midwife simply listened to me, explained what I had, and then gave me the right medication straight away. I feel really relieved. I’m divorced and I have three boys. I had pre-natal care with ASBEF for the first two pregnancies, but with the third, my 2-year-old son, I had to go to a public hospital. The experiences couldn’t be more different. First, there is a big difference in price, as ASBEF is much cheaper. Also, at the ASBEF clinic we are really listened to. The midwife explains things and gives me information. We can talk about our problems openly and without fear, unlike in other health centers. What I see now that the clinic has closed is a lot more pregnant young girls, problems with STIs and in order to get treatment we have to go to the public and private clinics. When people hear that ASBEF is back in town there is a huge rush to get a consultation, because the need is there but people don’t know where else to go. Unfortunately, the transport to go to the clinic in Dakar costs a lot of money for us that we don’t have. Some households don’t even have enough to eat. There isn’t a huge difference between the consultations in the old clinic and the pop-up events that ASBEF organize. They still listen to you properly and it’s well organized. It just takes longer to get seen.” Moudel Bassoum, a 22-year student studying NGO management in Dakar, explains why she has been unable to replace the welcome and care she received at the now closed Association Sénégalaise pour le Bien-Etre Familial clinic in her hometown of Guediawaye, but still makes us of the pop-up clinic when it is available. “I used to go to the clinic regularly but since it closed, we only see the staff rarely around here. I came with my friends today for a free check-up. I told the whole neighbourhood that ASBEF (Association Sénégalaise pour le Bien-Etre Familial) were doing a pop-up clinic today so that they could come for free consultations. It’s not easy to get to the main clinic in Dakar for us. The effects of the closure are numerous, especially on young people. It helped us so much but now I hear a lot more about teenage pregnancies and STIs, not to mention girls trying to abort pregnancies by themselves. When my friend had an infection she went all the way into Dakar for the consultation because the public clinic is more expensive. I would much rather talk to a woman about this type of problem and at the public clinic you don’t get to pick who you talk to. You have to say everything in front of everyone. I don’t think the service we receive since the closure is different when the ASBEF clinic set up here for the day, but the staff are usually not the same and it’s less frequent. It’s free so when they do come there are a lot of people. I would really like the clinic to be re-established when I have a baby one day. I want that welcome, and to know that they will listen to you.”

| 16 May 2025
“I used to attend the clinic regularly and then one day I didn’t know what happened. The clinic just shut down"
Senegal’s IPPF Member Association, Association Sénégalaise pour le Bien-Etre Familial (ASBEF) ran two clinics in the capital, Dakar, until funding was cut in 2017 due to the reinstatement of the Global Gag Rule (GGR) by the US administration. The ASBEF clinic in the struggling suburb of Guediawaye was forced to close as a result of the GGR, leaving just the main headquarters in the heart of the city. The GGR prohibits foreign non-governmental organizations (NGOs) who receive US assistance from providing abortion care services, even with the NGO’s non-US funds. Abortion is illegal in Senegal except when three doctors agree the procedure is required to save a mother’s life. ASBEF applied for emergency funds and now offers an alternative service to the population of Guediawaye, offering sexual and reproductive health services through pop-up clinics. Maguette Mbow, a 33-year-old homemaker, describes how the closure of Association Sénégalaise pour le Bien-Etre Familial clinic in Guediawaye, a suburb of Dakar, has affected her, and explains the difficulties with the alternative providers available. She spoke about how the closure of her local clinic has impacted her life at a pop-up clinic set up for the day at a school in Guediawaye. “I heard that ASBEF (Association Sénégalaise pour le Bien-Etre Familial), was doing consultations here today and I dropped everything at home to come. There was a clinic here in Guediawaye but we don’t have it anymore. I’m here for family planning because that’s what I used to get at the clinic; it was their strong point. I take the Pill and I came to change the type I take, but the midwife advised me today to keep taking the same one. I’ve used the pill between my pregnancies. I have two children aged 2 and 6, but for now I’m not sure if I want a third child. When the clinic closed, I started going to the public facilities instead. There is always an enormous queue. You can get there in the morning and wait until 3pm for a consultation. (The closure) has affected everyone here very seriously. All my friends and family went to ASBEF Guediawaye, but now we are in the other public and private clinics receiving a really poor service. I had all of my pre-natal care at ASBEF and when I was younger I used the services for young people as well. They helped me take the morning after pill a few times and that really left its mark on me. They are great with young people; they are knowledgeable and really good with teenagers. There are still taboos surrounding sexuality in Senegal but they know how to handle them. These days, when ASBEF come to Guediawaye they have to set up in different places each time. It’s a bit annoying because if you know a place well and it’s full of well-trained people who you know personally, you feel more at ease. I would like things to go back to how they were before, and for the clinic to reopen. I would also have liked to send my children there one day when the time came, to benefit from the same service. Sometimes I travel right into Dakar for a consultation at the ASBEF headquarters, but often I don’t have the money.” Fatou Bimtou Diop, 20, is a final year student at Lycée Seydina Limamou Laye in Guediawaye. She explains why the closure of the Association Sénégalaise pour le Bien-Etre Familial clinic in her area in 2017 means she no longer regularly seeks advice on her sexual health. “I came here today for a consultation. I haven’t been for two years because the clinic closed. I don’t know why that happened but I would really like that decision to be reversed. Yes, there are other clinics here but I don’t feel as relaxed as with ASBEF (Association Sénégalaise pour le Bien-Etre Familial). I used to feel really at ease because there were other young people like me there. In the other clinics I know I might see someone’s mother or my aunties and it worries me too much. They explained things well and the set-up felt secure. We could talk about the intimate problems that were affecting us to the ASBEF staff. I went because I have really painful periods, for example. Sometimes I wouldn’t have the nerve to ask certain questions but my friends who went to the ASBEF clinic would ask and then tell me the responses that they got. These days we end up talking a lot about girls who are 14,15 years old who are pregnant. When the ASBEF clinic was there it was really rare to see a girl that young with a baby but now it happens very frequently. A friend’s younger sister has a little boy now and she had to have a caesarian section because she’s younger than us. The clinic in Dakar is too far away. I have to go to school during the day so I can’t take the time off. I came to the session today at school and it was good to discuss my problems, but it took quite a long time to get seen by a midwife.” Ngouye Cissé, a 30-year-old woman who gave birth to her first child in her early teens, but who has since used regular contraception provided by ASBEF (Association Sénégalaise pour le Bien-Etre Familial). She visits the association’s pop-up clinics whenever they are in Guediawaye. “I used to attend the clinic regularly and then one day I didn’t know what happened. The clinic just shut down. Senegal’s economic situation is difficult and we don’t have a lot of money. The fees for a consultation are quite expensive, but when ASBEF does come into the community it’s free. I most recently visited the pop-up clinic because I was having some vaginal discharge and I didn’t know why. The midwife took care of me and gave me some advice and medication. Before I came here for my check-up, the public hospital was asking me to do a lot of tests and I was afraid I had some kind of terrible disease. But when I came to the ASBEF midwife simply listened to me, explained what I had, and then gave me the right medication straight away. I feel really relieved. I’m divorced and I have three boys. I had pre-natal care with ASBEF for the first two pregnancies, but with the third, my 2-year-old son, I had to go to a public hospital. The experiences couldn’t be more different. First, there is a big difference in price, as ASBEF is much cheaper. Also, at the ASBEF clinic we are really listened to. The midwife explains things and gives me information. We can talk about our problems openly and without fear, unlike in other health centers. What I see now that the clinic has closed is a lot more pregnant young girls, problems with STIs and in order to get treatment we have to go to the public and private clinics. When people hear that ASBEF is back in town there is a huge rush to get a consultation, because the need is there but people don’t know where else to go. Unfortunately, the transport to go to the clinic in Dakar costs a lot of money for us that we don’t have. Some households don’t even have enough to eat. There isn’t a huge difference between the consultations in the old clinic and the pop-up events that ASBEF organize. They still listen to you properly and it’s well organized. It just takes longer to get seen.” Moudel Bassoum, a 22-year student studying NGO management in Dakar, explains why she has been unable to replace the welcome and care she received at the now closed Association Sénégalaise pour le Bien-Etre Familial clinic in her hometown of Guediawaye, but still makes us of the pop-up clinic when it is available. “I used to go to the clinic regularly but since it closed, we only see the staff rarely around here. I came with my friends today for a free check-up. I told the whole neighbourhood that ASBEF (Association Sénégalaise pour le Bien-Etre Familial) were doing a pop-up clinic today so that they could come for free consultations. It’s not easy to get to the main clinic in Dakar for us. The effects of the closure are numerous, especially on young people. It helped us so much but now I hear a lot more about teenage pregnancies and STIs, not to mention girls trying to abort pregnancies by themselves. When my friend had an infection she went all the way into Dakar for the consultation because the public clinic is more expensive. I would much rather talk to a woman about this type of problem and at the public clinic you don’t get to pick who you talk to. You have to say everything in front of everyone. I don’t think the service we receive since the closure is different when the ASBEF clinic set up here for the day, but the staff are usually not the same and it’s less frequent. It’s free so when they do come there are a lot of people. I would really like the clinic to be re-established when I have a baby one day. I want that welcome, and to know that they will listen to you.”

