Spotlight
A selection of stories from across the Federation

Advances in Sexual and Reproductive Rights and Health: 2024 in Review
Let’s take a leap back in time to the beginning of 2024: In twelve months, what victories has our movement managed to secure in the face of growing opposition and the rise of the far right? These victories for sexual and reproductive rights and health are the result of relentless grassroots work and advocacy by our Member Associations, in partnership with community organizations, allied politicians, and the mobilization of public opinion.
Most Popular This Week

Advances in Sexual and Reproductive Rights and Health: 2024 in Review
Let’s take a leap back in time to the beginning of 2024: In twelve months, what victories has our movement managed to secure in t
Kazakhstan

Kazakhstan's Rising HIV Crisis: A Call for Action
On World AIDS Day, we commemorate the remarkable achievements of IPPF Member Associations in their unwavering commitment to combating the HIV epidemic.

Ensuring SRHR in Humanitarian Crises: What You Need to Know
Over the past two decades, global forced displacement has consistently increased, affecting an estimated 114 million people as of mid-2023.
Estonia, Nepal, Namibia, Japan, Thailand

The Rainbow Wave for Marriage Equality
Love wins! The fight for marriage equality has seen incredible progress worldwide, with a recent surge in legalizations.
France, Germany, Poland, United Kingdom, United States, Colombia, India, Tunisia

Abortion Rights: Latest Decisions and Developments around the World
Over the past 30 years, more than

Palestine

In their own words: The people providing sexual and reproductive health care under bombardment in Gaza
Week after week, heavy Israeli bombardment from air, land, and sea, has continued across most of the Gaza Strip.
Vanuatu

When getting to the hospital is difficult, Vanuatu mobile outreach can save lives
In the mountains of Kumera on Tanna Island, Vanuatu, the village women of Kamahaul normally spend over 10,000 Vatu ($83 USD) to travel to the nearest hospital.
Filter our stories by:
- Afghanistan
- Albania
- Aruba
- Bangladesh
- Benin
- Botswana
- Burundi
- (-) Cambodia
- Cameroon
- Colombia
- Congo, Dem. Rep.
- Cook Islands
- El Salvador
- Estonia
- Ethiopia
- Fiji
- France
- Germany
- Ghana
- Guinea-Conakry
- India
- Ireland
- Jamaica
- Japan
- Kazakhstan
- Kenya
- (-) Kiribati
- Lesotho
- Malawi
- Mali
- Mozambique
- Namibia
- Nepal
- Nigeria
- Pakistan
- Palestine
- Poland
- Senegal
- Somaliland
- Sri Lanka
- Sudan
- Thailand
- Togo
- Tonga
- Trinidad and Tobago
- Tunisia
- Uganda
- United Kingdom
- United States
- Vanuatu
- Zambia


