Spotlight
A selection of stories from across the Federation

Advances in Sexual and Reproductive Rights and Health: 2024 in Review
Let’s take a leap back in time to the beginning of 2024: In twelve months, what victories has our movement managed to secure in the face of growing opposition and the rise of the far right? These victories for sexual and reproductive rights and health are the result of relentless grassroots work and advocacy by our Member Associations, in partnership with community organizations, allied politicians, and the mobilization of public opinion.
Most Popular This Week

Advances in Sexual and Reproductive Rights and Health: 2024 in Review
Let’s take a leap back in time to the beginning of 2024: In twelve months, what victories has our movement managed to secure in t
Kazakhstan

Kazakhstan's Rising HIV Crisis: A Call for Action
On World AIDS Day, we commemorate the remarkable achievements of IPPF Member Associations in their unwavering commitment to combating the HIV epidemic.

Ensuring SRHR in Humanitarian Crises: What You Need to Know
Over the past two decades, global forced displacement has consistently increased, affecting an estimated 114 million people as of mid-2023.
Estonia, Nepal, Namibia, Japan, Thailand

The Rainbow Wave for Marriage Equality
Love wins! The fight for marriage equality has seen incredible progress worldwide, with a recent surge in legalizations.
France, Germany, Poland, United Kingdom, United States, Colombia, India, Tunisia

Abortion Rights: Latest Decisions and Developments around the World
Over the past 30 years, more than

Palestine

In their own words: The people providing sexual and reproductive health care under bombardment in Gaza
Week after week, heavy Israeli bombardment from air, land, and sea, has continued across most of the Gaza Strip.
Vanuatu

When getting to the hospital is difficult, Vanuatu mobile outreach can save lives
In the mountains of Kumera on Tanna Island, Vanuatu, the village women of Kamahaul normally spend over 10,000 Vatu ($83 USD) to travel to the nearest hospital.
Filter our stories by:
- Afghan Family Guidance Association
- Albanian Center for Population and Development
- Asociación Pro-Bienestar de la Familia Colombiana
- Associação Moçambicana para Desenvolvimento da Família
- Association Béninoise pour la Promotion de la Famille
- Association Burundaise pour le Bien-Etre Familial
- Association Malienne pour la Protection et la Promotion de la Famille
- Association pour le Bien-Etre Familial/Naissances Désirables
- Association Sénégalaise pour le Bien-Étre Familial
- Association Togolaise pour le Bien-Etre Familial
- Association Tunisienne de la Santé de la Reproduction
- Botswana Family Welfare Association
- Cameroon National Association for Family Welfare
- Cook Islands Family Welfare Association
- Eesti Seksuaaltervise Liit / Estonian Sexual Health Association
- Family Guidance Association of Ethiopia
- Family Planning Association of India
- Family Planning Association of Malawi
- Family Planning Association of Nepal
- Family Planning Association of Sri Lanka
- Family Planning Association of Trinidad and Tobago
- Foundation for the Promotion of Responsible Parenthood - Aruba
- Indonesian Planned Parenthood Association
- Jamaica Family Planning Association
- Kazakhstan Association on Sexual and Reproductive Health (KMPA)
- Kiribati Family Health Association
- Lesotho Planned Parenthood Association
- Mouvement Français pour le Planning Familial
- (-) Palestinian Family Planning and Protection Association (PFPPA)
- Planned Parenthood Association of Ghana
- Planned Parenthood Association of Thailand
- Planned Parenthood Association of Zambia
- Planned Parenthood Federation of America
- Planned Parenthood Federation of Nigeria
- Pro Familia - Germany
- Rahnuma-Family Planning Association of Pakistan
- Reproductive & Family Health Association of Fiji
- Reproductive Health Association of Cambodia (RHAC)
- (-) Reproductive Health Uganda
- Somaliland Family Health Association
- Sudan Family Planning Association
- Tonga Family Health Association
- Vanuatu Family Health Association


| 29 December 2023
In their own words: The people providing sexual and reproductive health care under bombardment in Gaza
Week after week, heavy Israeli bombardment from air, land, and sea, has continued across most of the Gaza Strip. According to the Ministry of Health, at least 21,320 Palestinians have been killed in Gaza since October 7th, about 70% of whom are women and children. Nearly 2 million people have been displaced from their homes, forced to live in extremely overcrowded and unsanitary shelters. The Ministry of Health says that 50% of pregnant women in the shelters suffer from thirst and malnutrition, and there is a lack of health care and vaccinations for newborns. The suffering is unimaginable, yet it is all too real. Many of those bearing witness to the seemingly endless death and misery are frontline healthcare workers - including those delivering sexual and reproductive healthcare. But they, too, are at risk of being killed just for doing their jobs. Israel continues to bombard Gaza’s health facilities and residential areas, despite mounting international pressure for a ceasefire - something IPPF and many other humanitarian organisations have been demanding for months. According to the World Health Organization (WHO) there have been more than 200 Israeli attacks on hospitals and ambulances since Oct. 7, with many medical workers detained during Israeli raids. At least 300 healthcare workers have been reported killed, according to the UN. This is more than the total number of health worker deaths recorded across all countries in conflict last year, and in any single year since 2016. Staff at IPPF's local member association, the Palestinian Family Planning and Protection Association (PFPPA), are among the heroic healthcare workers in Gaza that continue to provide care as best they can in the ongoing humanitarian catastrophe. We fear for their safety - and that of the 2.3 million civilians in Gaza - every single day. In their own words, PFPPA and other health workers describe what it's like to provide care under bombardment and blockade in Gaza and in the West Bank - offering glimpses of terror, devastation, and even some hope.

| 29 December 2023
In their own words: The people providing sexual and reproductive health care under bombardment in Gaza
Week after week, heavy Israeli bombardment from air, land, and sea, has continued across most of the Gaza Strip. According to the Ministry of Health, at least 21,320 Palestinians have been killed in Gaza since October 7th, about 70% of whom are women and children. Nearly 2 million people have been displaced from their homes, forced to live in extremely overcrowded and unsanitary shelters. The Ministry of Health says that 50% of pregnant women in the shelters suffer from thirst and malnutrition, and there is a lack of health care and vaccinations for newborns. The suffering is unimaginable, yet it is all too real. Many of those bearing witness to the seemingly endless death and misery are frontline healthcare workers - including those delivering sexual and reproductive healthcare. But they, too, are at risk of being killed just for doing their jobs. Israel continues to bombard Gaza’s health facilities and residential areas, despite mounting international pressure for a ceasefire - something IPPF and many other humanitarian organisations have been demanding for months. According to the World Health Organization (WHO) there have been more than 200 Israeli attacks on hospitals and ambulances since Oct. 7, with many medical workers detained during Israeli raids. At least 300 healthcare workers have been reported killed, according to the UN. This is more than the total number of health worker deaths recorded across all countries in conflict last year, and in any single year since 2016. Staff at IPPF's local member association, the Palestinian Family Planning and Protection Association (PFPPA), are among the heroic healthcare workers in Gaza that continue to provide care as best they can in the ongoing humanitarian catastrophe. We fear for their safety - and that of the 2.3 million civilians in Gaza - every single day. In their own words, PFPPA and other health workers describe what it's like to provide care under bombardment and blockade in Gaza and in the West Bank - offering glimpses of terror, devastation, and even some hope.

| 04 April 2019
"Women in our communities use many unsafe methods to try to end pregnancies"
Women and girls in Palestine face a number of difficulties and challenges. The ongoing conflict and lack of sitting government as well as high unemployment, has led to poverty and inequality, while an increasingly conservative society and traditionally patriarchal culture has led to increased gender-inequality and lack of access to sexual and reproductive healthcare. The current abortion law unfairly pushes women to risk their lives and health to attempt to end their unwanted pregnancies in unsafe ways. In this context, the Palestinian Family Planning and Protection Agency (PFPPA) has been working since 1964, to provide sexual and reproductive healthcare and advocate for women’s rights. Having received two grants from Safe Abortion Action Fund (SAAF) since 2014, they have been working on the lack of access to safe abortion in the country with a focus on increasing their provision of abortion-related services and advocating at community and national level for changes to the abortion law. My name is Fatima, I am a midwife and have worked with PFPPA for 18 years in the Halhul clinic in Palestine. PFPPA has had a great impact on me personally as well as the community as a whole. I experienced violence in my marriage but when I joined the organization I learned the meaning of violence and I realized that I didn’t have to put up with it and could make decisions for myself. This was a turning point in my life. My life changed 180 degrees, thank God, and my husband stopped being violent. Society & acceptance Since I have worked here, I have seen changes in society’s acceptance of sexual and reproductive health issues and I feel that more people are supporting us. They can be women, religious personalities or young volunteers. One of the proudest moments of my work has been working with a young man who was training to be a peer educator, he was violent, especially with his sister. From the very start of the training, he was against the issues that we were presenting, however, he started to understand our issues. I also met his mother and she thanked me for the change that happened in his life. She came to say that he is now helping in the house - washing dishes and doing other tasks that he would have thought were just for women before. The challenges that we face are a misunderstanding of religion, negative traditions and customs, as well as the political situation in Palestine with the occupation, the walls, the checkpoints as well as the economic situation. We work on issues that will take many years to witness any change due to the negative traditions and customs. Harm reduction & abortion care We have recently started implementing a harm reduction approach to abortion care. I remember one woman who was 44 years old and divorced. She came to the clinic and was seven weeks pregnant. Her face was pale and tired...I felt that all the problems were on her shoulders. She was looking for a saviour. We supported her with harm reduction information and afterwards provided information on post-abortion contraception. After one or two months she sent a message thanking me, saying that we had saved her life, I was really happy about that. There are also cases of women that come here, maybe they took pills or they did something that made them bleed. They don’t tell you what they did but I can detect if I think an abortion happened. If it is an incomplete abortion, we explain how to take the treatment and we follow up with support. Unsafe methods Women in our communities use many unsafe methods to try to end pregnancies. They drink special teas or chlorine. They jump off things or ask their children to jump on them. They sometimes put suppositories made from Arabic medicinal herbs into the cervix. Although it is common, deaths are not registered as linked to unsafe abortion but are probably registered as maternal deaths. When the society says that abortion is haram (forbidden), they don’t take into consideration the issues and these women in need. Imagine if we had safe abortion services at the hospitals, we would not see these issues at all. There are women who would choose abortion for reasons like their age, their health, social issues and psychological issues. There are women themselves who say “I will die if I complete this pregnancy”. I am passionate about the work that I do. I advocate for these issues everywhere I go, on the bus, during weddings and with friends and family, wherever I go. That is why the Safe Abortion Action Fund (SAAF) funded project is so important. I have learned a lot about advocacy and campaigning, how we manage legal advocacy and how to work with decision-makers. We have run events to mark International Safe Abortion Day with groups of women gathered here in the centre and with decision-makers and volunteers. Read more stories from SAAF in Palestine

| 15 May 2025
"Women in our communities use many unsafe methods to try to end pregnancies"
Women and girls in Palestine face a number of difficulties and challenges. The ongoing conflict and lack of sitting government as well as high unemployment, has led to poverty and inequality, while an increasingly conservative society and traditionally patriarchal culture has led to increased gender-inequality and lack of access to sexual and reproductive healthcare. The current abortion law unfairly pushes women to risk their lives and health to attempt to end their unwanted pregnancies in unsafe ways. In this context, the Palestinian Family Planning and Protection Agency (PFPPA) has been working since 1964, to provide sexual and reproductive healthcare and advocate for women’s rights. Having received two grants from Safe Abortion Action Fund (SAAF) since 2014, they have been working on the lack of access to safe abortion in the country with a focus on increasing their provision of abortion-related services and advocating at community and national level for changes to the abortion law. My name is Fatima, I am a midwife and have worked with PFPPA for 18 years in the Halhul clinic in Palestine. PFPPA has had a great impact on me personally as well as the community as a whole. I experienced violence in my marriage but when I joined the organization I learned the meaning of violence and I realized that I didn’t have to put up with it and could make decisions for myself. This was a turning point in my life. My life changed 180 degrees, thank God, and my husband stopped being violent. Society & acceptance Since I have worked here, I have seen changes in society’s acceptance of sexual and reproductive health issues and I feel that more people are supporting us. They can be women, religious personalities or young volunteers. One of the proudest moments of my work has been working with a young man who was training to be a peer educator, he was violent, especially with his sister. From the very start of the training, he was against the issues that we were presenting, however, he started to understand our issues. I also met his mother and she thanked me for the change that happened in his life. She came to say that he is now helping in the house - washing dishes and doing other tasks that he would have thought were just for women before. The challenges that we face are a misunderstanding of religion, negative traditions and customs, as well as the political situation in Palestine with the occupation, the walls, the checkpoints as well as the economic situation. We work on issues that will take many years to witness any change due to the negative traditions and customs. Harm reduction & abortion care We have recently started implementing a harm reduction approach to abortion care. I remember one woman who was 44 years old and divorced. She came to the clinic and was seven weeks pregnant. Her face was pale and tired...I felt that all the problems were on her shoulders. She was looking for a saviour. We supported her with harm reduction information and afterwards provided information on post-abortion contraception. After one or two months she sent a message thanking me, saying that we had saved her life, I was really happy about that. There are also cases of women that come here, maybe they took pills or they did something that made them bleed. They don’t tell you what they did but I can detect if I think an abortion happened. If it is an incomplete abortion, we explain how to take the treatment and we follow up with support. Unsafe methods Women in our communities use many unsafe methods to try to end pregnancies. They drink special teas or chlorine. They jump off things or ask their children to jump on them. They sometimes put suppositories made from Arabic medicinal herbs into the cervix. Although it is common, deaths are not registered as linked to unsafe abortion but are probably registered as maternal deaths. When the society says that abortion is haram (forbidden), they don’t take into consideration the issues and these women in need. Imagine if we had safe abortion services at the hospitals, we would not see these issues at all. There are women who would choose abortion for reasons like their age, their health, social issues and psychological issues. There are women themselves who say “I will die if I complete this pregnancy”. I am passionate about the work that I do. I advocate for these issues everywhere I go, on the bus, during weddings and with friends and family, wherever I go. That is why the Safe Abortion Action Fund (SAAF) funded project is so important. I have learned a lot about advocacy and campaigning, how we manage legal advocacy and how to work with decision-makers. We have run events to mark International Safe Abortion Day with groups of women gathered here in the centre and with decision-makers and volunteers. Read more stories from SAAF in Palestine