| 08 January 2021
"Girls have to know their rights"
Aminata Sonogo listened intently to the group of young volunteers as they explained different types of contraception, and raised her hand with questions. Sitting at a wooden school desk at 22, Aminata is older than most of her classmates, but she shrugs off the looks and comments. She has fought hard to be here. Aminata is studying in Bamako, the capital of Mali. Just a quarter of Malian girls complete secondary school, according to UNICEF. But even if she will graduate later than most, Aminata is conscious of how far she has come. “I wanted to go to high school but I needed to pass some exams to get here. In the end, it took me three years,” she said. At the start of her final year of collège, or middle school, Aminata got pregnant. She is far from alone: 38% of Malian girls will be pregnant or a mother by the age of 18. Abortion is illegal in Mali except in cases of rape, incest or danger to the mother’s life, and even then it is difficult to obtain, according to medical professionals. Determined to take control of her life “I felt a lot of stigma from my classmates and even my teachers. I tried to ignore them and carry on going to school and studying. But I gave birth to my daughter just before my exams, so I couldn’t take them.” Aminata went through her pregnancy with little support, as the father of her daughter, Fatoumata, distanced himself from her after arguments about their situation. “I have had some problems with the father of the baby. We fought a lot and I didn’t see him for most of the pregnancy, right until the birth,” she recalled. The first year of her daughter’s life was a blur of doctors’ appointments, as Fatoumata was often ill. It seemed Aminata’s chances of finishing school were slipping away. But gradually her family began to take a more active role in caring for her daughter, and she began demanding more help from Fatoumata’s father too. She went back to school in the autumn, 18 months after Fatoumata’s birth and with more determination than ever. She no longer had time to hang out with friends after school, but attended classes, took care of her daughter and then studied more. At the end of the academic year, it paid off. “I did it. I passed my exams and now I am in high school,” Aminata said, smiling and relaxing her shoulders. "Family planning protects girls" Aminata’s next goal is her high school diploma, and obtaining it while trying to navigate the difficult world of relationships and sex. “It’s something you can talk about with your close friends. I would be too ashamed to talk about this with my parents,” she said. She is guided by visits from the young volunteers of the Association Malienne pour la Protection et Promotion de la Famille (AMPPF), and shares her own story with classmates who she sees at risk. “The guys come up to you and tell you that you are beautiful, but if you don’t want to sleep with them they will rape you. That’s the choice. You can accept or you can refuse and they will rape you anyway,” she said. “Girls have to know their rights”. After listening to the volunteers talk about all the different options for contraception, she is reviewing her own choices. “Family planning protects girls,” Aminata said. “It means we can protect ourselves from pregnancies that we don’t want”.

| 16 May 2025
"Girls have to know their rights"
Aminata Sonogo listened intently to the group of young volunteers as they explained different types of contraception, and raised her hand with questions. Sitting at a wooden school desk at 22, Aminata is older than most of her classmates, but she shrugs off the looks and comments. She has fought hard to be here. Aminata is studying in Bamako, the capital of Mali. Just a quarter of Malian girls complete secondary school, according to UNICEF. But even if she will graduate later than most, Aminata is conscious of how far she has come. “I wanted to go to high school but I needed to pass some exams to get here. In the end, it took me three years,” she said. At the start of her final year of collège, or middle school, Aminata got pregnant. She is far from alone: 38% of Malian girls will be pregnant or a mother by the age of 18. Abortion is illegal in Mali except in cases of rape, incest or danger to the mother’s life, and even then it is difficult to obtain, according to medical professionals. Determined to take control of her life “I felt a lot of stigma from my classmates and even my teachers. I tried to ignore them and carry on going to school and studying. But I gave birth to my daughter just before my exams, so I couldn’t take them.” Aminata went through her pregnancy with little support, as the father of her daughter, Fatoumata, distanced himself from her after arguments about their situation. “I have had some problems with the father of the baby. We fought a lot and I didn’t see him for most of the pregnancy, right until the birth,” she recalled. The first year of her daughter’s life was a blur of doctors’ appointments, as Fatoumata was often ill. It seemed Aminata’s chances of finishing school were slipping away. But gradually her family began to take a more active role in caring for her daughter, and she began demanding more help from Fatoumata’s father too. She went back to school in the autumn, 18 months after Fatoumata’s birth and with more determination than ever. She no longer had time to hang out with friends after school, but attended classes, took care of her daughter and then studied more. At the end of the academic year, it paid off. “I did it. I passed my exams and now I am in high school,” Aminata said, smiling and relaxing her shoulders. "Family planning protects girls" Aminata’s next goal is her high school diploma, and obtaining it while trying to navigate the difficult world of relationships and sex. “It’s something you can talk about with your close friends. I would be too ashamed to talk about this with my parents,” she said. She is guided by visits from the young volunteers of the Association Malienne pour la Protection et Promotion de la Famille (AMPPF), and shares her own story with classmates who she sees at risk. “The guys come up to you and tell you that you are beautiful, but if you don’t want to sleep with them they will rape you. That’s the choice. You can accept or you can refuse and they will rape you anyway,” she said. “Girls have to know their rights”. After listening to the volunteers talk about all the different options for contraception, she is reviewing her own choices. “Family planning protects girls,” Aminata said. “It means we can protect ourselves from pregnancies that we don’t want”.