| 18 June 2020
In pictures: Healthcare in the face of the climate crisis in Kiribati
Humanitarian crises Largely brought on by sudden onset and slow-onset natural disasters, humanitarian crises are increasingly prevalent in the Pacific. During responses to humanitarian crises in the Pacific, sexual and reproductive healthcare is often under-prioritised and under-resourced. As a result, women and girls of reproductive age and vulnerable and marginalized groups are disproportionately affected and facing increased health and psychosocial risks. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Fragile environments Low topography, rising sea levels and insufficient fresh water supply leaves Kiribati’s population vulnerable to the effects of the climate crisis. The fragility of the outer islands of Kiribati during natural disasters is compounded by their geographic isolation, which makes transportation and communication during post-disaster relief and response both expensive and difficult. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Coastal exposure The majority of the population of 115,000 people live a subsistence lifestyle. Communities are geographically dispersed across 33 atolls covering 3.5 million square kilometres in the central Pacific Ocean. The population and infrastructure within Kiribati are largely concentrated on the coast, where communities face increased exposure to climate threats and natural hazards such as tsunamis, earthquakes, king tides, flooding, droughts, and occasionally cyclones. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Takaria, leader and youth organizer in the Tebikenikua community Takaria will be running to be a Member of Parliament in Kiribati in 2020. “I assist the youth with family problems and family planning and disasters. In our community there are unforeseen pregnancies, domestic violence, and disasters such as high tide waters and strong winds, which can also affect this community. The Kiribati Family Health Association (KFHA) is the key point for us with outreach and training so people in this community know how to prevent and treat STIs, etc. They all know where the KFHA clinic is and that they can get counselling or services there. The problem now is you can’t survive with the sea rise levels. I want all members of my community to live better and have better health and peace.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Susan*, sex worker Susan receives care at the Kiribati Family Health Association (KFHA) including a pap smear. Susan*, 28, is a sex worker from the town of Betio on the main island of Kiribati. Originally from an outlying island, she moved into Tarawa to seek work. Unable to find employment that would fulfill her dream of sending money back to her two children, she was introduced to sex work. With other sex workers, she regularly travels out to the large cargo ships from China, Philippines and Korea anchored off the coast of Kiribati. Despite her new income, she still can’t speak with her children or see them due to the restrictive costs involved of travel between islands.*pseudonym Share on Twitter Share on Facebook Share via WhatsApp Share via Email Theta, 25-year-old mother and youth volunteer Theta is part of the Humanitarian Youth Club set up by the Kiribati Family Health Association in her village. “We face a lot of situations here, one of them is disasters and the second is unemployment and school drop out with our youth. I have helped the Humanitarian Youth Club to apply for financial grants from the Australian High Commission [for $1,000] I am recognized as the smartest member who can write in English. We have learned how to design a disaster plan for the community and share our ideas on sexual and reproductive issues such as STIs. We discuss what we can do for the next strong tide, where we can gather as a community and what we can do if even the maneabe (town hall) floods? If the tide and wind is too strong, we need to go to another safer place, such as another community’s town hall. For now, I want to enjoy the chance to be in our own beloved country. I won’t move until the majority have already left. I want my daughter to grow up in the same place I grew up in.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Beitau, youth volunteer Beitau is the Chairperson of the Humanitarian Youth Club. “I was lucky to be selected as Chairperson as the Humanitarian Youth Club. I feel like I get more respect from the community now I am in this position. I would love advanced training on leadership now, to further assist the club. As I am the Chairperson of the HYC, my main target is to help people during a disaster. I have attended training through KFHA. What I took from this is that when a disaster strikes, we have to do our best for pregnant women, small children and people with disabilities. They more vulnerable and less able to survive a disaster.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Abe, youth officer Abe was involved with KFHA since 2012. “I was inspired by what they KFHA was doing and the issues they were addressing that affects youth. I was surprised to see how many young people come to the clinic as they are affected by STIs, HIV and teenage pregnancy. The lack of education here is a big problem, most people here have a lot of children and yet can’t afford to send them to school. Sexual and reproductive health is our responsibility and we must talk about it with young people. Climate change affects many countries, but Kiribati is small and low lying. I used to go visit a very nice beach with a lot of nice trees and plants. Now, the trees are gone, and the waves have taken over, and the houses have disappeared so no one can build there. In my role as a youth worker and activist, I tell people to fight climate change: to grow more mangroves, to clean up the beach, because we love our Kiribati.”©IPPF/Hannah Maule-Ffinch/Kiribati Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 17 May 2025
In pictures: Healthcare in the face of the climate crisis in Kiribati
Humanitarian crises Largely brought on by sudden onset and slow-onset natural disasters, humanitarian crises are increasingly prevalent in the Pacific. During responses to humanitarian crises in the Pacific, sexual and reproductive healthcare is often under-prioritised and under-resourced. As a result, women and girls of reproductive age and vulnerable and marginalized groups are disproportionately affected and facing increased health and psychosocial risks. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Fragile environments Low topography, rising sea levels and insufficient fresh water supply leaves Kiribati’s population vulnerable to the effects of the climate crisis. The fragility of the outer islands of Kiribati during natural disasters is compounded by their geographic isolation, which makes transportation and communication during post-disaster relief and response both expensive and difficult. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Coastal exposure The majority of the population of 115,000 people live a subsistence lifestyle. Communities are geographically dispersed across 33 atolls covering 3.5 million square kilometres in the central Pacific Ocean. The population and infrastructure within Kiribati are largely concentrated on the coast, where communities face increased exposure to climate threats and natural hazards such as tsunamis, earthquakes, king tides, flooding, droughts, and occasionally cyclones. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Takaria, leader and youth organizer in the Tebikenikua community Takaria will be running to be a Member of Parliament in Kiribati in 2020. “I assist the youth with family problems and family planning and disasters. In our community there are unforeseen pregnancies, domestic violence, and disasters such as high tide waters and strong winds, which can also affect this community. The Kiribati Family Health Association (KFHA) is the key point for us with outreach and training so people in this community know how to prevent and treat STIs, etc. They all know where the KFHA clinic is and that they can get counselling or services there. The problem now is you can’t survive with the sea rise levels. I want all members of my community to live better and have better health and peace.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Susan*, sex worker Susan receives care at the Kiribati Family Health Association (KFHA) including a pap smear. Susan*, 28, is a sex worker from the town of Betio on the main island of Kiribati. Originally from an outlying island, she moved into Tarawa to seek work. Unable to find employment that would fulfill her dream of sending money back to her two children, she was introduced to sex work. With other sex workers, she regularly travels out to the large cargo ships from China, Philippines and Korea anchored off the coast of Kiribati. Despite her new income, she still can’t speak with her children or see them due to the restrictive costs involved of travel between islands.*pseudonym Share on Twitter Share on Facebook Share via WhatsApp Share via Email Theta, 25-year-old mother and youth volunteer Theta is part of the Humanitarian Youth Club set up by the Kiribati Family Health Association in her village. “We face a lot of situations here, one of them is disasters and the second is unemployment and school drop out with our youth. I have helped the Humanitarian Youth Club to apply for financial grants from the Australian High Commission [for $1,000] I am recognized as the smartest member who can write in English. We have learned how to design a disaster plan for the community and share our ideas on sexual and reproductive issues such as STIs. We discuss what we can do for the next strong tide, where we can gather as a community and what we can do if even the maneabe (town hall) floods? If the tide and wind is too strong, we need to go to another safer place, such as another community’s town hall. For now, I want to enjoy the chance to be in our own beloved country. I won’t move until the majority have already left. I want my daughter to grow up in the same place I grew up in.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Beitau, youth volunteer Beitau is the Chairperson of the Humanitarian Youth Club. “I was lucky to be selected as Chairperson as the Humanitarian Youth Club. I feel like I get more respect from the community now I am in this position. I would love advanced training on leadership now, to further assist the club. As I am the Chairperson of the HYC, my main target is to help people during a disaster. I have attended training through KFHA. What I took from this is that when a disaster strikes, we have to do our best for pregnant women, small children and people with disabilities. They more vulnerable and less able to survive a disaster.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Abe, youth officer Abe was involved with KFHA since 2012. “I was inspired by what they KFHA was doing and the issues they were addressing that affects youth. I was surprised to see how many young people come to the clinic as they are affected by STIs, HIV and teenage pregnancy. The lack of education here is a big problem, most people here have a lot of children and yet can’t afford to send them to school. Sexual and reproductive health is our responsibility and we must talk about it with young people. Climate change affects many countries, but Kiribati is small and low lying. I used to go visit a very nice beach with a lot of nice trees and plants. Now, the trees are gone, and the waves have taken over, and the houses have disappeared so no one can build there. In my role as a youth worker and activist, I tell people to fight climate change: to grow more mangroves, to clean up the beach, because we love our Kiribati.”©IPPF/Hannah Maule-Ffinch/Kiribati Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 17 November 2017
“The doctors have also been giving me advice on how to look after myself and the baby"
When garment worker Ny thought she might be pregnant with her first child, a home test kit quickly confirmed her suspicions. But the 23-year-old – who is originally from Takeo province but moved to Phnom Penh to take up a job in the garment industry – did not know where to go to seek prenatal care. After a cousin recommended that she visit a nearby Reproductive Health Association of Cambodia clinic, Ny took her relative’s advice – and has gone back eight times to date. “I come here every month to check on the baby,” she says, cradling her belly. “I had never been before I got pregnant.” During her visits to the medical clinic, Ny says, she has had a raft of standard tests and procedures as part of her prenatal care, including two ultrasounds, blood and urine tests, and vaccinations. “The doctors have also been giving me advice on how to look after myself and the baby [such as] to eat nutritious food and not to carry heavy things,” she says. As well as caring for the health of mother and unborn child, RHAC staff have also offered up valuable family planning information. “I did not know about how to plan to have children before I came to the clinic,” Ny says. “The doctors here told me that there are three different methods of [long-term] contraception: medication, an implant and an IUD.” Ny, who sews winter clothing at a factory while her husband also works in a nearby garment factory, says she was very glad to learn about her options. “This child was unplanned, but I don’t feel any regret because I had already been married for two years. But after having the baby I plan to use birth control, though I don’t know what method I will use,” she says. “I know that I don’t want to have another child straight away. It may be two or three years until I have the next one, as I want to wait until my family’s finances improve.”

| 16 May 2025
“The doctors have also been giving me advice on how to look after myself and the baby"
When garment worker Ny thought she might be pregnant with her first child, a home test kit quickly confirmed her suspicions. But the 23-year-old – who is originally from Takeo province but moved to Phnom Penh to take up a job in the garment industry – did not know where to go to seek prenatal care. After a cousin recommended that she visit a nearby Reproductive Health Association of Cambodia clinic, Ny took her relative’s advice – and has gone back eight times to date. “I come here every month to check on the baby,” she says, cradling her belly. “I had never been before I got pregnant.” During her visits to the medical clinic, Ny says, she has had a raft of standard tests and procedures as part of her prenatal care, including two ultrasounds, blood and urine tests, and vaccinations. “The doctors have also been giving me advice on how to look after myself and the baby [such as] to eat nutritious food and not to carry heavy things,” she says. As well as caring for the health of mother and unborn child, RHAC staff have also offered up valuable family planning information. “I did not know about how to plan to have children before I came to the clinic,” Ny says. “The doctors here told me that there are three different methods of [long-term] contraception: medication, an implant and an IUD.” Ny, who sews winter clothing at a factory while her husband also works in a nearby garment factory, says she was very glad to learn about her options. “This child was unplanned, but I don’t feel any regret because I had already been married for two years. But after having the baby I plan to use birth control, though I don’t know what method I will use,” she says. “I know that I don’t want to have another child straight away. It may be two or three years until I have the next one, as I want to wait until my family’s finances improve.”