| 03 April 2019
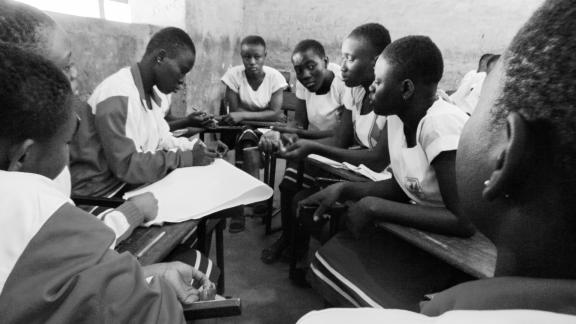
"The students don’t normally ask about abortion as it is such a taboo"
Women and girls in Palestine face a number of difficulties and challenges. The ongoing conflict and lack of sitting government as well as high unemployment, has led to poverty and inequality, while an increasingly conservative society and traditionally patriarchal culture has led to increased gender-inequality and lack of access to sexual and reproductive healthcare. The current abortion law unfairly pushes women to risk their lives and health to attempt to end their unwanted pregnancies in unsafe ways. In this context, the Palestinian Family Planning and Protection Agency (PFPPA) has been working since 1964, to provide sexual and reproductive healthcare and advocate for women’s rights. Having received two grants from Safe Abortion Action Fund (SAAF) since 2014, they have been working on the lack of access to safe abortion in the country with a focus on increasing their provision of abortion-related services and advocating at community and national level for changes to the abortion law. My name is Amani and I am 24 years old. I live with my parents in Bethlehem in the West Bank and I work as a midwife in a family hospital in Jerusalem as well as a peer education volunteer with the Palestinian Family Planning and Protection Agency. Working in schools Part of my role as a volunteer involves going to schools and doing presentations about early-marriage, family planning and gender-based violence. Even though sex outside of marriage is taboo, it does happen. However, it is very hard for unmarried people to access contraception as the culture is so restrictive, especially here in Hebron. When they need contraception, the man usually goes by himself or they look online. When we go to schools and talk to students about the subject of sexual health, the students want to know more because at home it is a taboo to talk about such things. We get many questions about issues such as masturbation or what causes pregnancy. They just know that it happens when men and women are together, they do not know how it happens. So people may ask a question like: ‘if I touch somebody, if I stand near someone or kiss them will I get pregnant?’ Abortion is still a taboo The students don’t normally ask about abortion as it is such a taboo. I do know that unsafe abortion happens though, for example my grandmother tried to end her pregnancy once. She was forty-five years old and had six children already. She did not know any way of not getting pregnant or safely ending the pregnancy. She told me that she drank liquids and jumped from the stairs, taking a great risk. She really didn’t want to be pregnant again and tried hard to end it but it did not work. I am very proud that as a peer educator I have expanded my knowledge on many issues, including how to provide harm reduction information to women so that they can reduce risks of unsafe abortion and not do what my grandmother did in case they don’t want to be pregnant. Once I met with a woman who already had six children, she was tired of having children but her husband wanted to have more so we visited them at home and through conversation, the husband understood the need, so she was able to access an IUD. Here we work a lot with women, we change them, we speak with them, they change their opinions, they become decision-makers and they leave the clinic as different people. Read more stories from SAAF in Palestine

| 15 May 2025
"The students don’t normally ask about abortion as it is such a taboo"
Women and girls in Palestine face a number of difficulties and challenges. The ongoing conflict and lack of sitting government as well as high unemployment, has led to poverty and inequality, while an increasingly conservative society and traditionally patriarchal culture has led to increased gender-inequality and lack of access to sexual and reproductive healthcare. The current abortion law unfairly pushes women to risk their lives and health to attempt to end their unwanted pregnancies in unsafe ways. In this context, the Palestinian Family Planning and Protection Agency (PFPPA) has been working since 1964, to provide sexual and reproductive healthcare and advocate for women’s rights. Having received two grants from Safe Abortion Action Fund (SAAF) since 2014, they have been working on the lack of access to safe abortion in the country with a focus on increasing their provision of abortion-related services and advocating at community and national level for changes to the abortion law. My name is Amani and I am 24 years old. I live with my parents in Bethlehem in the West Bank and I work as a midwife in a family hospital in Jerusalem as well as a peer education volunteer with the Palestinian Family Planning and Protection Agency. Working in schools Part of my role as a volunteer involves going to schools and doing presentations about early-marriage, family planning and gender-based violence. Even though sex outside of marriage is taboo, it does happen. However, it is very hard for unmarried people to access contraception as the culture is so restrictive, especially here in Hebron. When they need contraception, the man usually goes by himself or they look online. When we go to schools and talk to students about the subject of sexual health, the students want to know more because at home it is a taboo to talk about such things. We get many questions about issues such as masturbation or what causes pregnancy. They just know that it happens when men and women are together, they do not know how it happens. So people may ask a question like: ‘if I touch somebody, if I stand near someone or kiss them will I get pregnant?’ Abortion is still a taboo The students don’t normally ask about abortion as it is such a taboo. I do know that unsafe abortion happens though, for example my grandmother tried to end her pregnancy once. She was forty-five years old and had six children already. She did not know any way of not getting pregnant or safely ending the pregnancy. She told me that she drank liquids and jumped from the stairs, taking a great risk. She really didn’t want to be pregnant again and tried hard to end it but it did not work. I am very proud that as a peer educator I have expanded my knowledge on many issues, including how to provide harm reduction information to women so that they can reduce risks of unsafe abortion and not do what my grandmother did in case they don’t want to be pregnant. Once I met with a woman who already had six children, she was tired of having children but her husband wanted to have more so we visited them at home and through conversation, the husband understood the need, so she was able to access an IUD. Here we work a lot with women, we change them, we speak with them, they change their opinions, they become decision-makers and they leave the clinic as different people. Read more stories from SAAF in Palestine

| 02 April 2019
"From my experience the situation in relation to abortion in Palestine is very hard"
Women and girls in Palestine face a number of difficulties and challenges. The ongoing conflict and lack of sitting government as well as high unemployment, has led to poverty and inequality, while an increasingly conservative society and traditionally patriarchal culture has led to increased gender-inequality and lack of access to sexual and reproductive healthcare. The current abortion law unfairly pushes women to risk their lives and health to attempt to end their unwanted pregnancies in unsafe ways. In this context, the Palestinian Family Planning and Protection Agency (PFPPA) has been working since 1964, to provide sexual and reproductive healthcare and advocate for women’s rights. Having received two grants from Safe Abortion Action Fund (SAAF) since 2014, they have been working on the lack of access to safe abortion in the country with a focus on increasing their provision of abortion-related services and advocating at community and national level for changes to the abortion law. My name is Khawla*, I am 42 years old and I am a midwife and university lecturer. I have been married for 10 years and have three children, two boys and a girl. I have multiple health issues and a number of hereditary conditions in my family. I first became involved with PFPPA through my work, having taken many trainings with them about issues such as early marriage, gender-based violence, sexual health and safe abortion. Then last year I accidentally became pregnant myself. My youngest child was just two years old, I had a new job at the time and was suffering with a number of health issues that would make another pregnancy dangerous for me. Unintended pregnancy When I read that the pregnancy test was positive, it was a very hard time. I started crying – I felt like the world was very black – it was the end of my life. I would kill myself, if I didn’t end this pregnancy. So I came to PFPPA and they treated me as a client. I met with the social worker, midwife and doctor and, since the pregnancy was risk to my life and I was very weak and bleeding when I reached them they were able to prescribe the tablets. These pills are highly regulated and restricted here and not all pharmacists stock them but I was able to access them with the prescription and they worked. PFPPA provided follow up afterwards helping me to find an effective long-acting family planning method. Even though I knew about the different methods, they discussed them all with me to ensure that they would be appropriate for my health. Even though the law allows abortion in cases of risks to health of the woman, you need to get permission from the religious leaders and they are very hard to convince. I took my case to them and, despite my health issues, they refused despite it being very early in the pregnancy, before the ensoulment and is allowed according to Islam. The public hospital will not perform it unless they receive the permission from the religious leaders and they don’t give it despite what the religious rules say. Stigma & access From my experience the situation in relation to abortion in Palestine is very hard. There are many women who get pregnant who did not plan it and it’s not the time for the pregnancy. The door is closed to them from the public health system. I have started to campaign on this issue now, I talk to the students in my course about how we can solve this problem. I think the stigma is very difficult. I never thought I would be in this situation, I talked a lot about it before but when you are in the situation, it is totally different. I really appreciated the help given from the PFPPA team, particularly the psychological support. When I felt bad, they helped me to see that I was doing the right thing and it was my right. Read more stories from SAAF in Palestine *Not her real name