| 08 January 2021
"We see cases of early pregnancy from 14 years old – occasionally they are younger"
My name is Mariame Doumbia, I am a midwife with the Association Malienne pour la Protection et la Promotion de la Famille (AMPPF), providing family planning and sexual health services to Malians in and around the capital, Bamako. I have worked with AMPPF for almost six years in total, but there was a break two years ago when American funding stopped due to the Global Gag Rule. I was able to come back to work with Canadian funding for the project SheDecides, and they have paid my salary for the last two years. I work at fixed and mobile clinics in Bamako. In the neighbourhood of Kalabancoro, which is on the outskirts of the capital, I receive clients at the clinic who would not be able to afford travel to somewhere farther away. It’s a poor neighbourhood. Providing the correct information The women come with their ideas about sex, sometimes with lots of rumours, but we go through it all with them to explain what sexual health is and how to maintain it. We clarify things for them. More and more they come with their mothers, or their boyfriends or husbands. The youngest ones come to ask about their periods and how they can count their menstrual cycle. Then they start to ask about sex. These days the price of sanitary pads is going down, so they are using bits of fabric less often, which is what I used to see. Seeing the impact of our work We see cases of early pregnancy here in Kalabancoro, but the numbers are definitely going down. Most are from 14 years old upwards, though occasionally they are younger. SheDecides has brought so much to this clinic, starting with the fact that before the project’s arrival there was no one here at all for a prolonged period of time. Now the community has the right to information and I try my best to answer all their questions.

| 16 May 2025
"We see cases of early pregnancy from 14 years old – occasionally they are younger"
My name is Mariame Doumbia, I am a midwife with the Association Malienne pour la Protection et la Promotion de la Famille (AMPPF), providing family planning and sexual health services to Malians in and around the capital, Bamako. I have worked with AMPPF for almost six years in total, but there was a break two years ago when American funding stopped due to the Global Gag Rule. I was able to come back to work with Canadian funding for the project SheDecides, and they have paid my salary for the last two years. I work at fixed and mobile clinics in Bamako. In the neighbourhood of Kalabancoro, which is on the outskirts of the capital, I receive clients at the clinic who would not be able to afford travel to somewhere farther away. It’s a poor neighbourhood. Providing the correct information The women come with their ideas about sex, sometimes with lots of rumours, but we go through it all with them to explain what sexual health is and how to maintain it. We clarify things for them. More and more they come with their mothers, or their boyfriends or husbands. The youngest ones come to ask about their periods and how they can count their menstrual cycle. Then they start to ask about sex. These days the price of sanitary pads is going down, so they are using bits of fabric less often, which is what I used to see. Seeing the impact of our work We see cases of early pregnancy here in Kalabancoro, but the numbers are definitely going down. Most are from 14 years old upwards, though occasionally they are younger. SheDecides has brought so much to this clinic, starting with the fact that before the project’s arrival there was no one here at all for a prolonged period of time. Now the community has the right to information and I try my best to answer all their questions.

| 08 January 2021
"The movement helps girls to know their rights and their bodies"
My name is Fatoumata Yehiya Maiga. I’m 23-years-old, and I’m an IT specialist. I joined the Youth Action Movement at the end of 2018. The head of the movement in Mali is a friend of mine, and I met her before I knew she was the president. She invited me to their events and over time persuaded me to join. I watched them raising awareness about sexual and reproductive health, using sketches and speeches. I learnt a lot. Overcoming taboos I went home and talked about what I had seen and learnt with my family. In Africa, and even more so in the village where I come from in Gao, northern Mali, people don’t talk about these things. I wanted to take my sisters to the events, but every time I spoke about them my relatives would just say it was to teach girls to have sex, and that it’s taboo. That’s not what I believe. I think the movement helps girls, most of all, to know their sexual rights, their bodies, what to do and what not to do to stay healthy and safe. They don’t understand this concept. My family would say it was just a smokescreen to convince girls to get involved in something dirty. I have had to tell my younger cousins about their periods, for example, when they came from the village to live in the city. One of my cousins was so scared, and told me she was bleeding from her vagina and didn’t know why. We talk about managing periods in the Youth Action Movement, as well as how to manage cramps and feel better. The devastating impact of FGM But there was a much more important reason for me to join the movement. My parents are educated, so me and my sisters were never cut. I learned about female genital mutilation at a conference I attended in 2016. I didn’t know that there were different types of severity and ways that girls could be cut. I hadn’t understood quite how dangerous this practice is. Then, two years ago, I lost my friend Aïssata. She got married young, at 17. She struggled to conceive until she was 23. The day she gave birth, there were complications and she died. The doctors said that the excision was botched and that’s what killed her. From that day on, I decided I needed to teach all the girls in my community about how harmful this practice is for their health. I was so horrified by the way she died. Normally, girls in Mali are cut when they are three or four years old, though for some it’s done at birth. When they are older and get pregnant, I know they face the same challenges as every woman does giving birth, but they also live with the dangerous consequences of this unhealthy practice. The importance of talking openly The problem lies with the families. I want us, as a movement, to talk with the parents and explain to them how they can contribute to their children’s sexual health. I wish it were no longer a taboo between parents and their girls. But if we talk in such direct terms, they only see disobedience, and say that we are encouraging promiscuity. We need to talk to teenagers because they are already parents in many cases. They are the ones who decide to go through with cutting their daughters, or not. A lot of Mali is hard to reach though. We need travelling groups to go to those isolated rural areas and talk to people about sexual health. Pregnancy is the girl’s decision, and girls have a right to be healthy, and to choose their future.

| 16 May 2025
"The movement helps girls to know their rights and their bodies"
My name is Fatoumata Yehiya Maiga. I’m 23-years-old, and I’m an IT specialist. I joined the Youth Action Movement at the end of 2018. The head of the movement in Mali is a friend of mine, and I met her before I knew she was the president. She invited me to their events and over time persuaded me to join. I watched them raising awareness about sexual and reproductive health, using sketches and speeches. I learnt a lot. Overcoming taboos I went home and talked about what I had seen and learnt with my family. In Africa, and even more so in the village where I come from in Gao, northern Mali, people don’t talk about these things. I wanted to take my sisters to the events, but every time I spoke about them my relatives would just say it was to teach girls to have sex, and that it’s taboo. That’s not what I believe. I think the movement helps girls, most of all, to know their sexual rights, their bodies, what to do and what not to do to stay healthy and safe. They don’t understand this concept. My family would say it was just a smokescreen to convince girls to get involved in something dirty. I have had to tell my younger cousins about their periods, for example, when they came from the village to live in the city. One of my cousins was so scared, and told me she was bleeding from her vagina and didn’t know why. We talk about managing periods in the Youth Action Movement, as well as how to manage cramps and feel better. The devastating impact of FGM But there was a much more important reason for me to join the movement. My parents are educated, so me and my sisters were never cut. I learned about female genital mutilation at a conference I attended in 2016. I didn’t know that there were different types of severity and ways that girls could be cut. I hadn’t understood quite how dangerous this practice is. Then, two years ago, I lost my friend Aïssata. She got married young, at 17. She struggled to conceive until she was 23. The day she gave birth, there were complications and she died. The doctors said that the excision was botched and that’s what killed her. From that day on, I decided I needed to teach all the girls in my community about how harmful this practice is for their health. I was so horrified by the way she died. Normally, girls in Mali are cut when they are three or four years old, though for some it’s done at birth. When they are older and get pregnant, I know they face the same challenges as every woman does giving birth, but they also live with the dangerous consequences of this unhealthy practice. The importance of talking openly The problem lies with the families. I want us, as a movement, to talk with the parents and explain to them how they can contribute to their children’s sexual health. I wish it were no longer a taboo between parents and their girls. But if we talk in such direct terms, they only see disobedience, and say that we are encouraging promiscuity. We need to talk to teenagers because they are already parents in many cases. They are the ones who decide to go through with cutting their daughters, or not. A lot of Mali is hard to reach though. We need travelling groups to go to those isolated rural areas and talk to people about sexual health. Pregnancy is the girl’s decision, and girls have a right to be healthy, and to choose their future.