| 16 November 2017
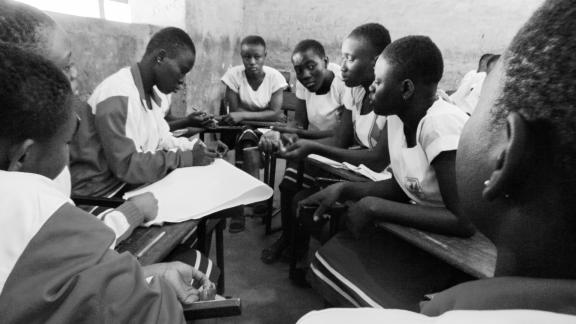
“When they don’t dare to ask questions about sensitive health topics, they don’t have the information they need"
Female workers, many of them undereducated migrants from rural areas, dominate the garment sector in Cambodia. And Propitious garment factory in Takhmao, a small city that lies just south of the capital Phnom Penh, is no exception. Women make up more than 90 percent of the factory’s workforce. Helping to oversee the 3,700-strong workforce is human resources manager Kouch Davy, who has worked at Propitious since it opened four years ago. Seeing a need to improve the workers’ sexual and reproductive health knowledge, she says she decided to work with the Reproductive Health Association of Cambodia (RHAC) because of its reputation for providing high-quality services. “I raised it in a management meeting, and the board was happy to explore it,” she says. For almost two years, trained staff from RHAC have been visiting the factory twice a month to meet with workers during their lunch break. They answer questions on topics ranging from birth control to STIs and abortion. The organisation has also provided training to the nurses who work in the factory’s on-site medical clinic. Davy says the factory’s female garment workers have changed as a result. “They are more open to asking questions about sexual health and they have also become more informed about the subject,” she says. “When they don’t dare to ask questions about sensitive health topics, they don’t have the information they need, so they tend to exaggerate their problems and ask for sick leave. But when they go to see an RHAC clinic and get proper treatment, there is less sick leave. “Now that they understand about contraception, there are fewer women getting pregnant and taking maternity leave, so that also helps with the workflow. ” Davy says the factory has seen requests for sick leave drop by an average of between 100 to 200 cases a month – and any decrease in absenteeism is a major boon for productivity. “The factory works like a chain: if just one person on the production line takes a day off, it affects the overall productivity,” she says. “And if a worker comes to work sick, they have problems concentrating.” Even Davy says she has gone to RHAC to seek medical care, visiting one of their clinics a few months ago for a breast examination. Meanwhile, the company that owns Propitious has extended its partnership with RHAC to a second factory in Phnom Penh. The firm has even requested that the NGO starts visiting its largest factory, which is situated in a rural province and has 10,000 workers, in the future.

| 16 May 2025
“When they don’t dare to ask questions about sensitive health topics, they don’t have the information they need"
Female workers, many of them undereducated migrants from rural areas, dominate the garment sector in Cambodia. And Propitious garment factory in Takhmao, a small city that lies just south of the capital Phnom Penh, is no exception. Women make up more than 90 percent of the factory’s workforce. Helping to oversee the 3,700-strong workforce is human resources manager Kouch Davy, who has worked at Propitious since it opened four years ago. Seeing a need to improve the workers’ sexual and reproductive health knowledge, she says she decided to work with the Reproductive Health Association of Cambodia (RHAC) because of its reputation for providing high-quality services. “I raised it in a management meeting, and the board was happy to explore it,” she says. For almost two years, trained staff from RHAC have been visiting the factory twice a month to meet with workers during their lunch break. They answer questions on topics ranging from birth control to STIs and abortion. The organisation has also provided training to the nurses who work in the factory’s on-site medical clinic. Davy says the factory’s female garment workers have changed as a result. “They are more open to asking questions about sexual health and they have also become more informed about the subject,” she says. “When they don’t dare to ask questions about sensitive health topics, they don’t have the information they need, so they tend to exaggerate their problems and ask for sick leave. But when they go to see an RHAC clinic and get proper treatment, there is less sick leave. “Now that they understand about contraception, there are fewer women getting pregnant and taking maternity leave, so that also helps with the workflow. ” Davy says the factory has seen requests for sick leave drop by an average of between 100 to 200 cases a month – and any decrease in absenteeism is a major boon for productivity. “The factory works like a chain: if just one person on the production line takes a day off, it affects the overall productivity,” she says. “And if a worker comes to work sick, they have problems concentrating.” Even Davy says she has gone to RHAC to seek medical care, visiting one of their clinics a few months ago for a breast examination. Meanwhile, the company that owns Propitious has extended its partnership with RHAC to a second factory in Phnom Penh. The firm has even requested that the NGO starts visiting its largest factory, which is situated in a rural province and has 10,000 workers, in the future.

| 16 November 2017
"During the pregnancy I was very worried”
Sophorn, a garment worker for the past decade, first visited a Reproductive Health Association of Cambodia (RHAC) clinic when she was pregnant with her first child. She returned for health checks each month until, at five months pregnant, she lost the baby. Her second pregnancy also resulted in a miscarriage, leaving her distraught. Then, she got pregnant a third time, in 2013. “I started to discuss with the doctors how to protect my child,” she says. “They gave me medication to strengthen my cervix, which I took for six months. In the seventh month, I gave birth prematurely.” Doctors told Sophorn that her baby girl was health, but she only weighed in at 1.7 kilograms. The infant was taken to a specialist children’s hospital, where she was cared for an additional two weeks. “During the pregnancy I was very worried,” Sophorn says. “I felt so happy when I finally delivered my child.” Her daughter was born without any complications is now a happy and healthy four years old. In initial stages of her third pregnancy, Sophorn’s friends told her that she would have to undergo surgery on her cervix or have injections to help her carry her baby to term, and doctors at a private clinic confirmed their suggestions. However, she decided to seek a second opinion at RHAC, where doctors instead gave her a prescription to strengthen her cervix. “When I heard I needed to have that surgery I was very scared, so I was relieved when the doctor at RHAC told me to take the medication instead,” she says. “While I was taking the medication I observed my body and any changes to it, so when I felt unwell I would go to the doctors and consult them, so I felt comfortable to continue taking it.” Sophorn also went for appointments at a government-run hospital, but found that their services were also lacking. “I told the doctors about losing my first and second babies, but they only weighed me and measured my stomach. There weren’t any more examinations or very much care,” she says. “When I went to RHAC they did so many examinations and had so many services, so I think it’s really better to go to RHAC for these kinds of services.” She estimates that during her third pregnancy, she had ten appointments at RHAC clinics at a cost of 40,000 to 60,000 riel (£7.40 to £11.15) each time. Compared to just 2,000 riel for an obstetrics appointment at the public hospital, the difference in cost is significant. “It’s expensive for me because my salary is little.” Despite the relatively high prices, Sophorn already knows where she will go for medical care in the future. “I want to have one more child, and I have already planned that when I decide to do it I will go to RHAC to get my cervix checked first,” she says. Until that day comes, Sophorn is taking the oral contraceptive after receiving advice about birth control from RHAC’s clinicians, with a midwife from the NGO making regular visits to the factory.

| 16 May 2025
"During the pregnancy I was very worried”
Sophorn, a garment worker for the past decade, first visited a Reproductive Health Association of Cambodia (RHAC) clinic when she was pregnant with her first child. She returned for health checks each month until, at five months pregnant, she lost the baby. Her second pregnancy also resulted in a miscarriage, leaving her distraught. Then, she got pregnant a third time, in 2013. “I started to discuss with the doctors how to protect my child,” she says. “They gave me medication to strengthen my cervix, which I took for six months. In the seventh month, I gave birth prematurely.” Doctors told Sophorn that her baby girl was health, but she only weighed in at 1.7 kilograms. The infant was taken to a specialist children’s hospital, where she was cared for an additional two weeks. “During the pregnancy I was very worried,” Sophorn says. “I felt so happy when I finally delivered my child.” Her daughter was born without any complications is now a happy and healthy four years old. In initial stages of her third pregnancy, Sophorn’s friends told her that she would have to undergo surgery on her cervix or have injections to help her carry her baby to term, and doctors at a private clinic confirmed their suggestions. However, she decided to seek a second opinion at RHAC, where doctors instead gave her a prescription to strengthen her cervix. “When I heard I needed to have that surgery I was very scared, so I was relieved when the doctor at RHAC told me to take the medication instead,” she says. “While I was taking the medication I observed my body and any changes to it, so when I felt unwell I would go to the doctors and consult them, so I felt comfortable to continue taking it.” Sophorn also went for appointments at a government-run hospital, but found that their services were also lacking. “I told the doctors about losing my first and second babies, but they only weighed me and measured my stomach. There weren’t any more examinations or very much care,” she says. “When I went to RHAC they did so many examinations and had so many services, so I think it’s really better to go to RHAC for these kinds of services.” She estimates that during her third pregnancy, she had ten appointments at RHAC clinics at a cost of 40,000 to 60,000 riel (£7.40 to £11.15) each time. Compared to just 2,000 riel for an obstetrics appointment at the public hospital, the difference in cost is significant. “It’s expensive for me because my salary is little.” Despite the relatively high prices, Sophorn already knows where she will go for medical care in the future. “I want to have one more child, and I have already planned that when I decide to do it I will go to RHAC to get my cervix checked first,” she says. Until that day comes, Sophorn is taking the oral contraceptive after receiving advice about birth control from RHAC’s clinicians, with a midwife from the NGO making regular visits to the factory.