| 16 May 2025
"From my experience the situation in relation to abortion in Palestine is very hard"
Women and girls in Palestine face a number of difficulties and challenges. The ongoing conflict and lack of sitting government as well as high unemployment, has led to poverty and inequality, while an increasingly conservative society and traditionally patriarchal culture has led to increased gender-inequality and lack of access to sexual and reproductive healthcare. The current abortion law unfairly pushes women to risk their lives and health to attempt to end their unwanted pregnancies in unsafe ways. In this context, the Palestinian Family Planning and Protection Agency (PFPPA) has been working since 1964, to provide sexual and reproductive healthcare and advocate for women’s rights. Having received two grants from Safe Abortion Action Fund (SAAF) since 2014, they have been working on the lack of access to safe abortion in the country with a focus on increasing their provision of abortion-related services and advocating at community and national level for changes to the abortion law. My name is Khawla*, I am 42 years old and I am a midwife and university lecturer. I have been married for 10 years and have three children, two boys and a girl. I have multiple health issues and a number of hereditary conditions in my family. I first became involved with PFPPA through my work, having taken many trainings with them about issues such as early marriage, gender-based violence, sexual health and safe abortion. Then last year I accidentally became pregnant myself. My youngest child was just two years old, I had a new job at the time and was suffering with a number of health issues that would make another pregnancy dangerous for me. Unintended pregnancy When I read that the pregnancy test was positive, it was a very hard time. I started crying – I felt like the world was very black – it was the end of my life. I would kill myself, if I didn’t end this pregnancy. So I came to PFPPA and they treated me as a client. I met with the social worker, midwife and doctor and, since the pregnancy was risk to my life and I was very weak and bleeding when I reached them they were able to prescribe the tablets. These pills are highly regulated and restricted here and not all pharmacists stock them but I was able to access them with the prescription and they worked. PFPPA provided follow up afterwards helping me to find an effective long-acting family planning method. Even though I knew about the different methods, they discussed them all with me to ensure that they would be appropriate for my health. Even though the law allows abortion in cases of risks to health of the woman, you need to get permission from the religious leaders and they are very hard to convince. I took my case to them and, despite my health issues, they refused despite it being very early in the pregnancy, before the ensoulment and is allowed according to Islam. The public hospital will not perform it unless they receive the permission from the religious leaders and they don’t give it despite what the religious rules say. Stigma & access From my experience the situation in relation to abortion in Palestine is very hard. There are many women who get pregnant who did not plan it and it’s not the time for the pregnancy. The door is closed to them from the public health system. I have started to campaign on this issue now, I talk to the students in my course about how we can solve this problem. I think the stigma is very difficult. I never thought I would be in this situation, I talked a lot about it before but when you are in the situation, it is totally different. I really appreciated the help given from the PFPPA team, particularly the psychological support. When I felt bad, they helped me to see that I was doing the right thing and it was my right. Read more stories from SAAF in Palestine *Not her real name
| 22 August 2018
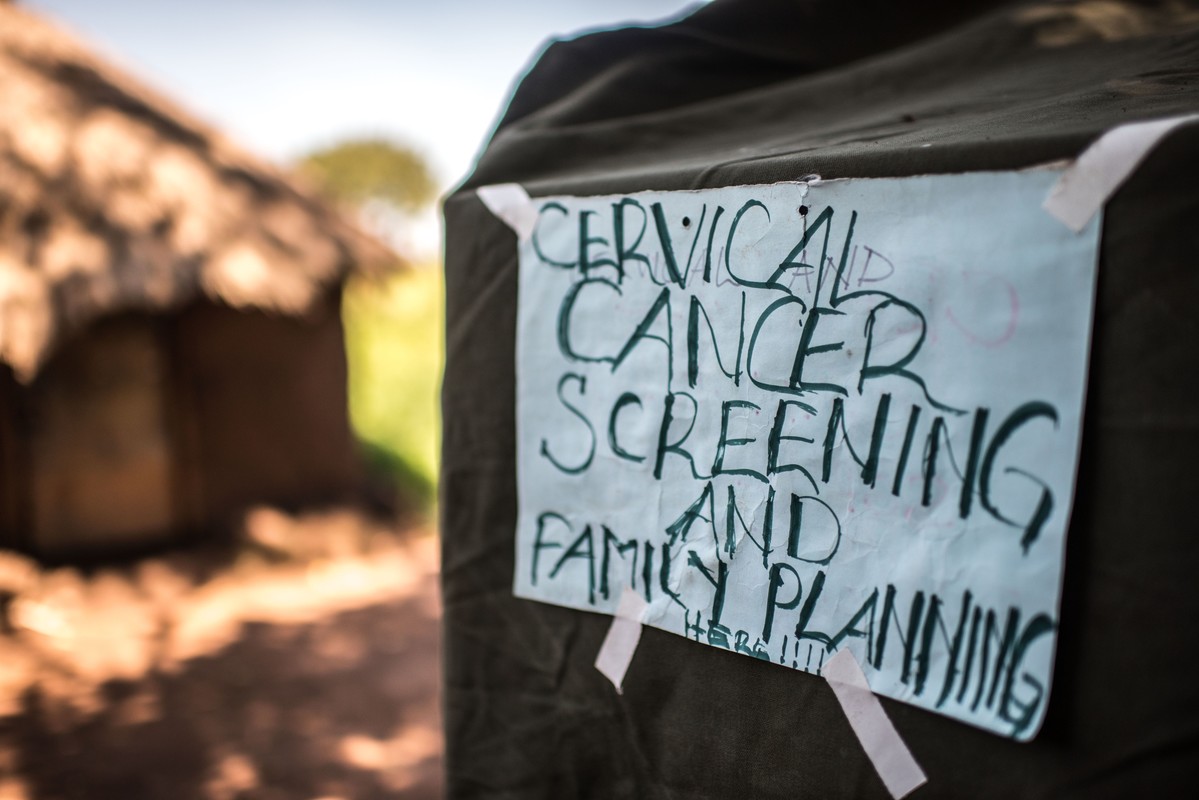
“A radio announcement saved my life” – Gertrude’s story
Gertrude Mugala is a teacher in Fort Portal, a town in Western Uganda. While Gertrude considered herself fairly knowledgeable about cancer, she had never considered taking a screening test or imagined herself ever having the disease. Then one day, she heard an announcement on the radio urging women to go for cervical cancer screenings at a Reproductive Health Uganda (RHU) clinic. “The radio presenter was talking about cervical cancer, and in her message she encouraged all women to get screened. I decided to go and try it out,” she said. Gertrude made her way to RHU's Fort Portal Branch clinic for the free cervical cancer screening. There, she met Ms. Irene Kugonza, an RHU service provider. Ms. Kugonza educated Gertrude and a group of other women about cervical cancer and the importance of routine screening. Gertrude received a type of cervical cancer screening called VIA (visual inspection with acetic acid). "I did not know what was happening" But Gertrude's results were not what she expected; she received a positive result. The good news, however, is that precancerous lesions can be treated if detected early. “I was so shaken when I was told I had pre-cancerous lesions. I did not know what was happening and I didn't believe what I was hearing. I had no idea of my health status. I thought I was healthy, but I was actually harbouring a potential killer disease in me. What would have happened if I didn't go for the screening? If I hadn't heard the radio announcement?” Gertrude was then referred for cryotherapy. “Following cryotherapy, I am now in the process of healing, and I am supposed to go back for review after three months,” said Gertrude. Community screenings Today, Gertrude advocates for cervical cancer screening in her community. She talks to women about cancer, especially cervical cancer, at her workplace, at the market, in meetings, and any other opportunity she gets. “I decided to let women know that cervical cancer is real and it is here with us, and that it kills. At the moment, those are the platforms I have, and I will continue educating women about cancer and encourage them to go for routine testing. I am also happy that I was near my radio that day, where I heard that announcement encouraging all women to get tested for cervical cancer. It might be because of that radio announcement that I am here today,” she said.
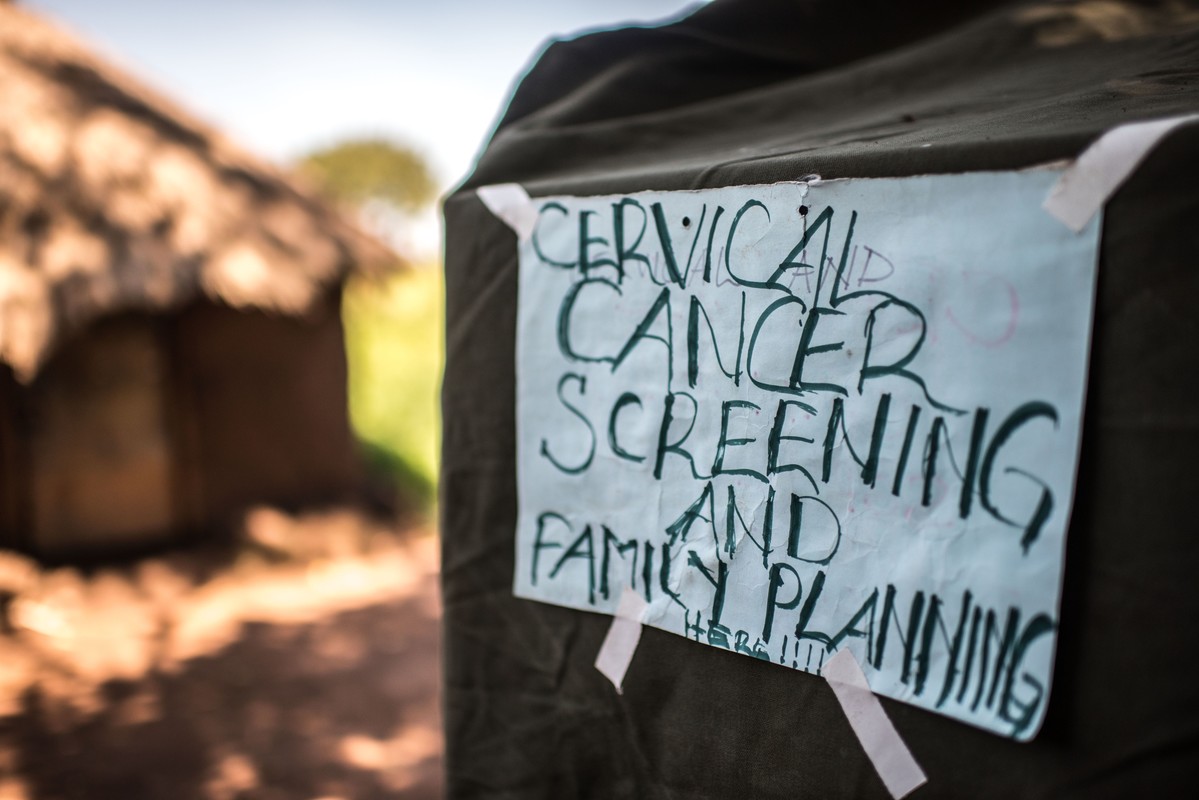
| 16 May 2025
“A radio announcement saved my life” – Gertrude’s story
Gertrude Mugala is a teacher in Fort Portal, a town in Western Uganda. While Gertrude considered herself fairly knowledgeable about cancer, she had never considered taking a screening test or imagined herself ever having the disease. Then one day, she heard an announcement on the radio urging women to go for cervical cancer screenings at a Reproductive Health Uganda (RHU) clinic. “The radio presenter was talking about cervical cancer, and in her message she encouraged all women to get screened. I decided to go and try it out,” she said. Gertrude made her way to RHU's Fort Portal Branch clinic for the free cervical cancer screening. There, she met Ms. Irene Kugonza, an RHU service provider. Ms. Kugonza educated Gertrude and a group of other women about cervical cancer and the importance of routine screening. Gertrude received a type of cervical cancer screening called VIA (visual inspection with acetic acid). "I did not know what was happening" But Gertrude's results were not what she expected; she received a positive result. The good news, however, is that precancerous lesions can be treated if detected early. “I was so shaken when I was told I had pre-cancerous lesions. I did not know what was happening and I didn't believe what I was hearing. I had no idea of my health status. I thought I was healthy, but I was actually harbouring a potential killer disease in me. What would have happened if I didn't go for the screening? If I hadn't heard the radio announcement?” Gertrude was then referred for cryotherapy. “Following cryotherapy, I am now in the process of healing, and I am supposed to go back for review after three months,” said Gertrude. Community screenings Today, Gertrude advocates for cervical cancer screening in her community. She talks to women about cancer, especially cervical cancer, at her workplace, at the market, in meetings, and any other opportunity she gets. “I decided to let women know that cervical cancer is real and it is here with us, and that it kills. At the moment, those are the platforms I have, and I will continue educating women about cancer and encourage them to go for routine testing. I am also happy that I was near my radio that day, where I heard that announcement encouraging all women to get tested for cervical cancer. It might be because of that radio announcement that I am here today,” she said.

| 21 May 2017
A graduate in need turns to sex work
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Lady Mermaid's Bureau. I am Pretty Lynn, aged 25. I am a sex worker but I went to university. I graduated with a Bachelor's Degree in Tourism in 2013. But now, during the day I’m sleeping and during the night I’m working. That is how my day goes every day. I got into sex work through friends. Okay it is not good but I am earning. I tried to get a job when I graduated. I have been applying since I graduated in 2013. I’m still applying but I’m not getting anywhere. You know to get jobs in Uganda; you have to know someone there and no one knows me there. To be a sex worker is like a curse. People look at you like, I don’t know, as someone that has no use in society. People look at you in a bad way. They even don’t consider why you are selling. They just see you as the worst thing that can happen in the society. So it is not comfortable, it is really hard but we try and survive. The fact sex working is illegal means you have to hide yourself when you are selling so that police cannot take you. And then you get diseases, men don’t want to pay. When the police come and take us, sometimes they even use us and don’t pay. So it is really hard. They want a free service. Like if they come and take you and pay that would be fair. But they say it is illegal to sell yourself. But they still use you yet they are saying it is illegal. You can’t report the police because there is no evidence. Abortion and unwanted pregnancies are really common because men don’t want to use condoms and female condoms are really rare and they are expensive. Though at times we get female condoms from Lady Marmaid’s Bureau (LMB) because there are so many of us they can’t keep on giving you them all the time. At times when we get pregnant we use local methods. You can go and use local herbs but it is not safe. One time I used local herbs and I was successful. Then the other time I used Omo washing powder and tea leaves but it was really hard for me. I almost died. I had a friend who died last year from this. But the good thing is that LMB taught us about safe abortion. I have had a safe abortion too. There are some tabs they are called Miso (misoprostol). It costs about fifty thousand shillings (£10 pounds or $20.) It is a lot of money. But if I’m working and I know I’m pregnant, I can say, "this week I’m working for my safe abortion". So if I’m working for twenty thousand, by the end of the week I will have the money. It is expensive compared to Omo at five hundred shillings but that is risky. So if I say I will work this whole week for Miso (misoprostol) it is better. But I'm working and I'm not eating. A project like this one from Lady Mermaid's can help young girls and women. But to take us from sex work, it would really be hard. They would not have enough money to cater for all of us. So what they have to do is to teach us how to protect ourselves, how to defend ourselves. Safe abortion yes. They will just have to sensitise us more about our lives, protection, female condoms and all that. I don't have a boyfriend but maybe when I get money and leave this job I will. But for now, no man would like a woman who sells. No man will bear the wife selling herself. And that will happen only if I get funds, settle somewhere else and become responsible woman. I don’t want this job. I don’t want to be in this business of sex work all the time. I want be married, with my children happily, not selling myself. Stories Read more stories about the amazing success of SAAF in Uganda