| 07 January 2021
In pictures: Overcoming the impact of the Global Gag Rule in Mali
In 2017, the Association Malienne pour la Protection et la Promotion de la Famille (AMPPF), was hit hard by the reinstatement of the Global Gag Rule (GGR). The impact was swift and devastating – depleted budgets meant that AMPPF had to cut back on key staff and suspend education activities and community healthcare provision. The situation turned around with funding from the Canadian Government supporting the SheDecides project, filling the gap left by GGR. AMPPF has been able to employ staff ensuring their team can reach the most vulnerable clients who would otherwise be left without access to sexual healthcare and increase their outreach to youth. Putting communities first Mama Keita Sy Diallo, midwife The SheDecides project has allowed AMPPF to maintain three mobile clinics, travelling to more remote areas where transportation costs and huge distances separate women from access to health and contraceptive care.“SheDecides has helped us a lot, above all in our work outside our own permanent clinics. When we go out in the community we have a lot of clients, and many women come to us who would otherwise not have the means to obtain advice or contraception,” explained Mama Keita Sy Diallo, a midwife and AMPPF board member. She runs consultations at community health centers in underserved areas of the Malian capital. “Everything is free for the women in these sessions.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email SheDecides projects ensures free access to healthcare and contraception Fatoumata Dramé, client By 9am at the Asaco Sekasi community health center in Bamako, its wooden benches are full of clients waiting their turn at a SheDecides outreach session. Fatoumata Dramé, 30, got here early and has already been fitted for a new implant. “I came here for family planning, and it’s my first time. I’ve just moved to the area so I came because it’s close to home,” she said. Bouncing two-month-old Tiemoko on her knee, Dramé said her main motivation was to space the births of her children. “I am a mum of three now. My first child is 7 years old. I try to leave three years between each child. It helps with my health,” she explained. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Targeting youth Mamadou Bah, Youth Action Movement “After the arrival of SheDecides, we intensified our targeting of vulnerable groups with activities in the evening, when domestic workers and those working during the day could attend,” said Mariam Modibo Tandina, who heads the national committee of the Youth Action Movement in Mali. “That means that young people in precarious situations could learn more about safer sex and family planning. Now they know how to protect themselves against sexually transmitted infections and unwanted pregnancies.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Speaking out against FGM Fatoumata Yehiya Maiga, youth volunteer Fatoumata’s decision to join the Youth Action Movement was fueled by a personal loss. “My parents are educated, so me and my sisters were never cut. I learned about female genital mutilation at a conference I attended in 2016. I didn’t know that there were different types of severity and ways that girls could be cut. I hadn’t understood quite how dangerous this practice is. Two years ago, I lost my friend Aïssata. She got married young, at 17. She struggled to conceive until she was 23. The day she gave birth, there were complications and she died. The doctors said that the excision was botched and that’s what killed her. From that day on, I decided I needed to teach all the girls in my community about how harmful this practice is for their health. I was so horrified by the way she died.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Using dance and comedy to talk about sex Abdoulaye Camara, Head of AMPPF dance troupe Abdoulaye’s moves are not just for fun. He is head of the dance troupe of the AMPPF’s Youth Action Movement, which uses dance and comedy sketches to talk about sex. It’s a canny way to deliver messages about everything from using condoms to taking counterfeit antibiotics, to an audience who are often confused and ashamed about such topics. “We distract them with dance and humour and then we transmit those important messages about sex without offending them,” explained Abdoulaye. “We show them that it’s not to insult them or show them up, but just to explain how these things happen.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Determination to graduate Aminata Sonogo, student Sitting at a wooden school desk at 22, Sonogo is older than most of her classmates, but she shrugs off the looks and comments. She has fought hard to be here. “I wanted to go to high school but I needed to pass some exams to get here. In the end, it took me three years,” she said.At the start of her final year of collège, or middle school, Sonogo got pregnant. She went back to school in the autumn, 18 months after Fatoumata’s birth and with more determination than ever. At the end of the academic year, it paid off. “I did it. I passed my exams and now I am in high school,” Sonogo said, smiling and relaxing her shoulders. She is guided by visits from the AMPPF youth volunteers and shares her own story with classmates who she sees at risk of an unwanted pregnancy. Share on Twitter Share on Facebook Share via WhatsApp Share via Email AMPPF’s mobile clinic offers a lifeline to remote communities Mariame Doumbia, midwife “I work at a mobile clinic. It’s important for accessibility, so that the women living in poorly serviced areas can access sexual and reproductive health services, and reliable information.I like what I do. I like helping people, especially the young ones. They know I am always on call to help them, and even if I don’t know the answer at that moment, I will find out. I like everything about my work. Actually, it’s not just work for me, and I became a midwife for that reason. I’ve always been an educator on these issues in my community.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Trust underpins the relationship between AMPPF’s mobile team and the village of Missala Adama Samaké, village elder and chief of the Missala Health Center Adama Samaké, chief of the Missala Health Center, oversees the proceedings as a village elder with deep trust from his community. When the mobile clinic isn’t around, his center offers maternity services and treats the many cases of malaria that are diagnosed in the community. “Given the distance between here and Bamako, most of the villagers around here rely on us for treatment,” he said. “But when we announce that the mobile clinic is coming, the women make sure they are here.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Contraceptive choice Kadidiatou Sogoba, client Kadidiatou Sogoba, a mother of seven, waited nervously for her turn. “I came today because I keep getting ill and I have felt very weak, just not myself, since I had a Caesarean section three years ago. I lost a lot of blood,” she said. “I have been very afraid since the birth of my last child. We have been using condoms and we were getting a bit tired of them, so I am looking for another longer-term type of contraception.”After emerging half an hour later, Sogoba clutched a packet of the contraceptive pill, and said next time she would go for a cervical screening.Photos ©IPPF/Xaume Olleros/Mali Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 16 May 2025
In pictures: Overcoming the impact of the Global Gag Rule in Mali
In 2017, the Association Malienne pour la Protection et la Promotion de la Famille (AMPPF), was hit hard by the reinstatement of the Global Gag Rule (GGR). The impact was swift and devastating – depleted budgets meant that AMPPF had to cut back on key staff and suspend education activities and community healthcare provision. The situation turned around with funding from the Canadian Government supporting the SheDecides project, filling the gap left by GGR. AMPPF has been able to employ staff ensuring their team can reach the most vulnerable clients who would otherwise be left without access to sexual healthcare and increase their outreach to youth. Putting communities first Mama Keita Sy Diallo, midwife The SheDecides project has allowed AMPPF to maintain three mobile clinics, travelling to more remote areas where transportation costs and huge distances separate women from access to health and contraceptive care.“SheDecides has helped us a lot, above all in our work outside our own permanent clinics. When we go out in the community we have a lot of clients, and many women come to us who would otherwise not have the means to obtain advice or contraception,” explained Mama Keita Sy Diallo, a midwife and AMPPF board member. She runs consultations at community health centers in underserved areas of the Malian capital. “Everything is free for the women in these sessions.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email SheDecides projects ensures free access to healthcare and contraception Fatoumata Dramé, client By 9am at the Asaco Sekasi community health center in Bamako, its wooden benches are full of clients waiting their turn at a SheDecides outreach session. Fatoumata Dramé, 30, got here early and has already been fitted for a new implant. “I came here for family planning, and it’s my first time. I’ve just moved to the area so I came because it’s close to home,” she said. Bouncing two-month-old Tiemoko on her knee, Dramé said her main motivation was to space the births of her children. “I am a mum of three now. My first child is 7 years old. I try to leave three years between each child. It helps with my health,” she explained. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Targeting youth Mamadou Bah, Youth Action Movement “After the arrival of SheDecides, we intensified our targeting of vulnerable groups with activities in the evening, when domestic workers and those working during the day could attend,” said Mariam Modibo Tandina, who heads the national committee of the Youth Action Movement in Mali. “That means that young people in precarious situations could learn more about safer sex and family planning. Now they know how to protect themselves against sexually transmitted infections and unwanted pregnancies.