| 16 November 2017
“Just yesterday during the outreach service, a woman asked me why she didn’t get her period after having an abortion..."
Pann Chandy gave her first sexual education lesson when she was still at school as a volunteer youth social worker with the Reproductive Health Association of Cambodia (RHAC). She had no qualms about standing up in front of her classmates to discuss culturally taboo topics when she was just a teenager. Now aged 25 and in possession of a Bachelor degree in midwifery, Chandy has been employed by RHAC for less than a year, working as part of the organisation’s health outreach team. The job is demanding: she is tasked with regularly visiting four karaoke parlours, eight garment factories and 20 villages in Phnom Penh, with plans to expand to two universities imminently. Travelling for hours A round trip to some communities can take two hours or more on her motorcycle, travelling alone into areas that are not always easily accessible. “Sometimes I have the clinic staff with me, but rarely,” Chandy says. “I promote the health services provided by Reproductive Health Association of Cambodia as well. If they are interested in going to a clinic, I give them a referral,” she says. One of the factories on her regular roster is Propitious garment factory in Takhmao, a small city south of Phnom Penh. Chandy spends two days a month at the factory, where she speaks to groups of women or has one-on-one discussions about sensitive topics. Passionate about the job “Just yesterday during the outreach service, a woman asked me why she didn’t get her period after having an abortion. She wanted to know what was wrong,” she says. “It’s common for women to use unsafe abortion methods. Mainly they take medicine from a pharmacy, and the pharmacy doesn’t give them any advice on how to use it. Often they go to cheap, unlicensed clinics near the factories for medical abortions.” Chandy is passionate about her job at Reproductive Health Association of Cambodia, and dreams about one day setting up her own pharmacy where she could provide comprehensive advice to clients. “There are a lot of unlicensed pharmacists in this country,” she says, many of which prescribe the counterfeit medicines that have inundated the market. “I think I may have the capacity to become a licensed one."

| 16 May 2025
“Just yesterday during the outreach service, a woman asked me why she didn’t get her period after having an abortion..."
Pann Chandy gave her first sexual education lesson when she was still at school as a volunteer youth social worker with the Reproductive Health Association of Cambodia (RHAC). She had no qualms about standing up in front of her classmates to discuss culturally taboo topics when she was just a teenager. Now aged 25 and in possession of a Bachelor degree in midwifery, Chandy has been employed by RHAC for less than a year, working as part of the organisation’s health outreach team. The job is demanding: she is tasked with regularly visiting four karaoke parlours, eight garment factories and 20 villages in Phnom Penh, with plans to expand to two universities imminently. Travelling for hours A round trip to some communities can take two hours or more on her motorcycle, travelling alone into areas that are not always easily accessible. “Sometimes I have the clinic staff with me, but rarely,” Chandy says. “I promote the health services provided by Reproductive Health Association of Cambodia as well. If they are interested in going to a clinic, I give them a referral,” she says. One of the factories on her regular roster is Propitious garment factory in Takhmao, a small city south of Phnom Penh. Chandy spends two days a month at the factory, where she speaks to groups of women or has one-on-one discussions about sensitive topics. Passionate about the job “Just yesterday during the outreach service, a woman asked me why she didn’t get her period after having an abortion. She wanted to know what was wrong,” she says. “It’s common for women to use unsafe abortion methods. Mainly they take medicine from a pharmacy, and the pharmacy doesn’t give them any advice on how to use it. Often they go to cheap, unlicensed clinics near the factories for medical abortions.” Chandy is passionate about her job at Reproductive Health Association of Cambodia, and dreams about one day setting up her own pharmacy where she could provide comprehensive advice to clients. “There are a lot of unlicensed pharmacists in this country,” she says, many of which prescribe the counterfeit medicines that have inundated the market. “I think I may have the capacity to become a licensed one."

| 16 November 2017
“I was very happy when my daughter was born”
After three years of marriage, Cambodian garment worker Sineang had started to wonder why she hadn’t yet become pregnant. Still in her early 20s, she and her husband wanted to have a baby and were not using contraception. In late 2011 or early 2012, Sineang visited a Reproductive Health Association of Cambodia clinic to seek treatment after she noticed some vaginal discharge. During the appointment, her doctor asked her more details about her sexual and reproductive health history: the issue of infertility soon came up. “I had been wanting to have a child for three years, since I was married,” she says. “I felt down about myself, but my husband gave me encouragement and told me it was okay that I was not pregnant yet.” During the initial examination, Sineang says, she was tested for cervical cancer as well as other reproductive health issues that can interfere with pregnancy. RHAC staff prescribed medication to treat her fertility problems, which she continued taking until they confirmed she was pregnant. “At first, I wasn’t really convinced that there was any relation between the discharge and not having a baby, but later I started to think that there was a connection,” she says. Throughout the whole period, Sineang went to RHAC each month – switching from infertility treatment to prenatal care – until she gave birth to a baby girl in 2013. “I was very happy when my daughter was born,” she says. “She’s healthy.” At the time, RHAC offered a discount to garment workers, which Sineang says was a big help. It’s no longer on offer, but she is an enthusiastic supporter of a plan RHAC is hoping to implement soon – a partnership with the National Social Security Fund that would allow them to visit RHAC clinics for free through the fund. “It would be really great if they could, because having a baby is expensive,” she says. “The clinic at RHAC has better service than the public hospitals. When I had my first baby, I wanted to have good service, because I had this problem with discharge [in the past].” Sineang, who is originally from Kandal province and works at Dewhirst garment factory in Phnom Penh, said she was pleased to see RHAC midwives doing regular outreach sessions at the factory. “It’s good for women to know more about these issues,” she says. And not only that, but Sineang is also an active ambassador for RHAC, spreading the word about the NGO’s services to friends and colleagues who have also struggled to have a baby. “I referred a friend to RHAC after she saw that I finally got pregnant. Now my friend, who didn’t have a baby, has two children,” she says. “I also referred another colleague who is having the same problem, and she is going to go on Sunday.”