| 15 May 2025
A graduate in need turns to sex work
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Lady Mermaid's Bureau. I am Pretty Lynn, aged 25. I am a sex worker but I went to university. I graduated with a Bachelor's Degree in Tourism in 2013. But now, during the day I’m sleeping and during the night I’m working. That is how my day goes every day. I got into sex work through friends. Okay it is not good but I am earning. I tried to get a job when I graduated. I have been applying since I graduated in 2013. I’m still applying but I’m not getting anywhere. You know to get jobs in Uganda; you have to know someone there and no one knows me there. To be a sex worker is like a curse. People look at you like, I don’t know, as someone that has no use in society. People look at you in a bad way. They even don’t consider why you are selling. They just see you as the worst thing that can happen in the society. So it is not comfortable, it is really hard but we try and survive. The fact sex working is illegal means you have to hide yourself when you are selling so that police cannot take you. And then you get diseases, men don’t want to pay. When the police come and take us, sometimes they even use us and don’t pay. So it is really hard. They want a free service. Like if they come and take you and pay that would be fair. But they say it is illegal to sell yourself. But they still use you yet they are saying it is illegal. You can’t report the police because there is no evidence. Abortion and unwanted pregnancies are really common because men don’t want to use condoms and female condoms are really rare and they are expensive. Though at times we get female condoms from Lady Marmaid’s Bureau (LMB) because there are so many of us they can’t keep on giving you them all the time. At times when we get pregnant we use local methods. You can go and use local herbs but it is not safe. One time I used local herbs and I was successful. Then the other time I used Omo washing powder and tea leaves but it was really hard for me. I almost died. I had a friend who died last year from this. But the good thing is that LMB taught us about safe abortion. I have had a safe abortion too. There are some tabs they are called Miso (misoprostol). It costs about fifty thousand shillings (£10 pounds or $20.) It is a lot of money. But if I’m working and I know I’m pregnant, I can say, "this week I’m working for my safe abortion". So if I’m working for twenty thousand, by the end of the week I will have the money. It is expensive compared to Omo at five hundred shillings but that is risky. So if I say I will work this whole week for Miso (misoprostol) it is better. But I'm working and I'm not eating. A project like this one from Lady Mermaid's can help young girls and women. But to take us from sex work, it would really be hard. They would not have enough money to cater for all of us. So what they have to do is to teach us how to protect ourselves, how to defend ourselves. Safe abortion yes. They will just have to sensitise us more about our lives, protection, female condoms and all that. I don't have a boyfriend but maybe when I get money and leave this job I will. But for now, no man would like a woman who sells. No man will bear the wife selling herself. And that will happen only if I get funds, settle somewhere else and become responsible woman. I don’t want this job. I don’t want to be in this business of sex work all the time. I want be married, with my children happily, not selling myself. Stories Read more stories about the amazing success of SAAF in Uganda

| 15 May 2017
All of the clients, all of the time: Our staff never turn anyone away
At the end of a long day, Anicia, closes the clinic with praise for her colleagues who never turn anyone away. "We open at 8am. From 8am we will be receiving a variety of clients for different services - whether post-abortion care, whether antenatal care - we have to give them all the services. We may end up to 10pm, because we'll never chase our clients, we'll never close the place when we have a client inside. People come when they have no hope. You receive them, and you give them hope by treating them properly and giving them quality services. The client gets better and will never forget you. And follow them up on the phone. "How are you doing?" It's good for us to know that they're doing well. Others even tell us 'The way you handle us, we love it so much'." Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE

| 15 May 2025
All of the clients, all of the time: Our staff never turn anyone away
At the end of a long day, Anicia, closes the clinic with praise for her colleagues who never turn anyone away. "We open at 8am. From 8am we will be receiving a variety of clients for different services - whether post-abortion care, whether antenatal care - we have to give them all the services. We may end up to 10pm, because we'll never chase our clients, we'll never close the place when we have a client inside. People come when they have no hope. You receive them, and you give them hope by treating them properly and giving them quality services. The client gets better and will never forget you. And follow them up on the phone. "How are you doing?" It's good for us to know that they're doing well. Others even tell us 'The way you handle us, we love it so much'." Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE

| 15 May 2017
Getting services to the most remote areas in Uganda
Every Thursday a team from RHU Gulu district provides a mobile outreach clinic in Atega village in the Omoro district in Northern Uganda. The outreach team goes out into this poor, remote area which would otherwise not have access to sexual and reproductive health services. The night before the outreach clinic RHU driver, Robert Nyeko and Godfrey Bedimot load up tents, chairs, medical equipment and supplies. The clinic needs to be set up and by 7am ready to receive clients from 8am. The outreach clinic provides a range of services including diagnosis, testing and treatment, family planning such as fitting implants, providing condoms and HPV vaccines. Laboratory technician, Denis Bongonyinge carries out testing for malaria, Hepatitis B, HIV/AIDS, pneumonia and other infections. Other members of the team provide immunisations and vaccinations. Typically men, women and children start arriving at the clinic by 7:30am. Two volunteers are on hand to direct them to the appropriate place to get the services they need. Some clients need a range of services. At 8am service provider, Anicia Filda, popularly known a 'Mama' in the community is ready with her team to start the day. There are now more than 200 clients waiting to be seen; with more people arriving to join the long queues. The longest queue is for the immunisation and vaccination services. The majority have come for either the Hepatitis B vaccine, which is a big threat in this community. Priority is given to the many young girls lining up for the Human Papilloma Virus (HPV) vaccine. Denis Bongonyinge takes blood samples for rapid tests for malaria, HIV, HPV and a range of other infections. Each client carries an exercise book where Denis records their results which is then taken to the staff giving out prescriptions. 32-year-Robert Otim pushes his bicycle to the outreach clinic. The single father has ridden 10 kilometres with his two young children. He lost his wife to Hepatitis B when their daughter was just six months. His four-year-old son was born prematurely and is now disabled. He has come today for his last Hepatitis B immunisation. His children need to be vaccinated as well as treated for malaria and coughs. Looking at the long queue, he says he doubts whether he will get the service today but he is lucky as one of the team who once treated his son, Geoffrey, notices Robert and they are given priority for treatment and prescriptions. Already by midday, one of the teams delivering minor surgeries, postnatal services, family planning and post abortion care have seen 47 mothers. This is almost the same as the number of clients they would treat at the Gulu Clinic during a normal day. Anicia Filda sends the driver to collect more supplies from the clinic; the stock is starting to run low because demand is so high There is no break for the team. Samuel Kedi, the only clinician at the outreach camp stands up, and picks up a bottle of water from his backpack for a quick drink before continuing with the next client. The clinic continues to see clients well into the evening. The outreach clinic is scheduled to finish by 5pm but Anicia says there is not one day they have closed on time: “We cannot close when clients are still lining up. It’s the same at the clinic in Gulu,” she says. As the clinic draws to a close for the day, the teams complete their report which records details of the numbers clients served, the types of services delivered and supplies of stock. It has been another busy but successful day for Anicia and her team. Provision of integrated services in such remote areas is vital for the local community; many men, women and children would not be able to receive the types of treatment and care that RHU works diligently to provide. Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE

| 16 May 2025
Getting services to the most remote areas in Uganda
Every Thursday a team from RHU Gulu district provides a mobile outreach clinic in Atega village in the Omoro district in Northern Uganda. The outreach team goes out into this poor, remote area which would otherwise not have access to sexual and reproductive health services. The night before the outreach clinic RHU driver, Robert Nyeko and Godfrey Bedimot load up tents, chairs, medical equipment and supplies. The clinic needs to be set up and by 7am ready to receive clients from 8am. The outreach clinic provides a range of services including diagnosis, testing and treatment, family planning such as fitting implants, providing condoms and HPV vaccines. Laboratory technician, Denis Bongonyinge carries out testing for malaria, Hepatitis B, HIV/AIDS, pneumonia and other infections. Other members of the team provide immunisations and vaccinations. Typically men, women and children start arriving at the clinic by 7:30am. Two volunteers are on hand to direct them to the appropriate place to get the services they need. Some clients need a range of services. At 8am service provider, Anicia Filda, popularly known a 'Mama' in the community is ready with her team to start the day. There are now more than 200 clients waiting to be seen; with more people arriving to join the long queues. The longest queue is for the immunisation and vaccination services. The majority have come for either the Hepatitis B vaccine, which is a big threat in this community. Priority is given to the many young girls lining up for the Human Papilloma Virus (HPV) vaccine. Denis Bongonyinge takes blood samples for rapid tests for malaria, HIV, HPV and a range of other infections. Each client carries an exercise book where Denis records their results which is then taken to the staff giving out prescriptions. 32-year-Robert Otim pushes his bicycle to the outreach clinic. The single father has ridden 10 kilometres with his two young children. He lost his wife to Hepatitis B when their daughter was just six months. His four-year-old son was born prematurely and is now disabled. He has come today for his last Hepatitis B immunisation. His children need to be vaccinated as well as treated for malaria and coughs. Looking at the long queue, he says he doubts whether he will get the service today but he is lucky as one of the team who once treated his son, Geoffrey, notices Robert and they are given priority for treatment and prescriptions. Already by midday, one of the teams delivering minor surgeries, postnatal services, family planning and post abortion care have seen 47 mothers. This is almost the same as the number of clients they would treat at the Gulu Clinic during a normal day. Anicia Filda sends the driver to collect more supplies from the clinic; the stock is starting to run low because demand is so high There is no break for the team. Samuel Kedi, the only clinician at the outreach camp stands up, and picks up a bottle of water from his backpack for a quick drink before continuing with the next client. The clinic continues to see clients well into the evening. The outreach clinic is scheduled to finish by 5pm but Anicia says there is not one day they have closed on time: “We cannot close when clients are still lining up. It’s the same at the clinic in Gulu,” she says. As the clinic draws to a close for the day, the teams complete their report which records details of the numbers clients served, the types of services delivered and supplies of stock. It has been another busy but successful day for Anicia and her team. Provision of integrated services in such remote areas is vital for the local community; many men, women and children would not be able to receive the types of treatment and care that RHU works diligently to provide. Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE

| 15 May 2017
Joyce's story - empowering disabled clients with services in rural communities
Joyce Auma, 25, is a business administration graduate currently working as a data clerk with Gulu Women with Disabilities Union. The union has partnered with Reproductive Health Uganda to extend sexual and reproductive health services to women living with disabilities in Gulu and neighbouring districts in Acholi. Joyce, who lost the use of her legs in childhood, is one of the women with disabilities that normally receive services at Gulu Clinic. “I found out about RHU because they are our partners at Gulu Women with Disability Union. I first came to the clinic to test for HIV and other STIs. We also receive their other services like family planning and cancer screening to people with disabilities.” “The first time I came here I was warmly welcomed. They're very good at talking to the youth. Though the place was new for me, I was given service as if it was not my first time.” Says Joyce. "Us people with disabilities have challenges at the main hospitals. People around look at you as if you are not a human being and you don’t fall sick.” Joyce has since been a regular client of RHU for HIV testing, cancer screening and other diseases. She says her status exposes her to many risks of infection which has to be regularly checked for. “I always come here for testing, there is also cancer screening. They don’t segregate me because of my disability. They give you the services you need.” Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE

| 16 May 2025
Joyce's story - empowering disabled clients with services in rural communities
Joyce Auma, 25, is a business administration graduate currently working as a data clerk with Gulu Women with Disabilities Union. The union has partnered with Reproductive Health Uganda to extend sexual and reproductive health services to women living with disabilities in Gulu and neighbouring districts in Acholi. Joyce, who lost the use of her legs in childhood, is one of the women with disabilities that normally receive services at Gulu Clinic. “I found out about RHU because they are our partners at Gulu Women with Disability Union. I first came to the clinic to test for HIV and other STIs. We also receive their other services like family planning and cancer screening to people with disabilities.” “The first time I came here I was warmly welcomed. They're very good at talking to the youth. Though the place was new for me, I was given service as if it was not my first time.” Says Joyce. "Us people with disabilities have challenges at the main hospitals. People around look at you as if you are not a human being and you don’t fall sick.” Joyce has since been a regular client of RHU for HIV testing, cancer screening and other diseases. She says her status exposes her to many risks of infection which has to be regularly checked for. “I always come here for testing, there is also cancer screening. They don’t segregate me because of my disability. They give you the services you need.” Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE

| 15 May 2017
Breaking gender taboos
After two years of struggling to conceive Brenda Abalo and her husband, Francis Opio, decided to visit Reproductive Health Uganda's clinic in Gulu. Much as there is progressive attitude to modern medicine in this northern Uganda region, fertility treatment remains a sensitive issue for both men and women. Anxious in the waiting room, Francis said he had decided to come to RHU with his wife because he heard their radio show about a similar problem. In addition to fertility treatments, the couple was also given counselling and treatment for another condition. “After sex, my wife was in pain. She was complaining a lot three weeks ago. I also felt some itches. They have given us treatment which we are still continuing with,” said Francis. The couple was given information to ensure that Brenda was in the best possible health to conceive. She is to undergo treatment to reduce the prolactin level in the blood and correct the hormonal imbalance. “This is not my first time at this clinic," says Brenda. “The service here is better in comparison with other health centres. They give much better attention to the patient.” “RHU has been supporting a lot of people. They helped a friend of mine; she was having a problem with miscarriage. So she came here and got properly treated” Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE