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Speaking out against FGM Fatoumata Yehiya Maiga, youth volunteer Fatoumata’s decision to join the Youth Action Movement was fueled by a personal loss. “My parents are educated, so me and my sisters were never cut. I learned about female genital mutilation at a conference I attended in 2016. I didn’t know that there were different types of severity and ways that girls could be cut. I hadn’t understood quite how dangerous this practice is. Two years ago, I lost my friend Aïssata. She got married young, at 17. She struggled to conceive until she was 23. The day she gave birth, there were complications and she died. The doctors said that the excision was botched and that’s what killed her. From that day on, I decided I needed to teach all the girls in my community about how harmful this practice is for their health. I was so horrified by the way she died.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Using dance and comedy to talk about sex Abdoulaye Camara, Head of AMPPF dance troupe Abdoulaye’s moves are not just for fun. He is head of the dance troupe of the AMPPF’s Youth Action Movement, which uses dance and comedy sketches to talk about sex. It’s a canny way to deliver messages about everything from using condoms to taking counterfeit antibiotics, to an audience who are often confused and ashamed about such topics. “We distract them with dance and humour and then we transmit those important messages about sex without offending them,” explained Abdoulaye. “We show them that it’s not to insult them or show them up, but just to explain how these things happen.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Determination to graduate Aminata Sonogo, student Sitting at a wooden school desk at 22, Sonogo is older than most of her classmates, but she shrugs off the looks and comments. She has fought hard to be here. “I wanted to go to high school but I needed to pass some exams to get here. In the end, it took me three years,” she said.At the start of her final year of collège, or middle school, Sonogo got pregnant. She went back to school in the autumn, 18 months after Fatoumata’s birth and with more determination than ever. At the end of the academic year, it paid off. “I did it. I passed my exams and now I am in high school,” Sonogo said, smiling and relaxing her shoulders. She is guided by visits from the AMPPF youth volunteers and shares her own story with classmates who she sees at risk of an unwanted pregnancy. Share on Twitter Share on Facebook Share via WhatsApp Share via Email AMPPF’s mobile clinic offers a lifeline to remote communities Mariame Doumbia, midwife “I work at a mobile clinic. It’s important for accessibility, so that the women living in poorly serviced areas can access sexual and reproductive health services, and reliable information.I like what I do. I like helping people, especially the young ones. They know I am always on call to help them, and even if I don’t know the answer at that moment, I will find out. I like everything about my work. Actually, it’s not just work for me, and I became a midwife for that reason. I’ve always been an educator on these issues in my community.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Trust underpins the relationship between AMPPF’s mobile team and the village of Missala Adama Samaké, village elder and chief of the Missala Health Center Adama Samaké, chief of the Missala Health Center, oversees the proceedings as a village elder with deep trust from his community. When the mobile clinic isn’t around, his center offers maternity services and treats the many cases of malaria that are diagnosed in the community. “Given the distance between here and Bamako, most of the villagers around here rely on us for treatment,” he said. “But when we announce that the mobile clinic is coming, the women make sure they are here.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Contraceptive choice Kadidiatou Sogoba, client Kadidiatou Sogoba, a mother of seven, waited nervously for her turn. “I came today because I keep getting ill and I have felt very weak, just not myself, since I had a Caesarean section three years ago. I lost a lot of blood,” she said. “I have been very afraid since the birth of my last child. We have been using condoms and we were getting a bit tired of them, so I am looking for another longer-term type of contraception.”After emerging half an hour later, Sogoba clutched a packet of the contraceptive pill, and said next time she would go for a cervical screening.Photos ©IPPF/Xaume Olleros/Mali Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 23 January 2019
“Since the closure of the clinic ... we encounter a lot more problems in our area"
Senegal’s IPPF Member Association, Association Sénégalaise pour le Bien-Etre Familial (ASBEF) ran two clinics in the capital, Dakar, until funding was cut in 2017 due to the reinstatement of the Global Gag Rule (GGR) by the US administration. The ASBEF clinic in the struggling suburb of Guediawaye was forced to close as a result of the GGR, leaving just the main headquarters in the heart of the city. The GGR prohibits foreign non-governmental organizations (NGOs) who receive US assistance from providing abortion care services, even with the NGO’s non-US funds. Abortion is illegal in Senegal except when three doctors agree the procedure is required to save a mother’s life. ASBEF applied for emergency funds and now offers an alternative service to the population of Guediawaye, offering sexual and reproductive health services through pop-up clinics. Asba Hann is the president of the Guediawaye chapter of IPPF’s Africa region youth action movement. She explains how the Global Gag Rule (GGR) cuts have deprived youth of a space to ask questions about their sexuality and seek advice on contraception. “Since the closure of the clinic, the nature of our advocacy has changed. We encounter a lot more problems in our area, above all from young people and women asking for services. ASBEF (Association Sénégalaise pour le Bien-Etre Familial) was a little bit less expensive for them and in this suburb there is a lot of poverty. Our facilities as volunteers also closed. We offer information to young people but since the closure of the clinic and our space they no longer get it in the same way, because they used to come and visit us. We still do activities but it’s difficult to get the information out, so young people worry about their sexual health and can’t get the confirmation needed for their questions. Young people don’t want to be seen going to a pharmacy and getting contraception, at risk of being seen by members of the community. They preferred seeing a midwife, discreetly, and to obtain their contraception privately. Young people often also can’t afford the contraception in the clinics and pharmacies. It would be much easier for us to have a specific place to hold events with the midwives who could then explain things to young people. A lot of the teenagers here still aren’t connected to the internet and active on social media. Others work all day and can’t look at their phones, and announcements get lost when they look at all their messages at night. Being on the ground is the best way for us to connect to young people.”

| 16 May 2025
“Since the closure of the clinic ... we encounter a lot more problems in our area"
Senegal’s IPPF Member Association, Association Sénégalaise pour le Bien-Etre Familial (ASBEF) ran two clinics in the capital, Dakar, until funding was cut in 2017 due to the reinstatement of the Global Gag Rule (GGR) by the US administration. The ASBEF clinic in the struggling suburb of Guediawaye was forced to close as a result of the GGR, leaving just the main headquarters in the heart of the city. The GGR prohibits foreign non-governmental organizations (NGOs) who receive US assistance from providing abortion care services, even with the NGO’s non-US funds. Abortion is illegal in Senegal except when three doctors agree the procedure is required to save a mother’s life. ASBEF applied for emergency funds and now offers an alternative service to the population of Guediawaye, offering sexual and reproductive health services through pop-up clinics. Asba Hann is the president of the Guediawaye chapter of IPPF’s Africa region youth action movement. She explains how the Global Gag Rule (GGR) cuts have deprived youth of a space to ask questions about their sexuality and seek advice on contraception. “Since the closure of the clinic, the nature of our advocacy has changed. We encounter a lot more problems in our area, above all from young people and women asking for services. ASBEF (Association Sénégalaise pour le Bien-Etre Familial) was a little bit less expensive for them and in this suburb there is a lot of poverty. Our facilities as volunteers also closed. We offer information to young people but since the closure of the clinic and our space they no longer get it in the same way, because they used to come and visit us. We still do activities but it’s difficult to get the information out, so young people worry about their sexual health and can’t get the confirmation needed for their questions. Young people don’t want to be seen going to a pharmacy and getting contraception, at risk of being seen by members of the community. They preferred seeing a midwife, discreetly, and to obtain their contraception privately. Young people often also can’t afford the contraception in the clinics and pharmacies. It would be much easier for us to have a specific place to hold events with the midwives who could then explain things to young people. A lot of the teenagers here still aren’t connected to the internet and active on social media. Others work all day and can’t look at their phones, and announcements get lost when they look at all their messages at night. Being on the ground is the best way for us to connect to young people.”