| 16 May 2025
“I was very happy when my daughter was born”
After three years of marriage, Cambodian garment worker Sineang had started to wonder why she hadn’t yet become pregnant. Still in her early 20s, she and her husband wanted to have a baby and were not using contraception. In late 2011 or early 2012, Sineang visited a Reproductive Health Association of Cambodia clinic to seek treatment after she noticed some vaginal discharge. During the appointment, her doctor asked her more details about her sexual and reproductive health history: the issue of infertility soon came up. “I had been wanting to have a child for three years, since I was married,” she says. “I felt down about myself, but my husband gave me encouragement and told me it was okay that I was not pregnant yet.” During the initial examination, Sineang says, she was tested for cervical cancer as well as other reproductive health issues that can interfere with pregnancy. RHAC staff prescribed medication to treat her fertility problems, which she continued taking until they confirmed she was pregnant. “At first, I wasn’t really convinced that there was any relation between the discharge and not having a baby, but later I started to think that there was a connection,” she says. Throughout the whole period, Sineang went to RHAC each month – switching from infertility treatment to prenatal care – until she gave birth to a baby girl in 2013. “I was very happy when my daughter was born,” she says. “She’s healthy.” At the time, RHAC offered a discount to garment workers, which Sineang says was a big help. It’s no longer on offer, but she is an enthusiastic supporter of a plan RHAC is hoping to implement soon – a partnership with the National Social Security Fund that would allow them to visit RHAC clinics for free through the fund. “It would be really great if they could, because having a baby is expensive,” she says. “The clinic at RHAC has better service than the public hospitals. When I had my first baby, I wanted to have good service, because I had this problem with discharge [in the past].” Sineang, who is originally from Kandal province and works at Dewhirst garment factory in Phnom Penh, said she was pleased to see RHAC midwives doing regular outreach sessions at the factory. “It’s good for women to know more about these issues,” she says. And not only that, but Sineang is also an active ambassador for RHAC, spreading the word about the NGO’s services to friends and colleagues who have also struggled to have a baby. “I referred a friend to RHAC after she saw that I finally got pregnant. Now my friend, who didn’t have a baby, has two children,” she says. “I also referred another colleague who is having the same problem, and she is going to go on Sunday.”

| 18 June 2020
In pictures: Healthcare in the face of the climate crisis in Kiribati
Humanitarian crises Largely brought on by sudden onset and slow-onset natural disasters, humanitarian crises are increasingly prevalent in the Pacific. During responses to humanitarian crises in the Pacific, sexual and reproductive healthcare is often under-prioritised and under-resourced. As a result, women and girls of reproductive age and vulnerable and marginalized groups are disproportionately affected and facing increased health and psychosocial risks. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Fragile environments Low topography, rising sea levels and insufficient fresh water supply leaves Kiribati’s population vulnerable to the effects of the climate crisis. The fragility of the outer islands of Kiribati during natural disasters is compounded by their geographic isolation, which makes transportation and communication during post-disaster relief and response both expensive and difficult. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Coastal exposure The majority of the population of 115,000 people live a subsistence lifestyle. Communities are geographically dispersed across 33 atolls covering 3.5 million square kilometres in the central Pacific Ocean. The population and infrastructure within Kiribati are largely concentrated on the coast, where communities face increased exposure to climate threats and natural hazards such as tsunamis, earthquakes, king tides, flooding, droughts, and occasionally cyclones. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Takaria, leader and youth organizer in the Tebikenikua community Takaria will be running to be a Member of Parliament in Kiribati in 2020. “I assist the youth with family problems and family planning and disasters. In our community there are unforeseen pregnancies, domestic violence, and disasters such as high tide waters and strong winds, which can also affect this community. The Kiribati Family Health Association (KFHA) is the key point for us with outreach and training so people in this community know how to prevent and treat STIs, etc. They all know where the KFHA clinic is and that they can get counselling or services there. The problem now is you can’t survive with the sea rise levels. I want all members of my community to live better and have better health and peace.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Susan*, sex worker Susan receives care at the Kiribati Family Health Association (KFHA) including a pap smear. Susan*, 28, is a sex worker from the town of Betio on the main island of Kiribati. Originally from an outlying island, she moved into Tarawa to seek work. Unable to find employment that would fulfill her dream of sending money back to her two children, she was introduced to sex work. With other sex workers, she regularly travels out to the large cargo ships from China, Philippines and Korea anchored off the coast of Kiribati. Despite her new income, she still can’t speak with her children or see them due to the restrictive costs involved of travel between islands.*pseudonym Share on Twitter Share on Facebook Share via WhatsApp Share via Email Theta, 25-year-old mother and youth volunteer Theta is part of the Humanitarian Youth Club set up by the Kiribati Family Health Association in her village. “We face a lot of situations here, one of them is disasters and the second is unemployment and school drop out with our youth. I have helped the Humanitarian Youth Club to apply for financial grants from the Australian High Commission [for $1,000] I am recognized as the smartest member who can write in English. We have learned how to design a disaster plan for the community and share our ideas on sexual and reproductive issues such as STIs. We discuss what we can do for the next strong tide, where we can gather as a community and what we can do if even the maneabe (town hall) floods? If the tide and wind is too strong, we need to go to another safer place, such as another community’s town hall. For now, I want to enjoy the chance to be in our own beloved country. I won’t move until the majority have already left. I want my daughter to grow up in the same place I grew up in.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Beitau, youth volunteer Beitau is the Chairperson of the Humanitarian Youth Club. “I was lucky to be selected as Chairperson as the Humanitarian Youth Club. I feel like I get more respect from the community now I am in this position. I would love advanced training on leadership now, to further assist the club. As I am the Chairperson of the HYC, my main target is to help people during a disaster. I have attended training through KFHA. What I took from this is that when a disaster strikes, we have to do our best for pregnant women, small children and people with disabilities. They more vulnerable and less able to survive a disaster.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Abe, youth officer Abe was involved with KFHA since 2012. “I was inspired by what they KFHA was doing and the issues they were addressing that affects youth. I was surprised to see how many young people come to the clinic as they are affected by STIs, HIV and teenage pregnancy. The lack of education here is a big problem, most people here have a lot of children and yet can’t afford to send them to school. Sexual and reproductive health is our responsibility and we must talk about it with young people. Climate change affects many countries, but Kiribati is small and low lying. I used to go visit a very nice beach with a lot of nice trees and plants. Now, the trees are gone, and the waves have taken over, and the houses have disappeared so no one can build there. In my role as a youth worker and activist, I tell people to fight climate change: to grow more mangroves, to clean up the beach, because we love our Kiribati.”©IPPF/Hannah Maule-Ffinch/Kiribati Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 17 May 2025
In pictures: Healthcare in the face of the climate crisis in Kiribati
Humanitarian crises Largely brought on by sudden onset and slow-onset natural disasters, humanitarian crises are increasingly prevalent in the Pacific. During responses to humanitarian crises in the Pacific, sexual and reproductive healthcare is often under-prioritised and under-resourced. As a result, women and girls of reproductive age and vulnerable and marginalized groups are disproportionately affected and facing increased health and psychosocial risks. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Fragile environments Low topography, rising sea levels and insufficient fresh water supply leaves Kiribati’s population vulnerable to the effects of the climate crisis. The fragility of the outer islands of Kiribati during natural disasters is compounded by their geographic isolation, which makes transportation and communication during post-disaster relief and response both expensive and difficult. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Coastal exposure The majority of the population of 115,000 people live a subsistence lifestyle. Communities are geographically dispersed across 33 atolls covering 3.5 million square kilometres in the central Pacific Ocean. The population and infrastructure within Kiribati are largely concentrated on the coast, where communities face increased exposure to climate threats and natural hazards such as tsunamis, earthquakes, king tides, flooding, droughts, and occasionally cyclones. Share on Twitter Share on Facebook Share via WhatsApp Share via Email Takaria, leader and youth organizer in the Tebikenikua community Takaria will be running to be a Member of Parliament in Kiribati in 2020. “I assist the youth with family problems and family planning and disasters. In our community there are unforeseen pregnancies, domestic violence, and disasters such as high tide waters and strong winds, which can also affect this community. The Kiribati Family Health Association (KFHA) is the key point for us with outreach and training so people in this community know how to prevent and treat STIs, etc. They all know where the KFHA clinic is and that they can get counselling or services there. The problem now is you can’t survive with the sea rise levels. I want all members of my community to live better and have better health and peace.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Susan*, sex worker Susan receives care at the Kiribati Family Health Association (KFHA) including a pap smear. Susan*, 28, is a sex worker from the town of Betio on the main island of Kiribati. Originally from an outlying island, she moved into Tarawa to seek work. Unable to find employment that would fulfill her dream of sending money back to her two children, she was introduced to sex work. With other sex workers, she regularly travels out to the large cargo ships from China, Philippines and Korea anchored off the coast of Kiribati. Despite her new income, she still can’t speak with her children or see them due to the restrictive costs involved of travel between islands.*pseudonym Share on Twitter Share on Facebook Share via WhatsApp Share via Email Theta, 25-year-old mother and youth volunteer Theta is part of the Humanitarian Youth Club set up by the Kiribati Family Health Association in her village. “We face a lot of situations here, one of them is disasters and the second is unemployment and school drop out with our youth. I have helped the Humanitarian Youth Club to apply for financial grants from the Australian High Commission [for $1,000] I am recognized as the smartest member who can write in English. We have learned how to design a disaster plan for the community and share our ideas on sexual and reproductive issues such as STIs. We discuss what we can do for the next strong tide, where we can gather as a community and what we can do if even the maneabe (town hall) floods? If the tide and wind is too strong, we need to go to another safer place, such as another community’s town hall. For now, I want to enjoy the chance to be in our own beloved country. I won’t move until the majority have already left. I want my daughter to grow up in the same place I grew up in.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Beitau, youth volunteer Beitau is the Chairperson of the Humanitarian Youth Club. “I was lucky to be selected as Chairperson as the Humanitarian Youth Club. I feel like I get more respect from the community now I am in this position. I would love advanced training on leadership now, to further assist the club. As I am the Chairperson of the HYC, my main target is to help people during a disaster. I have attended training through KFHA. What I took from this is that when a disaster strikes, we have to do our best for pregnant women, small children and people with disabilities. They more vulnerable and less able to survive a disaster.” Share on Twitter Share on Facebook Share via WhatsApp Share via Email Abe, youth officer Abe was involved with KFHA since 2012. “I was inspired by what they KFHA was doing and the issues they were addressing that affects youth. I was surprised to see how many young people come to the clinic as they are affected by STIs, HIV and teenage pregnancy. The lack of education here is a big problem, most people here have a lot of children and yet can’t afford to send them to school. Sexual and reproductive health is our responsibility and we must talk about it with young people. Climate change affects many countries, but Kiribati is small and low lying. I used to go visit a very nice beach with a lot of nice trees and plants. Now, the trees are gone, and the waves have taken over, and the houses have disappeared so no one can build there. In my role as a youth worker and activist, I tell people to fight climate change: to grow more mangroves, to clean up the beach, because we love our Kiribati.”©IPPF/Hannah Maule-Ffinch/Kiribati Share on Twitter Share on Facebook Share via WhatsApp Share via Email