| 16 May 2025
Breaking gender taboos
After two years of struggling to conceive Brenda Abalo and her husband, Francis Opio, decided to visit Reproductive Health Uganda's clinic in Gulu. Much as there is progressive attitude to modern medicine in this northern Uganda region, fertility treatment remains a sensitive issue for both men and women. Anxious in the waiting room, Francis said he had decided to come to RHU with his wife because he heard their radio show about a similar problem. In addition to fertility treatments, the couple was also given counselling and treatment for another condition. “After sex, my wife was in pain. She was complaining a lot three weeks ago. I also felt some itches. They have given us treatment which we are still continuing with,” said Francis. The couple was given information to ensure that Brenda was in the best possible health to conceive. She is to undergo treatment to reduce the prolactin level in the blood and correct the hormonal imbalance. “This is not my first time at this clinic," says Brenda. “The service here is better in comparison with other health centres. They give much better attention to the patient.” “RHU has been supporting a lot of people. They helped a friend of mine; she was having a problem with miscarriage. So she came here and got properly treated” Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE

| 29 December 2023
In their own words: The people providing sexual and reproductive health care under bombardment in Gaza
Week after week, heavy Israeli bombardment from air, land, and sea, has continued across most of the Gaza Strip. According to the Ministry of Health, at least 21,320 Palestinians have been killed in Gaza since October 7th, about 70% of whom are women and children. Nearly 2 million people have been displaced from their homes, forced to live in extremely overcrowded and unsanitary shelters. The Ministry of Health says that 50% of pregnant women in the shelters suffer from thirst and malnutrition, and there is a lack of health care and vaccinations for newborns. The suffering is unimaginable, yet it is all too real. Many of those bearing witness to the seemingly endless death and misery are frontline healthcare workers - including those delivering sexual and reproductive healthcare. But they, too, are at risk of being killed just for doing their jobs. Israel continues to bombard Gaza’s health facilities and residential areas, despite mounting international pressure for a ceasefire - something IPPF and many other humanitarian organisations have been demanding for months. According to the World Health Organization (WHO) there have been more than 200 Israeli attacks on hospitals and ambulances since Oct. 7, with many medical workers detained during Israeli raids. At least 300 healthcare workers have been reported killed, according to the UN. This is more than the total number of health worker deaths recorded across all countries in conflict last year, and in any single year since 2016. Staff at IPPF's local member association, the Palestinian Family Planning and Protection Association (PFPPA), are among the heroic healthcare workers in Gaza that continue to provide care as best they can in the ongoing humanitarian catastrophe. We fear for their safety - and that of the 2.3 million civilians in Gaza - every single day. In their own words, PFPPA and other health workers describe what it's like to provide care under bombardment and blockade in Gaza and in the West Bank - offering glimpses of terror, devastation, and even some hope.

| 29 December 2023
In their own words: The people providing sexual and reproductive health care under bombardment in Gaza
Week after week, heavy Israeli bombardment from air, land, and sea, has continued across most of the Gaza Strip. According to the Ministry of Health, at least 21,320 Palestinians have been killed in Gaza since October 7th, about 70% of whom are women and children. Nearly 2 million people have been displaced from their homes, forced to live in extremely overcrowded and unsanitary shelters. The Ministry of Health says that 50% of pregnant women in the shelters suffer from thirst and malnutrition, and there is a lack of health care and vaccinations for newborns. The suffering is unimaginable, yet it is all too real. Many of those bearing witness to the seemingly endless death and misery are frontline healthcare workers - including those delivering sexual and reproductive healthcare. But they, too, are at risk of being killed just for doing their jobs. Israel continues to bombard Gaza’s health facilities and residential areas, despite mounting international pressure for a ceasefire - something IPPF and many other humanitarian organisations have been demanding for months. According to the World Health Organization (WHO) there have been more than 200 Israeli attacks on hospitals and ambulances since Oct. 7, with many medical workers detained during Israeli raids. At least 300 healthcare workers have been reported killed, according to the UN. This is more than the total number of health worker deaths recorded across all countries in conflict last year, and in any single year since 2016. Staff at IPPF's local member association, the Palestinian Family Planning and Protection Association (PFPPA), are among the heroic healthcare workers in Gaza that continue to provide care as best they can in the ongoing humanitarian catastrophe. We fear for their safety - and that of the 2.3 million civilians in Gaza - every single day. In their own words, PFPPA and other health workers describe what it's like to provide care under bombardment and blockade in Gaza and in the West Bank - offering glimpses of terror, devastation, and even some hope.

| 04 April 2019
"Women in our communities use many unsafe methods to try to end pregnancies"
Women and girls in Palestine face a number of difficulties and challenges. The ongoing conflict and lack of sitting government as well as high unemployment, has led to poverty and inequality, while an increasingly conservative society and traditionally patriarchal culture has led to increased gender-inequality and lack of access to sexual and reproductive healthcare. The current abortion law unfairly pushes women to risk their lives and health to attempt to end their unwanted pregnancies in unsafe ways. In this context, the Palestinian Family Planning and Protection Agency (PFPPA) has been working since 1964, to provide sexual and reproductive healthcare and advocate for women’s rights. Having received two grants from Safe Abortion Action Fund (SAAF) since 2014, they have been working on the lack of access to safe abortion in the country with a focus on increasing their provision of abortion-related services and advocating at community and national level for changes to the abortion law. My name is Fatima, I am a midwife and have worked with PFPPA for 18 years in the Halhul clinic in Palestine. PFPPA has had a great impact on me personally as well as the community as a whole. I experienced violence in my marriage but when I joined the organization I learned the meaning of violence and I realized that I didn’t have to put up with it and could make decisions for myself. This was a turning point in my life. My life changed 180 degrees, thank God, and my husband stopped being violent. Society & acceptance Since I have worked here, I have seen changes in society’s acceptance of sexual and reproductive health issues and I feel that more people are supporting us. They can be women, religious personalities or young volunteers. One of the proudest moments of my work has been working with a young man who was training to be a peer educator, he was violent, especially with his sister. From the very start of the training, he was against the issues that we were presenting, however, he started to understand our issues. I also met his mother and she thanked me for the change that happened in his life. She came to say that he is now helping in the house - washing dishes and doing other tasks that he would have thought were just for women before. The challenges that we face are a misunderstanding of religion, negative traditions and customs, as well as the political situation in Palestine with the occupation, the walls, the checkpoints as well as the economic situation. We work on issues that will take many years to witness any change due to the negative traditions and customs. Harm reduction & abortion care We have recently started implementing a harm reduction approach to abortion care. I remember one woman who was 44 years old and divorced. She came to the clinic and was seven weeks pregnant. Her face was pale and tired...I felt that all the problems were on her shoulders. She was looking for a saviour. We supported her with harm reduction information and afterwards provided information on post-abortion contraception. After one or two months she sent a message thanking me, saying that we had saved her life, I was really happy about that. There are also cases of women that come here, maybe they took pills or they did something that made them bleed. They don’t tell you what they did but I can detect if I think an abortion happened. If it is an incomplete abortion, we explain how to take the treatment and we follow up with support. Unsafe methods Women in our communities use many unsafe methods to try to end pregnancies. They drink special teas or chlorine. They jump off things or ask their children to jump on them. They sometimes put suppositories made from Arabic medicinal herbs into the cervix. Although it is common, deaths are not registered as linked to unsafe abortion but are probably registered as maternal deaths. When the society says that abortion is haram (forbidden), they don’t take into consideration the issues and these women in need. Imagine if we had safe abortion services at the hospitals, we would not see these issues at all. There are women who would choose abortion for reasons like their age, their health, social issues and psychological issues. There are women themselves who say “I will die if I complete this pregnancy”. I am passionate about the work that I do. I advocate for these issues everywhere I go, on the bus, during weddings and with friends and family, wherever I go. That is why the Safe Abortion Action Fund (SAAF) funded project is so important. I have learned a lot about advocacy and campaigning, how we manage legal advocacy and how to work with decision-makers. We have run events to mark International Safe Abortion Day with groups of women gathered here in the centre and with decision-makers and volunteers. Read more stories from SAAF in Palestine

| 15 May 2025
"Women in our communities use many unsafe methods to try to end pregnancies"
Women and girls in Palestine face a number of difficulties and challenges. The ongoing conflict and lack of sitting government as well as high unemployment, has led to poverty and inequality, while an increasingly conservative society and traditionally patriarchal culture has led to increased gender-inequality and lack of access to sexual and reproductive healthcare. The current abortion law unfairly pushes women to risk their lives and health to attempt to end their unwanted pregnancies in unsafe ways. In this context, the Palestinian Family Planning and Protection Agency (PFPPA) has been working since 1964, to provide sexual and reproductive healthcare and advocate for women’s rights. Having received two grants from Safe Abortion Action Fund (SAAF) since 2014, they have been working on the lack of access to safe abortion in the country with a focus on increasing their provision of abortion-related services and advocating at community and national level for changes to the abortion law. My name is Fatima, I am a midwife and have worked with PFPPA for 18 years in the Halhul clinic in Palestine. PFPPA has had a great impact on me personally as well as the community as a whole. I experienced violence in my marriage but when I joined the organization I learned the meaning of violence and I realized that I didn’t have to put up with it and could make decisions for myself. This was a turning point in my life. My life changed 180 degrees, thank God, and my husband stopped being violent. Society & acceptance Since I have worked here, I have seen changes in society’s acceptance of sexual and reproductive health issues and I feel that more people are supporting us. They can be women, religious personalities or young volunteers. One of the proudest moments of my work has been working with a young man who was training to be a peer educator, he was violent, especially with his sister. From the very start of the training, he was against the issues that we were presenting, however, he started to understand our issues. I also met his mother and she thanked me for the change that happened in his life. She came to say that he is now helping in the house - washing dishes and doing other tasks that he would have thought were just for women before. The challenges that we face are a misunderstanding of religion, negative traditions and customs, as well as the political situation in Palestine with the occupation, the walls, the checkpoints as well as the economic situation. We work on issues that will take many years to witness any change due to the negative traditions and customs. Harm reduction & abortion care We have recently started implementing a harm reduction approach to abortion care. I remember one woman who was 44 years old and divorced. She came to the clinic and was seven weeks pregnant. Her face was pale and tired...I felt that all the problems were on her shoulders. She was looking for a saviour. We supported her with harm reduction information and afterwards provided information on post-abortion contraception. After one or two months she sent a message thanking me, saying that we had saved her life, I was really happy about that. There are also cases of women that come here, maybe they took pills or they did something that made them bleed. They don’t tell you what they did but I can detect if I think an abortion happened. If it is an incomplete abortion, we explain how to take the treatment and we follow up with support. Unsafe methods Women in our communities use many unsafe methods to try to end pregnancies. They drink special teas or chlorine. They jump off things or ask their children to jump on them. They sometimes put suppositories made from Arabic medicinal herbs into the cervix. Although it is common, deaths are not registered as linked to unsafe abortion but are probably registered as maternal deaths. When the society says that abortion is haram (forbidden), they don’t take into consideration the issues and these women in need. Imagine if we had safe abortion services at the hospitals, we would not see these issues at all. There are women who would choose abortion for reasons like their age, their health, social issues and psychological issues. There are women themselves who say “I will die if I complete this pregnancy”. I am passionate about the work that I do. I advocate for these issues everywhere I go, on the bus, during weddings and with friends and family, wherever I go. That is why the Safe Abortion Action Fund (SAAF) funded project is so important. I have learned a lot about advocacy and campaigning, how we manage legal advocacy and how to work with decision-makers. We have run events to mark International Safe Abortion Day with groups of women gathered here in the centre and with decision-makers and volunteers. Read more stories from SAAF in Palestine

| 03 April 2019
"The students don’t normally ask about abortion as it is such a taboo"
Women and girls in Palestine face a number of difficulties and challenges. The ongoing conflict and lack of sitting government as well as high unemployment, has led to poverty and inequality, while an increasingly conservative society and traditionally patriarchal culture has led to increased gender-inequality and lack of access to sexual and reproductive healthcare. The current abortion law unfairly pushes women to risk their lives and health to attempt to end their unwanted pregnancies in unsafe ways. In this context, the Palestinian Family Planning and Protection Agency (PFPPA) has been working since 1964, to provide sexual and reproductive healthcare and advocate for women’s rights. Having received two grants from Safe Abortion Action Fund (SAAF) since 2014, they have been working on the lack of access to safe abortion in the country with a focus on increasing their provision of abortion-related services and advocating at community and national level for changes to the abortion law. My name is Amani and I am 24 years old. I live with my parents in Bethlehem in the West Bank and I work as a midwife in a family hospital in Jerusalem as well as a peer education volunteer with the Palestinian Family Planning and Protection Agency. Working in schools Part of my role as a volunteer involves going to schools and doing presentations about early-marriage, family planning and gender-based violence. Even though sex outside of marriage is taboo, it does happen. However, it is very hard for unmarried people to access contraception as the culture is so restrictive, especially here in Hebron. When they need contraception, the man usually goes by himself or they look online. When we go to schools and talk to students about the subject of sexual health, the students want to know more because at home it is a taboo to talk about such things. We get many questions about issues such as masturbation or what causes pregnancy. They just know that it happens when men and women are together, they do not know how it happens. So people may ask a question like: ‘if I touch somebody, if I stand near someone or kiss them will I get pregnant?’ Abortion is still a taboo The students don’t normally ask about abortion as it is such a taboo. I do know that unsafe abortion happens though, for example my grandmother tried to end her pregnancy once. She was forty-five years old and had six children already. She did not know any way of not getting pregnant or safely ending the pregnancy. She told me that she drank liquids and jumped from the stairs, taking a great risk. She really didn’t want to be pregnant again and tried hard to end it but it did not work. I am very proud that as a peer educator I have expanded my knowledge on many issues, including how to provide harm reduction information to women so that they can reduce risks of unsafe abortion and not do what my grandmother did in case they don’t want to be pregnant. Once I met with a woman who already had six children, she was tired of having children but her husband wanted to have more so we visited them at home and through conversation, the husband understood the need, so she was able to access an IUD. Here we work a lot with women, we change them, we speak with them, they change their opinions, they become decision-makers and they leave the clinic as different people. Read more stories from SAAF in Palestine