| 23 January 2019
“Since the clinic closed in this town everything has been very difficult"
Senegal’s IPPF Member Association, Association Sénégalaise pour le Bien-Etre Familial (ASBEF) ran two clinics in the capital, Dakar, until funding was cut in 2017 due to the reinstatement of the Global Gag Rule (GGR) by the US administration. The ASBEF clinic in the struggling suburb of Guediawaye was forced to close as a result of the GGR, leaving just the main headquarters in the heart of the city. The GGR prohibits foreign non-governmental organizations (NGOs) who receive US assistance from providing abortion care services, even with the NGO’s non-US funds. Abortion is illegal in Senegal except when three doctors agree the procedure is required to save a mother’s life. ASBEF applied for emergency funds and now offers an alternative service to the population of Guediawaye, offering sexual and reproductive health services through pop-up clinics. Betty Guèye is a midwife who used to live in Guediawaye but moved to Dakar after the closure of the clinic in the suburb of Senegal’s capital following global gag rule (GGR) funding cuts. She describes the effects of the closure and how Association Sénégalaise pour le Bien-Etre Familial (ASBEF) staff try to maximise the reduced service they still offer. “Since the clinic closed in this town everything has been very difficult. The majority of Senegalese are poor and we are losing clients because they cannot access the main clinic in Dakar. If they have an appointment on a Monday, after the weekend they won’t have the 200 francs (35 US cents) needed for the bus, and they will wait until Tuesday or Wednesday to come even though they are in pain. The clinic was of huge benefit to the community of Guediawaye and the surrounding suburbs as well. What we see now is that women wait until pain or infections are at a more advanced stage before they visit us in Dakar. Another effect is that if they need to update their contraception they will exceed the date required for the new injection or pill and then get pregnant as a result. In addition, raising awareness of sexual health in schools and neighbourhoods is a key part of our work. Religion and the lack of openness in the parent-child relationship inhibit these conversations in Senegal, and so young people don’t tell their parents when they have sexual health problems. We were very present in this area and now we only appear much more rarely in their lives, which has had negative consequences for the health of our young people. If we were still there as before, there would be fewer teenage pregnancies as well, with the advice and contraception that we provide. However, we hand out medication, we care for the community and we educate them when we can, when we are here and we have the money to do so. Our prices remain the same and they are competitive compared with the private clinics and pharmacies in the area. Young people will tell you that they are closer to the midwives and nurses here than to their parents. They can tell them anything. If a girl tells me she has had sex I can give her the morning after pill, but if she goes to the local health center she may feel she is being watched by her neighbours.” Ndeye Yacine Touré is a midwife who regularly fields calls from young women in Guediawaye seeking advice on their sexual health, and who no longer know where to turn. The closure of the Association Sénégalaise pour le Bien-Etre Familial (ASBEF) clinic in their area has left them seeking often desperate solutions to the taboo of having a child outside of marriage. “Many of our colleagues lost their jobs, and these were people who were supporting their families. It was a loss for the area as a whole, because this is a very poor neighbourhood where people don’t have many options in life. ASBEF Guediawaye was their main source of help because they came here for consultations but also for confidential advice. The services we offer at ASBEF are special, in a way, especially in the area of family planning. Women were at ease at the clinic, but since then there is a gap in their lives. The patients call us day and night wanting advice, asking how to find the main clinic in Dakar. Some say they no longer get check-ups or seek help because they lack the money to go elsewhere. Others say they miss certain midwives or nurses. We make use of emergency funds in several ways. We do pop-up events. I also give them my number and tell them how to get to the clinic in central Dakar, and reassure them that it will all be confidential and that they can seek treatment there. In Senegal, a girl having sex outside marriage isn’t accepted. Some young women were taking contraception secretly, but since the closure of the clinic it’s no longer possible. Some of them got pregnant as a result. They don’t want to bump into their mother at the public clinic so they just stop taking contraception. In Senegal, a girl having sex outside marriage isn’t accepted. The impact on young people is particularly serious. Some tell me they know they have a sexually transmitted infection but they are too afraid to go to the hospital and get it treated. Before they could talk to us and tell us that they had sex, and we could help them. They have to hide now and some seek unsafe abortions. ”

| 16 May 2025
“Since the clinic closed in this town everything has been very difficult"
Senegal’s IPPF Member Association, Association Sénégalaise pour le Bien-Etre Familial (ASBEF) ran two clinics in the capital, Dakar, until funding was cut in 2017 due to the reinstatement of the Global Gag Rule (GGR) by the US administration. The ASBEF clinic in the struggling suburb of Guediawaye was forced to close as a result of the GGR, leaving just the main headquarters in the heart of the city. The GGR prohibits foreign non-governmental organizations (NGOs) who receive US assistance from providing abortion care services, even with the NGO’s non-US funds. Abortion is illegal in Senegal except when three doctors agree the procedure is required to save a mother’s life. ASBEF applied for emergency funds and now offers an alternative service to the population of Guediawaye, offering sexual and reproductive health services through pop-up clinics. Betty Guèye is a midwife who used to live in Guediawaye but moved to Dakar after the closure of the clinic in the suburb of Senegal’s capital following global gag rule (GGR) funding cuts. She describes the effects of the closure and how Association Sénégalaise pour le Bien-Etre Familial (ASBEF) staff try to maximise the reduced service they still offer. “Since the clinic closed in this town everything has been very difficult. The majority of Senegalese are poor and we are losing clients because they cannot access the main clinic in Dakar. If they have an appointment on a Monday, after the weekend they won’t have the 200 francs (35 US cents) needed for the bus, and they will wait until Tuesday or Wednesday to come even though they are in pain. The clinic was of huge benefit to the community of Guediawaye and the surrounding suburbs as well. What we see now is that women wait until pain or infections are at a more advanced stage before they visit us in Dakar. Another effect is that if they need to update their contraception they will exceed the date required for the new injection or pill and then get pregnant as a result. In addition, raising awareness of sexual health in schools and neighbourhoods is a key part of our work. Religion and the lack of openness in the parent-child relationship inhibit these conversations in Senegal, and so young people don’t tell their parents when they have sexual health problems. We were very present in this area and now we only appear much more rarely in their lives, which has had negative consequences for the health of our young people. If we were still there as before, there would be fewer teenage pregnancies as well, with the advice and contraception that we provide. However, we hand out medication, we care for the community and we educate them when we can, when we are here and we have the money to do so. Our prices remain the same and they are competitive compared with the private clinics and pharmacies in the area. Young people will tell you that they are closer to the midwives and nurses here than to their parents. They can tell them anything. If a girl tells me she has had sex I can give her the morning after pill, but if she goes to the local health center she may feel she is being watched by her neighbours.” Ndeye Yacine Touré is a midwife who regularly fields calls from young women in Guediawaye seeking advice on their sexual health, and who no longer know where to turn. The closure of the Association Sénégalaise pour le Bien-Etre Familial (ASBEF) clinic in their area has left them seeking often desperate solutions to the taboo of having a child outside of marriage. “Many of our colleagues lost their jobs, and these were people who were supporting their families. It was a loss for the area as a whole, because this is a very poor neighbourhood where people don’t have many options in life. ASBEF Guediawaye was their main source of help because they came here for consultations but also for confidential advice. The services we offer at ASBEF are special, in a way, especially in the area of family planning. Women were at ease at the clinic, but since then there is a gap in their lives. The patients call us day and night wanting advice, asking how to find the main clinic in Dakar. Some say they no longer get check-ups or seek help because they lack the money to go elsewhere. Others say they miss certain midwives or nurses. We make use of emergency funds in several ways. We do pop-up events. I also give them my number and tell them how to get to the clinic in central Dakar, and reassure them that it will all be confidential and that they can seek treatment there. In Senegal, a girl having sex outside marriage isn’t accepted. Some young women were taking contraception secretly, but since the closure of the clinic it’s no longer possible. Some of them got pregnant as a result. They don’t want to bump into their mother at the public clinic so they just stop taking contraception. In Senegal, a girl having sex outside marriage isn’t accepted. The impact on young people is particularly serious. Some tell me they know they have a sexually transmitted infection but they are too afraid to go to the hospital and get it treated. Before they could talk to us and tell us that they had sex, and we could help them. They have to hide now and some seek unsafe abortions. ”