| 17 November 2017
“The doctors have also been giving me advice on how to look after myself and the baby"
When garment worker Ny thought she might be pregnant with her first child, a home test kit quickly confirmed her suspicions. But the 23-year-old – who is originally from Takeo province but moved to Phnom Penh to take up a job in the garment industry – did not know where to go to seek prenatal care. After a cousin recommended that she visit a nearby Reproductive Health Association of Cambodia clinic, Ny took her relative’s advice – and has gone back eight times to date. “I come here every month to check on the baby,” she says, cradling her belly. “I had never been before I got pregnant.” During her visits to the medical clinic, Ny says, she has had a raft of standard tests and procedures as part of her prenatal care, including two ultrasounds, blood and urine tests, and vaccinations. “The doctors have also been giving me advice on how to look after myself and the baby [such as] to eat nutritious food and not to carry heavy things,” she says. As well as caring for the health of mother and unborn child, RHAC staff have also offered up valuable family planning information. “I did not know about how to plan to have children before I came to the clinic,” Ny says. “The doctors here told me that there are three different methods of [long-term] contraception: medication, an implant and an IUD.” Ny, who sews winter clothing at a factory while her husband also works in a nearby garment factory, says she was very glad to learn about her options. “This child was unplanned, but I don’t feel any regret because I had already been married for two years. But after having the baby I plan to use birth control, though I don’t know what method I will use,” she says. “I know that I don’t want to have another child straight away. It may be two or three years until I have the next one, as I want to wait until my family’s finances improve.”

| 16 May 2025
“The doctors have also been giving me advice on how to look after myself and the baby"
When garment worker Ny thought she might be pregnant with her first child, a home test kit quickly confirmed her suspicions. But the 23-year-old – who is originally from Takeo province but moved to Phnom Penh to take up a job in the garment industry – did not know where to go to seek prenatal care. After a cousin recommended that she visit a nearby Reproductive Health Association of Cambodia clinic, Ny took her relative’s advice – and has gone back eight times to date. “I come here every month to check on the baby,” she says, cradling her belly. “I had never been before I got pregnant.” During her visits to the medical clinic, Ny says, she has had a raft of standard tests and procedures as part of her prenatal care, including two ultrasounds, blood and urine tests, and vaccinations. “The doctors have also been giving me advice on how to look after myself and the baby [such as] to eat nutritious food and not to carry heavy things,” she says. As well as caring for the health of mother and unborn child, RHAC staff have also offered up valuable family planning information. “I did not know about how to plan to have children before I came to the clinic,” Ny says. “The doctors here told me that there are three different methods of [long-term] contraception: medication, an implant and an IUD.” Ny, who sews winter clothing at a factory while her husband also works in a nearby garment factory, says she was very glad to learn about her options. “This child was unplanned, but I don’t feel any regret because I had already been married for two years. But after having the baby I plan to use birth control, though I don’t know what method I will use,” she says. “I know that I don’t want to have another child straight away. It may be two or three years until I have the next one, as I want to wait until my family’s finances improve.”

| 16 November 2017
“When they don’t dare to ask questions about sensitive health topics, they don’t have the information they need"
Female workers, many of them undereducated migrants from rural areas, dominate the garment sector in Cambodia. And Propitious garment factory in Takhmao, a small city that lies just south of the capital Phnom Penh, is no exception. Women make up more than 90 percent of the factory’s workforce. Helping to oversee the 3,700-strong workforce is human resources manager Kouch Davy, who has worked at Propitious since it opened four years ago. Seeing a need to improve the workers’ sexual and reproductive health knowledge, she says she decided to work with the Reproductive Health Association of Cambodia (RHAC) because of its reputation for providing high-quality services. “I raised it in a management meeting, and the board was happy to explore it,” she says. For almost two years, trained staff from RHAC have been visiting the factory twice a month to meet with workers during their lunch break. They answer questions on topics ranging from birth control to STIs and abortion. The organisation has also provided training to the nurses who work in the factory’s on-site medical clinic. Davy says the factory’s female garment workers have changed as a result. “They are more open to asking questions about sexual health and they have also become more informed about the subject,” she says. “When they don’t dare to ask questions about sensitive health topics, they don’t have the information they need, so they tend to exaggerate their problems and ask for sick leave. But when they go to see an RHAC clinic and get proper treatment, there is less sick leave. “Now that they understand about contraception, there are fewer women getting pregnant and taking maternity leave, so that also helps with the workflow. ” Davy says the factory has seen requests for sick leave drop by an average of between 100 to 200 cases a month – and any decrease in absenteeism is a major boon for productivity. “The factory works like a chain: if just one person on the production line takes a day off, it affects the overall productivity,” she says. “And if a worker comes to work sick, they have problems concentrating.” Even Davy says she has gone to RHAC to seek medical care, visiting one of their clinics a few months ago for a breast examination. Meanwhile, the company that owns Propitious has extended its partnership with RHAC to a second factory in Phnom Penh. The firm has even requested that the NGO starts visiting its largest factory, which is situated in a rural province and has 10,000 workers, in the future.