| 15 May 2025
"The students don’t normally ask about abortion as it is such a taboo"
Women and girls in Palestine face a number of difficulties and challenges. The ongoing conflict and lack of sitting government as well as high unemployment, has led to poverty and inequality, while an increasingly conservative society and traditionally patriarchal culture has led to increased gender-inequality and lack of access to sexual and reproductive healthcare. The current abortion law unfairly pushes women to risk their lives and health to attempt to end their unwanted pregnancies in unsafe ways. In this context, the Palestinian Family Planning and Protection Agency (PFPPA) has been working since 1964, to provide sexual and reproductive healthcare and advocate for women’s rights. Having received two grants from Safe Abortion Action Fund (SAAF) since 2014, they have been working on the lack of access to safe abortion in the country with a focus on increasing their provision of abortion-related services and advocating at community and national level for changes to the abortion law. My name is Amani and I am 24 years old. I live with my parents in Bethlehem in the West Bank and I work as a midwife in a family hospital in Jerusalem as well as a peer education volunteer with the Palestinian Family Planning and Protection Agency. Working in schools Part of my role as a volunteer involves going to schools and doing presentations about early-marriage, family planning and gender-based violence. Even though sex outside of marriage is taboo, it does happen. However, it is very hard for unmarried people to access contraception as the culture is so restrictive, especially here in Hebron. When they need contraception, the man usually goes by himself or they look online. When we go to schools and talk to students about the subject of sexual health, the students want to know more because at home it is a taboo to talk about such things. We get many questions about issues such as masturbation or what causes pregnancy. They just know that it happens when men and women are together, they do not know how it happens. So people may ask a question like: ‘if I touch somebody, if I stand near someone or kiss them will I get pregnant?’ Abortion is still a taboo The students don’t normally ask about abortion as it is such a taboo. I do know that unsafe abortion happens though, for example my grandmother tried to end her pregnancy once. She was forty-five years old and had six children already. She did not know any way of not getting pregnant or safely ending the pregnancy. She told me that she drank liquids and jumped from the stairs, taking a great risk. She really didn’t want to be pregnant again and tried hard to end it but it did not work. I am very proud that as a peer educator I have expanded my knowledge on many issues, including how to provide harm reduction information to women so that they can reduce risks of unsafe abortion and not do what my grandmother did in case they don’t want to be pregnant. Once I met with a woman who already had six children, she was tired of having children but her husband wanted to have more so we visited them at home and through conversation, the husband understood the need, so she was able to access an IUD. Here we work a lot with women, we change them, we speak with them, they change their opinions, they become decision-makers and they leave the clinic as different people. Read more stories from SAAF in Palestine

| 02 April 2019
"From my experience the situation in relation to abortion in Palestine is very hard"
Women and girls in Palestine face a number of difficulties and challenges. The ongoing conflict and lack of sitting government as well as high unemployment, has led to poverty and inequality, while an increasingly conservative society and traditionally patriarchal culture has led to increased gender-inequality and lack of access to sexual and reproductive healthcare. The current abortion law unfairly pushes women to risk their lives and health to attempt to end their unwanted pregnancies in unsafe ways. In this context, the Palestinian Family Planning and Protection Agency (PFPPA) has been working since 1964, to provide sexual and reproductive healthcare and advocate for women’s rights. Having received two grants from Safe Abortion Action Fund (SAAF) since 2014, they have been working on the lack of access to safe abortion in the country with a focus on increasing their provision of abortion-related services and advocating at community and national level for changes to the abortion law. My name is Khawla*, I am 42 years old and I am a midwife and university lecturer. I have been married for 10 years and have three children, two boys and a girl. I have multiple health issues and a number of hereditary conditions in my family. I first became involved with PFPPA through my work, having taken many trainings with them about issues such as early marriage, gender-based violence, sexual health and safe abortion. Then last year I accidentally became pregnant myself. My youngest child was just two years old, I had a new job at the time and was suffering with a number of health issues that would make another pregnancy dangerous for me. Unintended pregnancy When I read that the pregnancy test was positive, it was a very hard time. I started crying – I felt like the world was very black – it was the end of my life. I would kill myself, if I didn’t end this pregnancy. So I came to PFPPA and they treated me as a client. I met with the social worker, midwife and doctor and, since the pregnancy was risk to my life and I was very weak and bleeding when I reached them they were able to prescribe the tablets. These pills are highly regulated and restricted here and not all pharmacists stock them but I was able to access them with the prescription and they worked. PFPPA provided follow up afterwards helping me to find an effective long-acting family planning method. Even though I knew about the different methods, they discussed them all with me to ensure that they would be appropriate for my health. Even though the law allows abortion in cases of risks to health of the woman, you need to get permission from the religious leaders and they are very hard to convince. I took my case to them and, despite my health issues, they refused despite it being very early in the pregnancy, before the ensoulment and is allowed according to Islam. The public hospital will not perform it unless they receive the permission from the religious leaders and they don’t give it despite what the religious rules say. Stigma & access From my experience the situation in relation to abortion in Palestine is very hard. There are many women who get pregnant who did not plan it and it’s not the time for the pregnancy. The door is closed to them from the public health system. I have started to campaign on this issue now, I talk to the students in my course about how we can solve this problem. I think the stigma is very difficult. I never thought I would be in this situation, I talked a lot about it before but when you are in the situation, it is totally different. I really appreciated the help given from the PFPPA team, particularly the psychological support. When I felt bad, they helped me to see that I was doing the right thing and it was my right. Read more stories from SAAF in Palestine *Not her real name