| 22 January 2019
“I used to attend the clinic regularly and then one day I didn’t know what happened. The clinic just shut down"
Senegal’s IPPF Member Association, Association Sénégalaise pour le Bien-Etre Familial (ASBEF) ran two clinics in the capital, Dakar, until funding was cut in 2017 due to the reinstatement of the Global Gag Rule (GGR) by the US administration. The ASBEF clinic in the struggling suburb of Guediawaye was forced to close as a result of the GGR, leaving just the main headquarters in the heart of the city. The GGR prohibits foreign non-governmental organizations (NGOs) who receive US assistance from providing abortion care services, even with the NGO’s non-US funds. Abortion is illegal in Senegal except when three doctors agree the procedure is required to save a mother’s life. ASBEF applied for emergency funds and now offers an alternative service to the population of Guediawaye, offering sexual and reproductive health services through pop-up clinics. Maguette Mbow, a 33-year-old homemaker, describes how the closure of Association Sénégalaise pour le Bien-Etre Familial clinic in Guediawaye, a suburb of Dakar, has affected her, and explains the difficulties with the alternative providers available. She spoke about how the closure of her local clinic has impacted her life at a pop-up clinic set up for the day at a school in Guediawaye. “I heard that ASBEF (Association Sénégalaise pour le Bien-Etre Familial), was doing consultations here today and I dropped everything at home to come. There was a clinic here in Guediawaye but we don’t have it anymore. I’m here for family planning because that’s what I used to get at the clinic; it was their strong point. I take the Pill and I came to change the type I take, but the midwife advised me today to keep taking the same one. I’ve used the pill between my pregnancies. I have two children aged 2 and 6, but for now I’m not sure if I want a third child. When the clinic closed, I started going to the public facilities instead. There is always an enormous queue. You can get there in the morning and wait until 3pm for a consultation. (The closure) has affected everyone here very seriously. All my friends and family went to ASBEF Guediawaye, but now we are in the other public and private clinics receiving a really poor service. I had all of my pre-natal care at ASBEF and when I was younger I used the services for young people as well. They helped me take the morning after pill a few times and that really left its mark on me. They are great with young people; they are knowledgeable and really good with teenagers. There are still taboos surrounding sexuality in Senegal but they know how to handle them. These days, when ASBEF come to Guediawaye they have to set up in different places each time. It’s a bit annoying because if you know a place well and it’s full of well-trained people who you know personally, you feel more at ease. I would like things to go back to how they were before, and for the clinic to reopen. I would also have liked to send my children there one day when the time came, to benefit from the same service. Sometimes I travel right into Dakar for a consultation at the ASBEF headquarters, but often I don’t have the money.” Fatou Bimtou Diop, 20, is a final year student at Lycée Seydina Limamou Laye in Guediawaye. She explains why the closure of the Association Sénégalaise pour le Bien-Etre Familial clinic in her area in 2017 means she no longer regularly seeks advice on her sexual health. “I came here today for a consultation. I haven’t been for two years because the clinic closed. I don’t know why that happened but I would really like that decision to be reversed. Yes, there are other clinics here but I don’t feel as relaxed as with ASBEF (Association Sénégalaise pour le Bien-Etre Familial). I used to feel really at ease because there were other young people like me there. In the other clinics I know I might see someone’s mother or my aunties and it worries me too much. They explained things well and the set-up felt secure. We could talk about the intimate problems that were affecting us to the ASBEF staff. I went because I have really painful periods, for example. Sometimes I wouldn’t have the nerve to ask certain questions but my friends who went to the ASBEF clinic would ask and then tell me the responses that they got. These days we end up talking a lot about girls who are 14,15 years old who are pregnant. When the ASBEF clinic was there it was really rare to see a girl that young with a baby but now it happens very frequently. A friend’s younger sister has a little boy now and she had to have a caesarian section because she’s younger than us. The clinic in Dakar is too far away. I have to go to school during the day so I can’t take the time off. I came to the session today at school and it was good to discuss my problems, but it took quite a long time to get seen by a midwife.” Ngouye Cissé, a 30-year-old woman who gave birth to her first child in her early teens, but who has since used regular contraception provided by ASBEF (Association Sénégalaise pour le Bien-Etre Familial). She visits the association’s pop-up clinics whenever they are in Guediawaye. “I used to attend the clinic regularly and then one day I didn’t know what happened. The clinic just shut down. Senegal’s economic situation is difficult and we don’t have a lot of money. The fees for a consultation are quite expensive, but when ASBEF does come into the community it’s free. I most recently visited the pop-up clinic because I was having some vaginal discharge and I didn’t know why. The midwife took care of me and gave me some advice and medication. Before I came here for my check-up, the public hospital was asking me to do a lot of tests and I was afraid I had some kind of terrible disease. But when I came to the ASBEF midwife simply listened to me, explained what I had, and then gave me the right medication straight away. I feel really relieved. I’m divorced and I have three boys. I had pre-natal care with ASBEF for the first two pregnancies, but with the third, my 2-year-old son, I had to go to a public hospital. The experiences couldn’t be more different. First, there is a big difference in price, as ASBEF is much cheaper. Also, at the ASBEF clinic we are really listened to. The midwife explains things and gives me information. We can talk about our problems openly and without fear, unlike in other health centers. What I see now that the clinic has closed is a lot more pregnant young girls, problems with STIs and in order to get treatment we have to go to the public and private clinics. When people hear that ASBEF is back in town there is a huge rush to get a consultation, because the need is there but people don’t know where else to go. Unfortunately, the transport to go to the clinic in Dakar costs a lot of money for us that we don’t have. Some households don’t even have enough to eat. There isn’t a huge difference between the consultations in the old clinic and the pop-up events that ASBEF organize. They still listen to you properly and it’s well organized. It just takes longer to get seen.” Moudel Bassoum, a 22-year student studying NGO management in Dakar, explains why she has been unable to replace the welcome and care she received at the now closed Association Sénégalaise pour le Bien-Etre Familial clinic in her hometown of Guediawaye, but still makes us of the pop-up clinic when it is available. “I used to go to the clinic regularly but since it closed, we only see the staff rarely around here. I came with my friends today for a free check-up. I told the whole neighbourhood that ASBEF (Association Sénégalaise pour le Bien-Etre Familial) were doing a pop-up clinic today so that they could come for free consultations. It’s not easy to get to the main clinic in Dakar for us. The effects of the closure are numerous, especially on young people. It helped us so much but now I hear a lot more about teenage pregnancies and STIs, not to mention girls trying to abort pregnancies by themselves. When my friend had an infection she went all the way into Dakar for the consultation because the public clinic is more expensive. I would much rather talk to a woman about this type of problem and at the public clinic you don’t get to pick who you talk to. You have to say everything in front of everyone. I don’t think the service we receive since the closure is different when the ASBEF clinic set up here for the day, but the staff are usually not the same and it’s less frequent. It’s free so when they do come there are a lot of people. I would really like the clinic to be re-established when I have a baby one day. I want that welcome, and to know that they will listen to you.”