| 16 May 2025
“When they don’t dare to ask questions about sensitive health topics, they don’t have the information they need"
Female workers, many of them undereducated migrants from rural areas, dominate the garment sector in Cambodia. And Propitious garment factory in Takhmao, a small city that lies just south of the capital Phnom Penh, is no exception. Women make up more than 90 percent of the factory’s workforce. Helping to oversee the 3,700-strong workforce is human resources manager Kouch Davy, who has worked at Propitious since it opened four years ago. Seeing a need to improve the workers’ sexual and reproductive health knowledge, she says she decided to work with the Reproductive Health Association of Cambodia (RHAC) because of its reputation for providing high-quality services. “I raised it in a management meeting, and the board was happy to explore it,” she says. For almost two years, trained staff from RHAC have been visiting the factory twice a month to meet with workers during their lunch break. They answer questions on topics ranging from birth control to STIs and abortion. The organisation has also provided training to the nurses who work in the factory’s on-site medical clinic. Davy says the factory’s female garment workers have changed as a result. “They are more open to asking questions about sexual health and they have also become more informed about the subject,” she says. “When they don’t dare to ask questions about sensitive health topics, they don’t have the information they need, so they tend to exaggerate their problems and ask for sick leave. But when they go to see an RHAC clinic and get proper treatment, there is less sick leave. “Now that they understand about contraception, there are fewer women getting pregnant and taking maternity leave, so that also helps with the workflow. ” Davy says the factory has seen requests for sick leave drop by an average of between 100 to 200 cases a month – and any decrease in absenteeism is a major boon for productivity. “The factory works like a chain: if just one person on the production line takes a day off, it affects the overall productivity,” she says. “And if a worker comes to work sick, they have problems concentrating.” Even Davy says she has gone to RHAC to seek medical care, visiting one of their clinics a few months ago for a breast examination. Meanwhile, the company that owns Propitious has extended its partnership with RHAC to a second factory in Phnom Penh. The firm has even requested that the NGO starts visiting its largest factory, which is situated in a rural province and has 10,000 workers, in the future.

| 16 November 2017
"During the pregnancy I was very worried”
Sophorn, a garment worker for the past decade, first visited a Reproductive Health Association of Cambodia (RHAC) clinic when she was pregnant with her first child. She returned for health checks each month until, at five months pregnant, she lost the baby. Her second pregnancy also resulted in a miscarriage, leaving her distraught. Then, she got pregnant a third time, in 2013. “I started to discuss with the doctors how to protect my child,” she says. “They gave me medication to strengthen my cervix, which I took for six months. In the seventh month, I gave birth prematurely.” Doctors told Sophorn that her baby girl was health, but she only weighed in at 1.7 kilograms. The infant was taken to a specialist children’s hospital, where she was cared for an additional two weeks. “During the pregnancy I was very worried,” Sophorn says. “I felt so happy when I finally delivered my child.” Her daughter was born without any complications is now a happy and healthy four years old. In initial stages of her third pregnancy, Sophorn’s friends told her that she would have to undergo surgery on her cervix or have injections to help her carry her baby to term, and doctors at a private clinic confirmed their suggestions. However, she decided to seek a second opinion at RHAC, where doctors instead gave her a prescription to strengthen her cervix. “When I heard I needed to have that surgery I was very scared, so I was relieved when the doctor at RHAC told me to take the medication instead,” she says. “While I was taking the medication I observed my body and any changes to it, so when I felt unwell I would go to the doctors and consult them, so I felt comfortable to continue taking it.” Sophorn also went for appointments at a government-run hospital, but found that their services were also lacking. “I told the doctors about losing my first and second babies, but they only weighed me and measured my stomach. There weren’t any more examinations or very much care,” she says. “When I went to RHAC they did so many examinations and had so many services, so I think it’s really better to go to RHAC for these kinds of services.” She estimates that during her third pregnancy, she had ten appointments at RHAC clinics at a cost of 40,000 to 60,000 riel (£7.40 to £11.15) each time. Compared to just 2,000 riel for an obstetrics appointment at the public hospital, the difference in cost is significant. “It’s expensive for me because my salary is little.” Despite the relatively high prices, Sophorn already knows where she will go for medical care in the future. “I want to have one more child, and I have already planned that when I decide to do it I will go to RHAC to get my cervix checked first,” she says. Until that day comes, Sophorn is taking the oral contraceptive after receiving advice about birth control from RHAC’s clinicians, with a midwife from the NGO making regular visits to the factory.

| 16 May 2025
"During the pregnancy I was very worried”
Sophorn, a garment worker for the past decade, first visited a Reproductive Health Association of Cambodia (RHAC) clinic when she was pregnant with her first child. She returned for health checks each month until, at five months pregnant, she lost the baby. Her second pregnancy also resulted in a miscarriage, leaving her distraught. Then, she got pregnant a third time, in 2013. “I started to discuss with the doctors how to protect my child,” she says. “They gave me medication to strengthen my cervix, which I took for six months. In the seventh month, I gave birth prematurely.” Doctors told Sophorn that her baby girl was health, but she only weighed in at 1.7 kilograms. The infant was taken to a specialist children’s hospital, where she was cared for an additional two weeks. “During the pregnancy I was very worried,” Sophorn says. “I felt so happy when I finally delivered my child.” Her daughter was born without any complications is now a happy and healthy four years old. In initial stages of her third pregnancy, Sophorn’s friends told her that she would have to undergo surgery on her cervix or have injections to help her carry her baby to term, and doctors at a private clinic confirmed their suggestions. However, she decided to seek a second opinion at RHAC, where doctors instead gave her a prescription to strengthen her cervix. “When I heard I needed to have that surgery I was very scared, so I was relieved when the doctor at RHAC told me to take the medication instead,” she says. “While I was taking the medication I observed my body and any changes to it, so when I felt unwell I would go to the doctors and consult them, so I felt comfortable to continue taking it.” Sophorn also went for appointments at a government-run hospital, but found that their services were also lacking. “I told the doctors about losing my first and second babies, but they only weighed me and measured my stomach. There weren’t any more examinations or very much care,” she says. “When I went to RHAC they did so many examinations and had so many services, so I think it’s really better to go to RHAC for these kinds of services.” She estimates that during her third pregnancy, she had ten appointments at RHAC clinics at a cost of 40,000 to 60,000 riel (£7.40 to £11.15) each time. Compared to just 2,000 riel for an obstetrics appointment at the public hospital, the difference in cost is significant. “It’s expensive for me because my salary is little.” Despite the relatively high prices, Sophorn already knows where she will go for medical care in the future. “I want to have one more child, and I have already planned that when I decide to do it I will go to RHAC to get my cervix checked first,” she says. Until that day comes, Sophorn is taking the oral contraceptive after receiving advice about birth control from RHAC’s clinicians, with a midwife from the NGO making regular visits to the factory.