| 16 May 2025
"From my experience the situation in relation to abortion in Palestine is very hard"
Women and girls in Palestine face a number of difficulties and challenges. The ongoing conflict and lack of sitting government as well as high unemployment, has led to poverty and inequality, while an increasingly conservative society and traditionally patriarchal culture has led to increased gender-inequality and lack of access to sexual and reproductive healthcare. The current abortion law unfairly pushes women to risk their lives and health to attempt to end their unwanted pregnancies in unsafe ways. In this context, the Palestinian Family Planning and Protection Agency (PFPPA) has been working since 1964, to provide sexual and reproductive healthcare and advocate for women’s rights. Having received two grants from Safe Abortion Action Fund (SAAF) since 2014, they have been working on the lack of access to safe abortion in the country with a focus on increasing their provision of abortion-related services and advocating at community and national level for changes to the abortion law. My name is Khawla*, I am 42 years old and I am a midwife and university lecturer. I have been married for 10 years and have three children, two boys and a girl. I have multiple health issues and a number of hereditary conditions in my family. I first became involved with PFPPA through my work, having taken many trainings with them about issues such as early marriage, gender-based violence, sexual health and safe abortion. Then last year I accidentally became pregnant myself. My youngest child was just two years old, I had a new job at the time and was suffering with a number of health issues that would make another pregnancy dangerous for me. Unintended pregnancy When I read that the pregnancy test was positive, it was a very hard time. I started crying – I felt like the world was very black – it was the end of my life. I would kill myself, if I didn’t end this pregnancy. So I came to PFPPA and they treated me as a client. I met with the social worker, midwife and doctor and, since the pregnancy was risk to my life and I was very weak and bleeding when I reached them they were able to prescribe the tablets. These pills are highly regulated and restricted here and not all pharmacists stock them but I was able to access them with the prescription and they worked. PFPPA provided follow up afterwards helping me to find an effective long-acting family planning method. Even though I knew about the different methods, they discussed them all with me to ensure that they would be appropriate for my health. Even though the law allows abortion in cases of risks to health of the woman, you need to get permission from the religious leaders and they are very hard to convince. I took my case to them and, despite my health issues, they refused despite it being very early in the pregnancy, before the ensoulment and is allowed according to Islam. The public hospital will not perform it unless they receive the permission from the religious leaders and they don’t give it despite what the religious rules say. Stigma & access From my experience the situation in relation to abortion in Palestine is very hard. There are many women who get pregnant who did not plan it and it’s not the time for the pregnancy. The door is closed to them from the public health system. I have started to campaign on this issue now, I talk to the students in my course about how we can solve this problem. I think the stigma is very difficult. I never thought I would be in this situation, I talked a lot about it before but when you are in the situation, it is totally different. I really appreciated the help given from the PFPPA team, particularly the psychological support. When I felt bad, they helped me to see that I was doing the right thing and it was my right. Read more stories from SAAF in Palestine *Not her real name
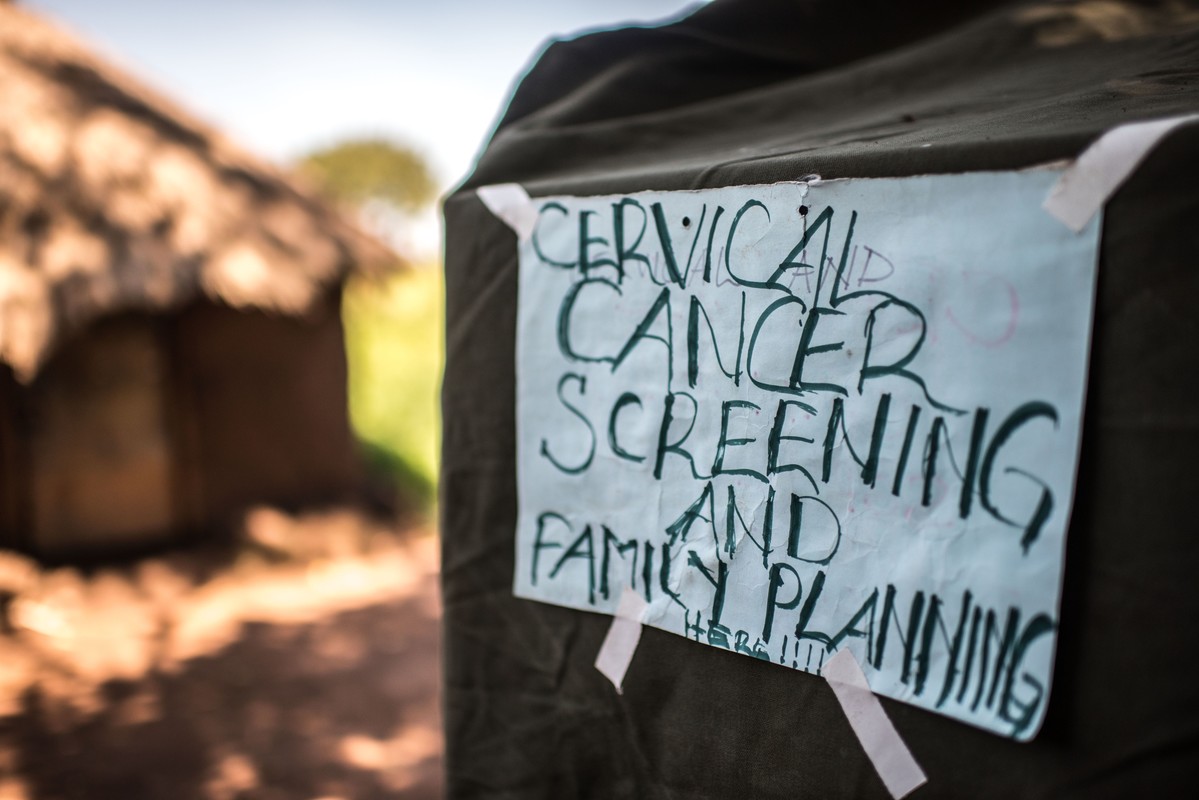
| 22 August 2018
“A radio announcement saved my life” – Gertrude’s story
Gertrude Mugala is a teacher in Fort Portal, a town in Western Uganda. While Gertrude considered herself fairly knowledgeable about cancer, she had never considered taking a screening test or imagined herself ever having the disease. Then one day, she heard an announcement on the radio urging women to go for cervical cancer screenings at a Reproductive Health Uganda (RHU) clinic. “The radio presenter was talking about cervical cancer, and in her message she encouraged all women to get screened. I decided to go and try it out,” she said. Gertrude made her way to RHU's Fort Portal Branch clinic for the free cervical cancer screening. There, she met Ms. Irene Kugonza, an RHU service provider. Ms. Kugonza educated Gertrude and a group of other women about cervical cancer and the importance of routine screening. Gertrude received a type of cervical cancer screening called VIA (visual inspection with acetic acid). "I did not know what was happening" But Gertrude's results were not what she expected; she received a positive result. The good news, however, is that precancerous lesions can be treated if detected early. “I was so shaken when I was told I had pre-cancerous lesions. I did not know what was happening and I didn't believe what I was hearing. I had no idea of my health status. I thought I was healthy, but I was actually harbouring a potential killer disease in me. What would have happened if I didn't go for the screening? If I hadn't heard the radio announcement?” Gertrude was then referred for cryotherapy. “Following cryotherapy, I am now in the process of healing, and I am supposed to go back for review after three months,” said Gertrude. Community screenings Today, Gertrude advocates for cervical cancer screening in her community. She talks to women about cancer, especially cervical cancer, at her workplace, at the market, in meetings, and any other opportunity she gets. “I decided to let women know that cervical cancer is real and it is here with us, and that it kills. At the moment, those are the platforms I have, and I will continue educating women about cancer and encourage them to go for routine testing. I am also happy that I was near my radio that day, where I heard that announcement encouraging all women to get tested for cervical cancer. It might be because of that radio announcement that I am here today,” she said.
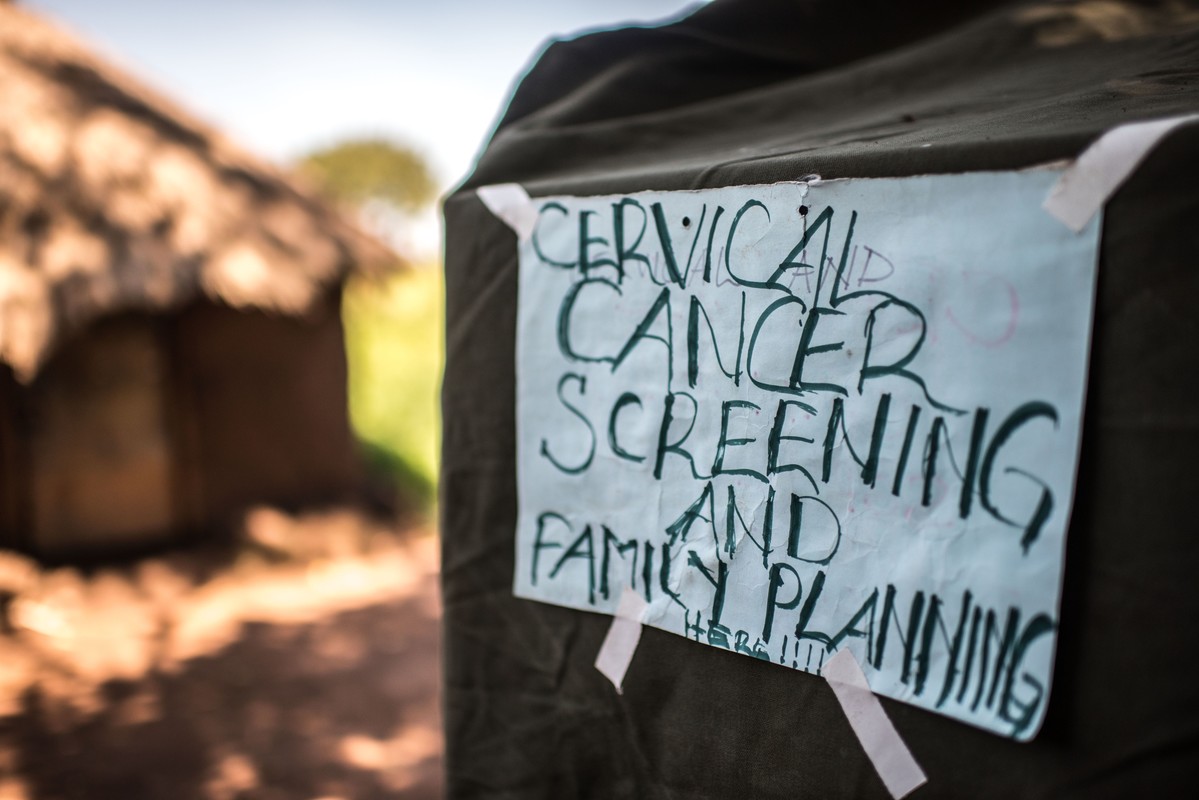
| 16 May 2025
“A radio announcement saved my life” – Gertrude’s story
Gertrude Mugala is a teacher in Fort Portal, a town in Western Uganda. While Gertrude considered herself fairly knowledgeable about cancer, she had never considered taking a screening test or imagined herself ever having the disease. Then one day, she heard an announcement on the radio urging women to go for cervical cancer screenings at a Reproductive Health Uganda (RHU) clinic. “The radio presenter was talking about cervical cancer, and in her message she encouraged all women to get screened. I decided to go and try it out,” she said. Gertrude made her way to RHU's Fort Portal Branch clinic for the free cervical cancer screening. There, she met Ms. Irene Kugonza, an RHU service provider. Ms. Kugonza educated Gertrude and a group of other women about cervical cancer and the importance of routine screening. Gertrude received a type of cervical cancer screening called VIA (visual inspection with acetic acid). "I did not know what was happening" But Gertrude's results were not what she expected; she received a positive result. The good news, however, is that precancerous lesions can be treated if detected early. “I was so shaken when I was told I had pre-cancerous lesions. I did not know what was happening and I didn't believe what I was hearing. I had no idea of my health status. I thought I was healthy, but I was actually harbouring a potential killer disease in me. What would have happened if I didn't go for the screening? If I hadn't heard the radio announcement?” Gertrude was then referred for cryotherapy. “Following cryotherapy, I am now in the process of healing, and I am supposed to go back for review after three months,” said Gertrude. Community screenings Today, Gertrude advocates for cervical cancer screening in her community. She talks to women about cancer, especially cervical cancer, at her workplace, at the market, in meetings, and any other opportunity she gets. “I decided to let women know that cervical cancer is real and it is here with us, and that it kills. At the moment, those are the platforms I have, and I will continue educating women about cancer and encourage them to go for routine testing. I am also happy that I was near my radio that day, where I heard that announcement encouraging all women to get tested for cervical cancer. It might be because of that radio announcement that I am here today,” she said.

| 21 May 2017
A graduate in need turns to sex work
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Lady Mermaid's Bureau. I am Pretty Lynn, aged 25. I am a sex worker but I went to university. I graduated with a Bachelor's Degree in Tourism in 2013. But now, during the day I’m sleeping and during the night I’m working. That is how my day goes every day. I got into sex work through friends. Okay it is not good but I am earning. I tried to get a job when I graduated. I have been applying since I graduated in 2013. I’m still applying but I’m not getting anywhere. You know to get jobs in Uganda; you have to know someone there and no one knows me there. To be a sex worker is like a curse. People look at you like, I don’t know, as someone that has no use in society. People look at you in a bad way. They even don’t consider why you are selling. They just see you as the worst thing that can happen in the society. So it is not comfortable, it is really hard but we try and survive. The fact sex working is illegal means you have to hide yourself when you are selling so that police cannot take you. And then you get diseases, men don’t want to pay. When the police come and take us, sometimes they even use us and don’t pay. So it is really hard. They want a free service. Like if they come and take you and pay that would be fair. But they say it is illegal to sell yourself. But they still use you yet they are saying it is illegal. You can’t report the police because there is no evidence. Abortion and unwanted pregnancies are really common because men don’t want to use condoms and female condoms are really rare and they are expensive. Though at times we get female condoms from Lady Marmaid’s Bureau (LMB) because there are so many of us they can’t keep on giving you them all the time. At times when we get pregnant we use local methods. You can go and use local herbs but it is not safe. One time I used local herbs and I was successful. Then the other time I used Omo washing powder and tea leaves but it was really hard for me. I almost died. I had a friend who died last year from this. But the good thing is that LMB taught us about safe abortion. I have had a safe abortion too. There are some tabs they are called Miso (misoprostol). It costs about fifty thousand shillings (£10 pounds or $20.) It is a lot of money. But if I’m working and I know I’m pregnant, I can say, "this week I’m working for my safe abortion". So if I’m working for twenty thousand, by the end of the week I will have the money. It is expensive compared to Omo at five hundred shillings but that is risky. So if I say I will work this whole week for Miso (misoprostol) it is better. But I'm working and I'm not eating. A project like this one from Lady Mermaid's can help young girls and women. But to take us from sex work, it would really be hard. They would not have enough money to cater for all of us. So what they have to do is to teach us how to protect ourselves, how to defend ourselves. Safe abortion yes. They will just have to sensitise us more about our lives, protection, female condoms and all that. I don't have a boyfriend but maybe when I get money and leave this job I will. But for now, no man would like a woman who sells. No man will bear the wife selling herself. And that will happen only if I get funds, settle somewhere else and become responsible woman. I don’t want this job. I don’t want to be in this business of sex work all the time. I want be married, with my children happily, not selling myself. Stories Read more stories about the amazing success of SAAF in Uganda

| 15 May 2025
A graduate in need turns to sex work
The Safe Abortion Action Fund (SAAF) which is hosted by IPPF was set up in 2006 in order to support grass-roots organisations to increase access to safe abortion. One such organisation which received support under the last round of funding is called Lady Mermaid's Bureau. I am Pretty Lynn, aged 25. I am a sex worker but I went to university. I graduated with a Bachelor's Degree in Tourism in 2013. But now, during the day I’m sleeping and during the night I’m working. That is how my day goes every day. I got into sex work through friends. Okay it is not good but I am earning. I tried to get a job when I graduated. I have been applying since I graduated in 2013. I’m still applying but I’m not getting anywhere. You know to get jobs in Uganda; you have to know someone there and no one knows me there. To be a sex worker is like a curse. People look at you like, I don’t know, as someone that has no use in society. People look at you in a bad way. They even don’t consider why you are selling. They just see you as the worst thing that can happen in the society. So it is not comfortable, it is really hard but we try and survive. The fact sex working is illegal means you have to hide yourself when you are selling so that police cannot take you. And then you get diseases, men don’t want to pay. When the police come and take us, sometimes they even use us and don’t pay. So it is really hard. They want a free service. Like if they come and take you and pay that would be fair. But they say it is illegal to sell yourself. But they still use you yet they are saying it is illegal. You can’t report the police because there is no evidence. Abortion and unwanted pregnancies are really common because men don’t want to use condoms and female condoms are really rare and they are expensive. Though at times we get female condoms from Lady Marmaid’s Bureau (LMB) because there are so many of us they can’t keep on giving you them all the time. At times when we get pregnant we use local methods. You can go and use local herbs but it is not safe. One time I used local herbs and I was successful. Then the other time I used Omo washing powder and tea leaves but it was really hard for me. I almost died. I had a friend who died last year from this. But the good thing is that LMB taught us about safe abortion. I have had a safe abortion too. There are some tabs they are called Miso (misoprostol). It costs about fifty thousand shillings (£10 pounds or $20.) It is a lot of money. But if I’m working and I know I’m pregnant, I can say, "this week I’m working for my safe abortion". So if I’m working for twenty thousand, by the end of the week I will have the money. It is expensive compared to Omo at five hundred shillings but that is risky. So if I say I will work this whole week for Miso (misoprostol) it is better. But I'm working and I'm not eating. A project like this one from Lady Mermaid's can help young girls and women. But to take us from sex work, it would really be hard. They would not have enough money to cater for all of us. So what they have to do is to teach us how to protect ourselves, how to defend ourselves. Safe abortion yes. They will just have to sensitise us more about our lives, protection, female condoms and all that. I don't have a boyfriend but maybe when I get money and leave this job I will. But for now, no man would like a woman who sells. No man will bear the wife selling herself. And that will happen only if I get funds, settle somewhere else and become responsible woman. I don’t want this job. I don’t want to be in this business of sex work all the time. I want be married, with my children happily, not selling myself. Stories Read more stories about the amazing success of SAAF in Uganda

| 15 May 2017
All of the clients, all of the time: Our staff never turn anyone away
At the end of a long day, Anicia, closes the clinic with praise for her colleagues who never turn anyone away. "We open at 8am. From 8am we will be receiving a variety of clients for different services - whether post-abortion care, whether antenatal care - we have to give them all the services. We may end up to 10pm, because we'll never chase our clients, we'll never close the place when we have a client inside. People come when they have no hope. You receive them, and you give them hope by treating them properly and giving them quality services. The client gets better and will never forget you. And follow them up on the phone. "How are you doing?" It's good for us to know that they're doing well. Others even tell us 'The way you handle us, we love it so much'." Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE

| 15 May 2025
All of the clients, all of the time: Our staff never turn anyone away
At the end of a long day, Anicia, closes the clinic with praise for her colleagues who never turn anyone away. "We open at 8am. From 8am we will be receiving a variety of clients for different services - whether post-abortion care, whether antenatal care - we have to give them all the services. We may end up to 10pm, because we'll never chase our clients, we'll never close the place when we have a client inside. People come when they have no hope. You receive them, and you give them hope by treating them properly and giving them quality services. The client gets better and will never forget you. And follow them up on the phone. "How are you doing?" It's good for us to know that they're doing well. Others even tell us 'The way you handle us, we love it so much'." Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE

| 15 May 2017
Getting services to the most remote areas in Uganda
Every Thursday a team from RHU Gulu district provides a mobile outreach clinic in Atega village in the Omoro district in Northern Uganda. The outreach team goes out into this poor, remote area which would otherwise not have access to sexual and reproductive health services. The night before the outreach clinic RHU driver, Robert Nyeko and Godfrey Bedimot load up tents, chairs, medical equipment and supplies. The clinic needs to be set up and by 7am ready to receive clients from 8am. The outreach clinic provides a range of services including diagnosis, testing and treatment, family planning such as fitting implants, providing condoms and HPV vaccines. Laboratory technician, Denis Bongonyinge carries out testing for malaria, Hepatitis B, HIV/AIDS, pneumonia and other infections. Other members of the team provide immunisations and vaccinations. Typically men, women and children start arriving at the clinic by 7:30am. Two volunteers are on hand to direct them to the appropriate place to get the services they need. Some clients need a range of services. At 8am service provider, Anicia Filda, popularly known a 'Mama' in the community is ready with her team to start the day. There are now more than 200 clients waiting to be seen; with more people arriving to join the long queues. The longest queue is for the immunisation and vaccination services. The majority have come for either the Hepatitis B vaccine, which is a big threat in this community. Priority is given to the many young girls lining up for the Human Papilloma Virus (HPV) vaccine. Denis Bongonyinge takes blood samples for rapid tests for malaria, HIV, HPV and a range of other infections. Each client carries an exercise book where Denis records their results which is then taken to the staff giving out prescriptions. 32-year-Robert Otim pushes his bicycle to the outreach clinic. The single father has ridden 10 kilometres with his two young children. He lost his wife to Hepatitis B when their daughter was just six months. His four-year-old son was born prematurely and is now disabled. He has come today for his last Hepatitis B immunisation. His children need to be vaccinated as well as treated for malaria and coughs. Looking at the long queue, he says he doubts whether he will get the service today but he is lucky as one of the team who once treated his son, Geoffrey, notices Robert and they are given priority for treatment and prescriptions. Already by midday, one of the teams delivering minor surgeries, postnatal services, family planning and post abortion care have seen 47 mothers. This is almost the same as the number of clients they would treat at the Gulu Clinic during a normal day. Anicia Filda sends the driver to collect more supplies from the clinic; the stock is starting to run low because demand is so high There is no break for the team. Samuel Kedi, the only clinician at the outreach camp stands up, and picks up a bottle of water from his backpack for a quick drink before continuing with the next client. The clinic continues to see clients well into the evening. The outreach clinic is scheduled to finish by 5pm but Anicia says there is not one day they have closed on time: “We cannot close when clients are still lining up. It’s the same at the clinic in Gulu,” she says. As the clinic draws to a close for the day, the teams complete their report which records details of the numbers clients served, the types of services delivered and supplies of stock. It has been another busy but successful day for Anicia and her team. Provision of integrated services in such remote areas is vital for the local community; many men, women and children would not be able to receive the types of treatment and care that RHU works diligently to provide. Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE

| 16 May 2025
Getting services to the most remote areas in Uganda
Every Thursday a team from RHU Gulu district provides a mobile outreach clinic in Atega village in the Omoro district in Northern Uganda. The outreach team goes out into this poor, remote area which would otherwise not have access to sexual and reproductive health services. The night before the outreach clinic RHU driver, Robert Nyeko and Godfrey Bedimot load up tents, chairs, medical equipment and supplies. The clinic needs to be set up and by 7am ready to receive clients from 8am. The outreach clinic provides a range of services including diagnosis, testing and treatment, family planning such as fitting implants, providing condoms and HPV vaccines. Laboratory technician, Denis Bongonyinge carries out testing for malaria, Hepatitis B, HIV/AIDS, pneumonia and other infections. Other members of the team provide immunisations and vaccinations. Typically men, women and children start arriving at the clinic by 7:30am. Two volunteers are on hand to direct them to the appropriate place to get the services they need. Some clients need a range of services. At 8am service provider, Anicia Filda, popularly known a 'Mama' in the community is ready with her team to start the day. There are now more than 200 clients waiting to be seen; with more people arriving to join the long queues. The longest queue is for the immunisation and vaccination services. The majority have come for either the Hepatitis B vaccine, which is a big threat in this community. Priority is given to the many young girls lining up for the Human Papilloma Virus (HPV) vaccine. Denis Bongonyinge takes blood samples for rapid tests for malaria, HIV, HPV and a range of other infections. Each client carries an exercise book where Denis records their results which is then taken to the staff giving out prescriptions. 32-year-Robert Otim pushes his bicycle to the outreach clinic. The single father has ridden 10 kilometres with his two young children. He lost his wife to Hepatitis B when their daughter was just six months. His four-year-old son was born prematurely and is now disabled. He has come today for his last Hepatitis B immunisation. His children need to be vaccinated as well as treated for malaria and coughs. Looking at the long queue, he says he doubts whether he will get the service today but he is lucky as one of the team who once treated his son, Geoffrey, notices Robert and they are given priority for treatment and prescriptions. Already by midday, one of the teams delivering minor surgeries, postnatal services, family planning and post abortion care have seen 47 mothers. This is almost the same as the number of clients they would treat at the Gulu Clinic during a normal day. Anicia Filda sends the driver to collect more supplies from the clinic; the stock is starting to run low because demand is so high There is no break for the team. Samuel Kedi, the only clinician at the outreach camp stands up, and picks up a bottle of water from his backpack for a quick drink before continuing with the next client. The clinic continues to see clients well into the evening. The outreach clinic is scheduled to finish by 5pm but Anicia says there is not one day they have closed on time: “We cannot close when clients are still lining up. It’s the same at the clinic in Gulu,” she says. As the clinic draws to a close for the day, the teams complete their report which records details of the numbers clients served, the types of services delivered and supplies of stock. It has been another busy but successful day for Anicia and her team. Provision of integrated services in such remote areas is vital for the local community; many men, women and children would not be able to receive the types of treatment and care that RHU works diligently to provide. Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE

| 15 May 2017
Joyce's story - empowering disabled clients with services in rural communities
Joyce Auma, 25, is a business administration graduate currently working as a data clerk with Gulu Women with Disabilities Union. The union has partnered with Reproductive Health Uganda to extend sexual and reproductive health services to women living with disabilities in Gulu and neighbouring districts in Acholi. Joyce, who lost the use of her legs in childhood, is one of the women with disabilities that normally receive services at Gulu Clinic. “I found out about RHU because they are our partners at Gulu Women with Disability Union. I first came to the clinic to test for HIV and other STIs. We also receive their other services like family planning and cancer screening to people with disabilities.” “The first time I came here I was warmly welcomed. They're very good at talking to the youth. Though the place was new for me, I was given service as if it was not my first time.” Says Joyce. "Us people with disabilities have challenges at the main hospitals. People around look at you as if you are not a human being and you don’t fall sick.” Joyce has since been a regular client of RHU for HIV testing, cancer screening and other diseases. She says her status exposes her to many risks of infection which has to be regularly checked for. “I always come here for testing, there is also cancer screening. They don’t segregate me because of my disability. They give you the services you need.” Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE

| 16 May 2025
Joyce's story - empowering disabled clients with services in rural communities
Joyce Auma, 25, is a business administration graduate currently working as a data clerk with Gulu Women with Disabilities Union. The union has partnered with Reproductive Health Uganda to extend sexual and reproductive health services to women living with disabilities in Gulu and neighbouring districts in Acholi. Joyce, who lost the use of her legs in childhood, is one of the women with disabilities that normally receive services at Gulu Clinic. “I found out about RHU because they are our partners at Gulu Women with Disability Union. I first came to the clinic to test for HIV and other STIs. We also receive their other services like family planning and cancer screening to people with disabilities.” “The first time I came here I was warmly welcomed. They're very good at talking to the youth. Though the place was new for me, I was given service as if it was not my first time.” Says Joyce. "Us people with disabilities have challenges at the main hospitals. People around look at you as if you are not a human being and you don’t fall sick.” Joyce has since been a regular client of RHU for HIV testing, cancer screening and other diseases. She says her status exposes her to many risks of infection which has to be regularly checked for. “I always come here for testing, there is also cancer screening. They don’t segregate me because of my disability. They give you the services you need.” Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE

| 15 May 2017
Breaking gender taboos
After two years of struggling to conceive Brenda Abalo and her husband, Francis Opio, decided to visit Reproductive Health Uganda's clinic in Gulu. Much as there is progressive attitude to modern medicine in this northern Uganda region, fertility treatment remains a sensitive issue for both men and women. Anxious in the waiting room, Francis said he had decided to come to RHU with his wife because he heard their radio show about a similar problem. In addition to fertility treatments, the couple was also given counselling and treatment for another condition. “After sex, my wife was in pain. She was complaining a lot three weeks ago. I also felt some itches. They have given us treatment which we are still continuing with,” said Francis. The couple was given information to ensure that Brenda was in the best possible health to conceive. She is to undergo treatment to reduce the prolactin level in the blood and correct the hormonal imbalance. “This is not my first time at this clinic," says Brenda. “The service here is better in comparison with other health centres. They give much better attention to the patient.” “RHU has been supporting a lot of people. They helped a friend of mine; she was having a problem with miscarriage. So she came here and got properly treated” Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE

| 16 May 2025
Breaking gender taboos
After two years of struggling to conceive Brenda Abalo and her husband, Francis Opio, decided to visit Reproductive Health Uganda's clinic in Gulu. Much as there is progressive attitude to modern medicine in this northern Uganda region, fertility treatment remains a sensitive issue for both men and women. Anxious in the waiting room, Francis said he had decided to come to RHU with his wife because he heard their radio show about a similar problem. In addition to fertility treatments, the couple was also given counselling and treatment for another condition. “After sex, my wife was in pain. She was complaining a lot three weeks ago. I also felt some itches. They have given us treatment which we are still continuing with,” said Francis. The couple was given information to ensure that Brenda was in the best possible health to conceive. She is to undergo treatment to reduce the prolactin level in the blood and correct the hormonal imbalance. “This is not my first time at this clinic," says Brenda. “The service here is better in comparison with other health centres. They give much better attention to the patient.” “RHU has been supporting a lot of people. They helped a friend of mine; she was having a problem with miscarriage. So she came here and got properly treated” Follow a day in the life of our team and clients in Gulu, Uganda 07:00 08:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 22:00 Prev Next 7am: The team prepare for the long day ahead "Every year tens of thousands of Ugandans come to our clinic. Everyone is welcome. Here are just a few of the people that we served in one day last month." READ MORE 8am: Nancy, 19, becomes a volunteer "I was suffering but when I came here, I was treated and I got better. Now I'm inspired to volunteer here" READ MORE 9am: Monica, 25, a sex worker's story "I am sex working. I came here for Hepatitis B testing and also counselling. I have so many personal problems, but here….they’re so caring." READ MORE 10am: Jane, 23, saved by family planning "After multiple miscarriages, family planning here has helped me a lot. I'm glad we've been able to space the number of children we've had. I am not growing old, I am fresh." READ MORE 11am: Vicky, handling disabilities "I'm deaf so accessing services is hard, but here they really try to speak in sign language." READ MORE 12pm: Dorcus, first time patient "This is the first time I've ever come here, I like the service. They give good counselling so I recommend coming." READ MORE 1pm: Christine, 45, a grandmother's tale of living with HIV "I am living with HIV and had HPV. They treated me and now I'm free of cervical cancer." READ MORE 2pm: Lilian, struggling mother of six with sickle cell " I have sickle cell disease and so do all my children. I want to have my tube removed so that I don't get pregnant again but I don't know if my husband will allow it." READ MORE 3pm: Brenda and Francis get fertility treatments "Fertility treatment is a sensitive issue in Uganda but they help us a lot and we get proper treatment." READ MORE 4pm: Joyce, 25, repected regardless of her disability "I realised that at this place they don't segregate. Us people with disabilities have challenges at the main hospitals. You go there, people around look at you as if you are not a human being and you don't fall sick." READ MORE 5pm: Mobile clinic provides outreach services to remote villages "Our outreach to remote communities is a 'one-stop-centre'. We give family planning, vaccines for HPV, malaria, and Hepatitis B, HIV testing and more." READ MORE 22pm: Still giving the last client our very best "Together, we have great teamwork. Sometimes we're still working up to 10pm because we never chase out our clients. We’ll never close the place when we have a client inside. People come when they have no hope." READ MORE