| 16 May 2025
“I used to attend the clinic regularly and then one day I didn’t know what happened. The clinic just shut down"
Senegal’s IPPF Member Association, Association Sénégalaise pour le Bien-Etre Familial (ASBEF) ran two clinics in the capital, Dakar, until funding was cut in 2017 due to the reinstatement of the Global Gag Rule (GGR) by the US administration. The ASBEF clinic in the struggling suburb of Guediawaye was forced to close as a result of the GGR, leaving just the main headquarters in the heart of the city. The GGR prohibits foreign non-governmental organizations (NGOs) who receive US assistance from providing abortion care services, even with the NGO’s non-US funds. Abortion is illegal in Senegal except when three doctors agree the procedure is required to save a mother’s life. ASBEF applied for emergency funds and now offers an alternative service to the population of Guediawaye, offering sexual and reproductive health services through pop-up clinics. Maguette Mbow, a 33-year-old homemaker, describes how the closure of Association Sénégalaise pour le Bien-Etre Familial clinic in Guediawaye, a suburb of Dakar, has affected her, and explains the difficulties with the alternative providers available. She spoke about how the closure of her local clinic has impacted her life at a pop-up clinic set up for the day at a school in Guediawaye. “I heard that ASBEF (Association Sénégalaise pour le Bien-Etre Familial), was doing consultations here today and I dropped everything at home to come. There was a clinic here in Guediawaye but we don’t have it anymore. I’m here for family planning because that’s what I used to get at the clinic; it was their strong point. I take the Pill and I came to change the type I take, but the midwife advised me today to keep taking the same one. I’ve used the pill between my pregnancies. I have two children aged 2 and 6, but for now I’m not sure if I want a third child. When the clinic closed, I started going to the public facilities instead. There is always an enormous queue. You can get there in the morning and wait until 3pm for a consultation. (The closure) has affected everyone here very seriously. All my friends and family went to ASBEF Guediawaye, but now we are in the other public and private clinics receiving a really poor service. I had all of my pre-natal care at ASBEF and when I was younger I used the services for young people as well. They helped me take the morning after pill a few times and that really left its mark on me. They are great with young people; they are knowledgeable and really good with teenagers. There are still taboos surrounding sexuality in Senegal but they know how to handle them. These days, when ASBEF come to Guediawaye they have to set up in different places each time. It’s a bit annoying because if you know a place well and it’s full of well-trained people who you know personally, you feel more at ease. I would like things to go back to how they were before, and for the clinic to reopen. I would also have liked to send my children there one day when the time came, to benefit from the same service. Sometimes I travel right into Dakar for a consultation at the ASBEF headquarters, but often I don’t have the money.” Fatou Bimtou Diop, 20, is a final year student at Lycée Seydina Limamou Laye in Guediawaye. She explains why the closure of the Association Sénégalaise pour le Bien-Etre Familial clinic in her area in 2017 means she no longer regularly seeks advice on her sexual health. “I came here today for a consultation. I haven’t been for two years because the clinic closed. I don’t know why that happened but I would really like that decision to be reversed. Yes, there are other clinics here but I don’t feel as relaxed as with ASBEF (Association Sénégalaise pour le Bien-Etre Familial). I used to feel really at ease because there were other young people like me there. In the other clinics I know I might see someone’s mother or my aunties and it worries me too much. They explained things well and the set-up felt secure. We could talk about the intimate problems that were affecting us to the ASBEF staff. I went because I have really painful periods, for example. Sometimes I wouldn’t have the nerve to ask certain questions but my friends who went to the ASBEF clinic would ask and then tell me the responses that they got. These days we end up talking a lot about girls who are 14,15 years old who are pregnant. When the ASBEF clinic was there it was really rare to see a girl that young with a baby but now it happens very frequently. A friend’s younger sister has a little boy now and she had to have a caesarian section because she’s younger than us. The clinic in Dakar is too far away. I have to go to school during the day so I can’t take the time off. I came to the session today at school and it was good to discuss my problems, but it took quite a long time to get seen by a midwife.” Ngouye Cissé, a 30-year-old woman who gave birth to her first child in her early teens, but who has since used regular contraception provided by ASBEF (Association Sénégalaise pour le Bien-Etre Familial). She visits the association’s pop-up clinics whenever they are in Guediawaye. “I used to attend the clinic regularly and then one day I didn’t know what happened. The clinic just shut down. Senegal’s economic situation is difficult and we don’t have a lot of money. The fees for a consultation are quite expensive, but when ASBEF does come into the community it’s free. I most recently visited the pop-up clinic because I was having some vaginal discharge and I didn’t know why. The midwife took care of me and gave me some advice and medication. Before I came here for my check-up, the public hospital was asking me to do a lot of tests and I was afraid I had some kind of terrible disease. But when I came to the ASBEF midwife simply listened to me, explained what I had, and then gave me the right medication straight away. I feel really relieved. I’m divorced and I have three boys. I had pre-natal care with ASBEF for the first two pregnancies, but with the third, my 2-year-old son, I had to go to a public hospital. The experiences couldn’t be more different. First, there is a big difference in price, as ASBEF is much cheaper. Also, at the ASBEF clinic we are really listened to. The midwife explains things and gives me information. We can talk about our problems openly and without fear, unlike in other health centers. What I see now that the clinic has closed is a lot more pregnant young girls, problems with STIs and in order to get treatment we have to go to the public and private clinics. When people hear that ASBEF is back in town there is a huge rush to get a consultation, because the need is there but people don’t know where else to go. Unfortunately, the transport to go to the clinic in Dakar costs a lot of money for us that we don’t have. Some households don’t even have enough to eat. There isn’t a huge difference between the consultations in the old clinic and the pop-up events that ASBEF organize. They still listen to you properly and it’s well organized. It just takes longer to get seen.” Moudel Bassoum, a 22-year student studying NGO management in Dakar, explains why she has been unable to replace the welcome and care she received at the now closed Association Sénégalaise pour le Bien-Etre Familial clinic in her hometown of Guediawaye, but still makes us of the pop-up clinic when it is available. “I used to go to the clinic regularly but since it closed, we only see the staff rarely around here. I came with my friends today for a free check-up. I told the whole neighbourhood that ASBEF (Association Sénégalaise pour le Bien-Etre Familial) were doing a pop-up clinic today so that they could come for free consultations. It’s not easy to get to the main clinic in Dakar for us. The effects of the closure are numerous, especially on young people. It helped us so much but now I hear a lot more about teenage pregnancies and STIs, not to mention girls trying to abort pregnancies by themselves. When my friend had an infection she went all the way into Dakar for the consultation because the public clinic is more expensive. I would much rather talk to a woman about this type of problem and at the public clinic you don’t get to pick who you talk to. You have to say everything in front of everyone. I don’t think the service we receive since the closure is different when the ASBEF clinic set up here for the day, but the staff are usually not the same and it’s less frequent. It’s free so when they do come there are a lot of people. I would really like the clinic to be re-established when I have a baby one day. I want that welcome, and to know that they will listen to you.”