| 16 November 2017
“Just yesterday during the outreach service, a woman asked me why she didn’t get her period after having an abortion..."
Pann Chandy gave her first sexual education lesson when she was still at school as a volunteer youth social worker with the Reproductive Health Association of Cambodia (RHAC). She had no qualms about standing up in front of her classmates to discuss culturally taboo topics when she was just a teenager. Now aged 25 and in possession of a Bachelor degree in midwifery, Chandy has been employed by RHAC for less than a year, working as part of the organisation’s health outreach team. The job is demanding: she is tasked with regularly visiting four karaoke parlours, eight garment factories and 20 villages in Phnom Penh, with plans to expand to two universities imminently. Travelling for hours A round trip to some communities can take two hours or more on her motorcycle, travelling alone into areas that are not always easily accessible. “Sometimes I have the clinic staff with me, but rarely,” Chandy says. “I promote the health services provided by Reproductive Health Association of Cambodia as well. If they are interested in going to a clinic, I give them a referral,” she says. One of the factories on her regular roster is Propitious garment factory in Takhmao, a small city south of Phnom Penh. Chandy spends two days a month at the factory, where she speaks to groups of women or has one-on-one discussions about sensitive topics. Passionate about the job “Just yesterday during the outreach service, a woman asked me why she didn’t get her period after having an abortion. She wanted to know what was wrong,” she says. “It’s common for women to use unsafe abortion methods. Mainly they take medicine from a pharmacy, and the pharmacy doesn’t give them any advice on how to use it. Often they go to cheap, unlicensed clinics near the factories for medical abortions.” Chandy is passionate about her job at Reproductive Health Association of Cambodia, and dreams about one day setting up her own pharmacy where she could provide comprehensive advice to clients. “There are a lot of unlicensed pharmacists in this country,” she says, many of which prescribe the counterfeit medicines that have inundated the market. “I think I may have the capacity to become a licensed one."

| 16 May 2025
“Just yesterday during the outreach service, a woman asked me why she didn’t get her period after having an abortion..."
Pann Chandy gave her first sexual education lesson when she was still at school as a volunteer youth social worker with the Reproductive Health Association of Cambodia (RHAC). She had no qualms about standing up in front of her classmates to discuss culturally taboo topics when she was just a teenager. Now aged 25 and in possession of a Bachelor degree in midwifery, Chandy has been employed by RHAC for less than a year, working as part of the organisation’s health outreach team. The job is demanding: she is tasked with regularly visiting four karaoke parlours, eight garment factories and 20 villages in Phnom Penh, with plans to expand to two universities imminently. Travelling for hours A round trip to some communities can take two hours or more on her motorcycle, travelling alone into areas that are not always easily accessible. “Sometimes I have the clinic staff with me, but rarely,” Chandy says. “I promote the health services provided by Reproductive Health Association of Cambodia as well. If they are interested in going to a clinic, I give them a referral,” she says. One of the factories on her regular roster is Propitious garment factory in Takhmao, a small city south of Phnom Penh. Chandy spends two days a month at the factory, where she speaks to groups of women or has one-on-one discussions about sensitive topics. Passionate about the job “Just yesterday during the outreach service, a woman asked me why she didn’t get her period after having an abortion. She wanted to know what was wrong,” she says. “It’s common for women to use unsafe abortion methods. Mainly they take medicine from a pharmacy, and the pharmacy doesn’t give them any advice on how to use it. Often they go to cheap, unlicensed clinics near the factories for medical abortions.” Chandy is passionate about her job at Reproductive Health Association of Cambodia, and dreams about one day setting up her own pharmacy where she could provide comprehensive advice to clients. “There are a lot of unlicensed pharmacists in this country,” she says, many of which prescribe the counterfeit medicines that have inundated the market. “I think I may have the capacity to become a licensed one."

| 16 November 2017
“I was very happy when my daughter was born”
After three years of marriage, Cambodian garment worker Sineang had started to wonder why she hadn’t yet become pregnant. Still in her early 20s, she and her husband wanted to have a baby and were not using contraception. In late 2011 or early 2012, Sineang visited a Reproductive Health Association of Cambodia clinic to seek treatment after she noticed some vaginal discharge. During the appointment, her doctor asked her more details about her sexual and reproductive health history: the issue of infertility soon came up. “I had been wanting to have a child for three years, since I was married,” she says. “I felt down about myself, but my husband gave me encouragement and told me it was okay that I was not pregnant yet.” During the initial examination, Sineang says, she was tested for cervical cancer as well as other reproductive health issues that can interfere with pregnancy. RHAC staff prescribed medication to treat her fertility problems, which she continued taking until they confirmed she was pregnant. “At first, I wasn’t really convinced that there was any relation between the discharge and not having a baby, but later I started to think that there was a connection,” she says. Throughout the whole period, Sineang went to RHAC each month – switching from infertility treatment to prenatal care – until she gave birth to a baby girl in 2013. “I was very happy when my daughter was born,” she says. “She’s healthy.” At the time, RHAC offered a discount to garment workers, which Sineang says was a big help. It’s no longer on offer, but she is an enthusiastic supporter of a plan RHAC is hoping to implement soon – a partnership with the National Social Security Fund that would allow them to visit RHAC clinics for free through the fund. “It would be really great if they could, because having a baby is expensive,” she says. “The clinic at RHAC has better service than the public hospitals. When I had my first baby, I wanted to have good service, because I had this problem with discharge [in the past].” Sineang, who is originally from Kandal province and works at Dewhirst garment factory in Phnom Penh, said she was pleased to see RHAC midwives doing regular outreach sessions at the factory. “It’s good for women to know more about these issues,” she says. And not only that, but Sineang is also an active ambassador for RHAC, spreading the word about the NGO’s services to friends and colleagues who have also struggled to have a baby. “I referred a friend to RHAC after she saw that I finally got pregnant. Now my friend, who didn’t have a baby, has two children,” she says. “I also referred another colleague who is having the same problem, and she is going to go on Sunday.”

| 16 May 2025
“I was very happy when my daughter was born”
After three years of marriage, Cambodian garment worker Sineang had started to wonder why she hadn’t yet become pregnant. Still in her early 20s, she and her husband wanted to have a baby and were not using contraception. In late 2011 or early 2012, Sineang visited a Reproductive Health Association of Cambodia clinic to seek treatment after she noticed some vaginal discharge. During the appointment, her doctor asked her more details about her sexual and reproductive health history: the issue of infertility soon came up. “I had been wanting to have a child for three years, since I was married,” she says. “I felt down about myself, but my husband gave me encouragement and told me it was okay that I was not pregnant yet.” During the initial examination, Sineang says, she was tested for cervical cancer as well as other reproductive health issues that can interfere with pregnancy. RHAC staff prescribed medication to treat her fertility problems, which she continued taking until they confirmed she was pregnant. “At first, I wasn’t really convinced that there was any relation between the discharge and not having a baby, but later I started to think that there was a connection,” she says. Throughout the whole period, Sineang went to RHAC each month – switching from infertility treatment to prenatal care – until she gave birth to a baby girl in 2013. “I was very happy when my daughter was born,” she says. “She’s healthy.” At the time, RHAC offered a discount to garment workers, which Sineang says was a big help. It’s no longer on offer, but she is an enthusiastic supporter of a plan RHAC is hoping to implement soon – a partnership with the National Social Security Fund that would allow them to visit RHAC clinics for free through the fund. “It would be really great if they could, because having a baby is expensive,” she says. “The clinic at RHAC has better service than the public hospitals. When I had my first baby, I wanted to have good service, because I had this problem with discharge [in the past].” Sineang, who is originally from Kandal province and works at Dewhirst garment factory in Phnom Penh, said she was pleased to see RHAC midwives doing regular outreach sessions at the factory. “It’s good for women to know more about these issues,” she says. And not only that, but Sineang is also an active ambassador for RHAC, spreading the word about the NGO’s services to friends and colleagues who have also struggled to have a baby. “I referred a friend to RHAC after she saw that I finally got pregnant. Now my friend, who didn’t have a baby, has two children,” she says. “I also referred another colleague who is having the same problem, and she is going to go on Sunday.”